Introduction
Cubital tunnel syndrome (CTS), characterized by the entrapment of the ulnar nerve at the elbow, is a prevalent condition causing symptoms that include but are not limited to pain, numbness, and muscle weakness in the affected limb. It often results in sensory disturbances and motor deficits, significantly affecting patients’ daily activities and livelihood. The diagnosis of CTS relies on a thorough understanding of the ulnar nerve and its sensory and motor branch distribution. However, the clinical identification of ulnar nerve pathology is often complex due to anatomical variations, a wide array of differential diagnoses, and diverse clinical presentations. Untreated or inadequately managed injury to the ulnar nerve may lead to severe complications, including persistent sensory impairments, muscle weakness, and joint contractures.1 Therefore, early and accurate diagnosis is crucial for effective management and rehabilitation. Electromyography (EMG) and nerve conduction studies (NCS) have traditionally been the mainstay in the diagnosis of ulnar nerve pathology. While effective, they also have limitations including cost, accessibility, and patient discomfort. MSK-US imaging is emerging as a valuable diagnostic tool, particularly in cases where the diagnosis of ulnar nerve pathology is uncertain.2 The integration of MSK-US imaging into the diagnostic process offers clinicians a real-time, dynamic approach to correlate imaging findings with clinical symptoms directly. This article aims to provide an in-depth exploration of the application of ultrasound imaging in the diagnosis of ulnar neuropathy at the elbow, underscoring its significance as a non-invasive, real-time, and highly informative diagnostic modality.
Epidemiology, Risk Factors, and Pathophysiology
Ulnar neuropathy at the elbow is a condition with diverse etiologies and mechanisms of injury. The ulnar nerve is vulnerable to compression at several anatomical locations in the vicinity of the elbow, predominantly at the ulnar groove and beneath the humeroulnar aponeurotic arcade.2 However, entrapment can also occur at various other points, including the medial intermuscular septum of the arm, the arcade of Struthers, the cubital tunnel, and between the flexor carpi ulnaris (FCU) and flexor digitorum superficialis (FDS) muscles.2
Ulnar neuropathy at the elbow is estimated to affect up to 5.9% of the general population, as highlighted in recent studies.3,4 Research has identified several risk factors associated with the development of ulnar neuropathy. A significant correlation has been observed between smoking and the onset of ulnar neuropathy, as indicated by epidemiological data.4 Furthermore, demographic factors such as advancing age and male sex have been identified as potential risk factors for the development of ulnar neuropathy.5 Occupational factors, particularly hand-arm vibration exposure in specific jobs, have also been implicated in ulnar neuropathy development.6
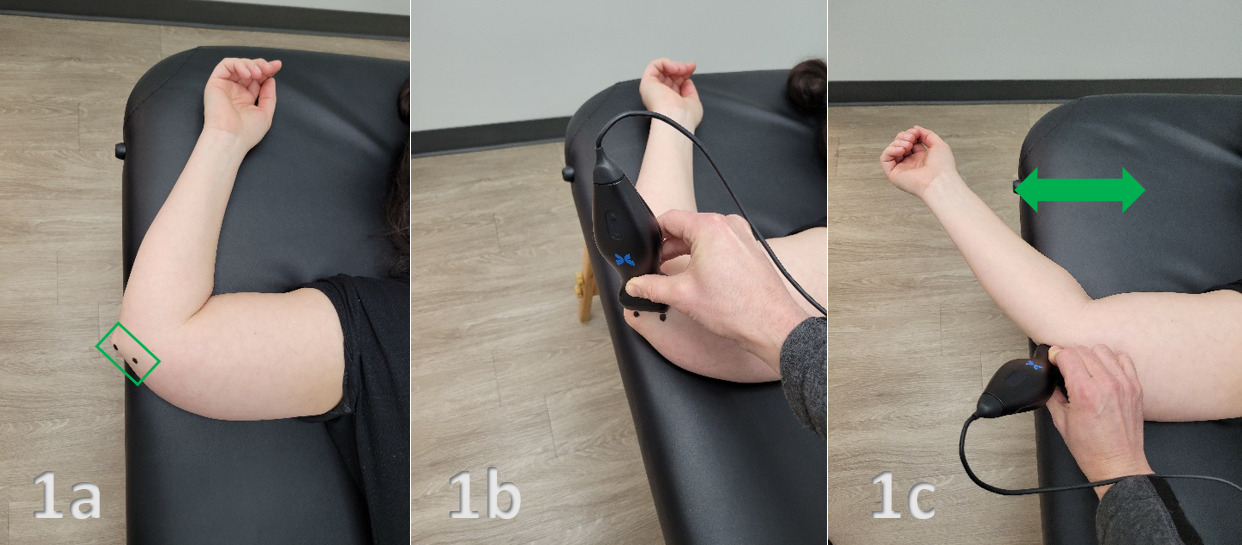
The pathophysiological mechanisms underlying dynamic ulnar nerve compression at the elbow are not entirely known. An intriguing aspect is the congenital absence of the ulnar groove retinaculum, potentially accounting for increased ulnar nerve mobility outside the ulnar groove upon elbow flexion.7 Additionally, a shallow bony ulnar groove might contribute to instability.8 Although ulnar nerve instability is frequently observed in asymptomatic individuals, its exact relationship to symptomatic presentations remains ambiguous.9 Notably, while often asymptomatic, ulnar nerve instability can be implicated in pain syndromes due to friction and increased pressure.
Furthermore, the hypermobility of the ulnar nerve, particularly during flexion, renders it susceptible to damage from direct trauma or pressure.2 The notion of “frictional neuritis” suggests that the subluxing or dislocating ulnar nerve may become irritated against bony irregularities, particularly in arthritic or post-traumatic joints.10 Additionally, it has been proposed that complete ulnar nerve dislocation might paradoxically act as a protective mechanism against nerve strain.11
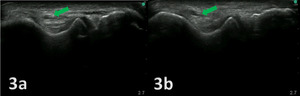
Diagnosis and Ultrasound Scanning Techniques
The diagnosis of ulnar neuropathy at the elbow is a multifaceted process that hinges on a comprehensive patient history, physical examination, electrophysiological testing, and MSK-US examination. Clinical manifestations of ulnar nerve entrapment typically include medial elbow pain, tingling, and numbness in the area supplied by the ulnar nerve, primarily affecting the fourth and fifth digits. These symptoms are often exacerbated by elbow flexion, such as during phone use, leaning on an elbow, or sleeping with the elbow bent beyond 90 degrees.2 Difficulties in fine motor tasks, such as typing or opening bottles, are also reported, although overt motor symptoms like muscle atrophy or weakness may not be initially present.
Diagnostic provocative tests, including the Tinel test at the ulnar groove and the elbow flexion test with wrist extension, are valuable in confirming ulnar nerve entrapment. Enhancing these tests with additional shoulder internal rotation can improve their sensitivity and specificity.12 Impairment in two-point discrimination in the ring and small fingers may also be present. Clinical examination may reveal the snapping of the dislocating ulnar nerve beneath the fingertips anterior to the medial epicondyle during elbow flexion.
Electrodiagnostic testing, including motor and sensory nerve conduction studies and needle examination, plays a crucial role in diagnosing ulnar nerve entrapment, pinpointing the site of entrapment, and determining the severity of the condition.13 Despite their utility, electrodiagnostic studies have limitations in visualizing the morphology of the ulnar nerve and its surrounding tissues. Imaging examinations, like MSK-US or magnetic resonance imaging (MRI), become indispensable, especially in cases with ambiguous diagnoses or secondary causes of compression.14
Technical Aspects
MSK-US involves the use of high-frequency sound waves to create detailed images of muscles, ligaments, nerves, and other soft tissues. Its high resolution allows for the visualization of the ulnar nerve and its surrounding structures with exceptional clarity. MSK-US offers several advantages over traditional diagnostic methods:
-
Dynamic Imaging: MSK-US enables the observation of the ulnar nerve in motion, helping to identify pathological changes during different arm positions.
-
Accessibility and Cost-effectiveness: Compared to MRI, MSK-US is more accessible and cost-effective, making it a practical choice in various clinical settings.
-
Patient Comfort: Being non-invasive and painless, MSK-US enhances patient comfort and compliance.
-
Immediate Feedback: Real-time imaging allows for immediate evaluation and diagnosis, facilitating quicker decision-making in treatment planning.
Conclusion
MSK-US is a valuable tool in the evaluation of CTS and ulnar nerve pathology. Its non-invasive nature, coupled with the ability to provide dynamic and detailed visualization of the nerve, makes it an excellent adjunct to clinical examination and traditional nerve conduction studies. The integration of MSK-US aids in the early detection of ulnar nerve pathologies, which is crucial for timely intervention and preventing progression to chronic stages. Rehabilitation providers, equipped with knowledge and skills in MSK-US, can significantly enhance their diagnostic and therapeutic approach to ulnar nerve pathology, ultimately improving patient outcomes.

.png)
.png)
