INTRODUCTION
Hip and groin pain is a common issue in elite hockey,1,2 with approximately 50% of professional European hockey athletes reporting a hip or groin problem during a competitive season.3 Furthermore, during the 2014-15 to the 2018-19 collegiate hockey seasons, injuries to the hip and groin constituted the body region with the highest proportion (~20%) of injuries sustained during practice.4 However, it is important to note that the majority of these (~50-60%) do not cause time-loss from training or competition.5,6 Nonetheless, on-going hip and groin pain can have debilitating long-term effects, such as increased dependency on medication, higher surgical intervention rates, and potentially early retirement.7–9 While hockey athletes can still participate in training and competition, their performance capacity is likely to be reduced.1,3 This diminished performance capacity can negatively impact their ability to showcase their skills to coaches and scouts, which may limit playing time and reduce their chances of being selected for higher competitive levels.
To address the high prevalence of hip and groin pain in hockey athletes, it is crucial to gain a deeper understanding of the underlying pathologies and injury mechanisms that may contribute to the development of such pathologies. The most common hip pathologies observed in elite hockey athletes include: femoroacetabular impingement (FAI), injuries to the non-contractile tissues including the labrum, iliofemoral ligament (IFL), and ligamentum teres (LT), as well as muscular injuries, such as core muscle injuries (CMI), hip flexor, and adductor injuries. Increased knowledge of the functional links between these pathologies, pain, and the biomechanics of key hockey activities will allow practitioners to develop evidence-informed monitoring strategies and training interventions aimed at reducing the likelihood or severity of these. Together, this may improve the athletes’ performance potential and overall well-being. Therefore, the purpose of this clinical commentary was to examine current evidence on common hip pathologies in hockey athletes, exploring potential associations between hip and groin pain and the biomechanics of hockey activities.
Femoroacetabular Impingement
FAI is often considered a primary cause of hip and groin pain in hockey athletes and may contribute to the development of other hip and groin injuries.10 It is clinically characterized by symptoms of pain, clicking, catching and stiffness, as well as signs of limited hip range-of-motion (ROM), a positive impingement test, and radiographic evidence of cam or pincer morphology.11,12 Concerningly, Lerebours et al.13 identified that approximately 70% of elite hockey athletes fit the criteria for cam morphology. In addition, these athletes are reported to display significantly lower hip internal rotation (IR), external rotation (ER), total rotation, and flexion ROM, which can cause compensatory movement patterns during key activities including skating, shooting, and passing.12–15 While there is evidence that the presence of cam morphology does not impact on-ice skating performance, such compensatory movements may alter the mechanics of the hip, thereby changing the mechanical forces experienced in this region and increasing the opportunity for future hip and groin injuries.16–18
Skating Mechanics and Development of Femoroacetabular Impingement
The exact mechanism for the development of FAI in athletes, and particularly hockey athletes, is yet to be fully understood. However, the most commonly proposed theory for the cause of cam morphologies in hockey athletes is the abutment of the femoral neck on the anterior aspect of the acetabular rim during the unique skating mechanics.13,19,20 Research investigating potential causes of hip impingement has demonstrated that positions of end-range hip flexion, adduction and IR are needed to induce contact between the femoral neck and acetabular rim, which are the combination of joint actions required during the stance and recovery phases of a skating stride (Figure 1).19,21,22 Specifically, Bedi et al.23 used computerized tomography scans to model dynamic hip impingement in 18 symptomatic FAI patients. It was identified that anterior impingement occurred in both a position of 85° of hip flexion with 15° of hip IR, as well as a position of 85° of hip flexion, with 5° of IR and 20° of hip adduction. Similarly, Han et al.24 utilized cadaver models and determined that the greatest anterior impingement occurred at 120° of hip flexion with maximal adduction and IR. However, current evidence suggests that typical skating mechanics may not necessarily achieve these joint angle combinations required to induce substantial impingement, and therefore, the development of FAI.
During a sprint skating start, it was identified that adolescent hockey athletes reached a maximum position of 44° of hip flexion, with concurrent IR of approximately 6° during the swing phase of a stride.19 Similarly, Renaud et al.21 reported that during the first two strides of a start, high-caliber skaters achieved joint angle positions of approximately 65-76° of hip flexion, with 5-16° of ER and 17-33° of hip abduction. Whereas, in the weight acceptance phase of steady state skating, the positions have been recorded as approximately 40-47° of hip flexion, with neutral hip abduction and slight ER.22,25 Although differences in acetabular and femoral version can lead to abutment within lesser hip joint angles,26 it is likely that only a small percentage of hockey athletes deviate substantially from the typical presentation for hip anatomy, compared to the high prevalence of FAI in this population.13 Based on these concurrent hip positions during sprint starts and steady state strides, it appears unlikely that hockey athletes are reaching the positions required for femoral neck abutment on the acetabulum during forward skating. However, it is important to note that current research has only investigated the mechanics of forward skating, with further research required to better understand the hip joint actions and angles of other skating movements such as crossovers, tight turns, backward skating, and open hip maneuvers, which may achieve such positions.
Cam Morphology and Early Sport Specialization (ESS)
Early sport specialization (ESS) is defined as intentionally focusing on a single sport for more than eight months of the year before the age of 12.27 Interestingly, there is limited evidence suggesting that ESS increases the likelihood of successful performance pathway progression in hockey.28 However, recent authors have suggested that it may have detrimental effects on an adolescent athlete’s hip health, potentially increasing the risk of cam morphology and FAI.27 Specifically, there is evidence suggesting that cam morphology often begins during periods of accelerated growth in early adolescence, particularly in hockey athletes.2,29 During adolescent growth spurts, and especially in males, the repetitive joint loading from intense sports activities evokes an increase in growth hormone, which leads to the proliferation and differentiation of chondrocytes into bone cells, making the epiphyseal plate more susceptible to adaptive changes.30 For example, Laor et al.31 identified that adolescent athletes with overuse knee injuries exhibited widening of the distal femur, and proximal tibia and fibula epiphyseal plates. This plate widening was attributed to hypertrophic chondrocytes extending into the metaphysis, which was likely caused by a disruption in blood supply from the repetitive trauma. Similarly, numerous authors have observed hypertrophic increases in femoral neck cartilage in adolescent athletes, which preceded epiphyseal extension and the development of a cam morphology.32,33
The activity level of adolescent athletes (12 to 14 years old) has been reported as a stepwise relationship with the magnitude of epiphyseal extension and alpha angle increase. For instance, it has been observed that adolescents who participated in organized sport more than three days per week or more than 12.5 hours per week, doubled their risk of developing a cam morphology.16,33 When considering the recent trend in adolescent hockey of a substantially increased proportion of ESS, and hence, greater on-ice practice time, it appears that this may help explain the high prevalence of cam morphologies observed in elite hockey athletes.34,35 Specifically, there are large-magnitude repetitive shear stresses applied to the proximal femur during skating, which the femoral cartilage has a low resistance to.36,37 This can lead to a disruption in blood supply and an increase in epiphyseal plate hypertrophy, particularly in a skeletally immature hip.36 The result is an altered epiphyseal plate shape, and eventually the formation of a callus, representing the presence of a cam morphology. Taken together, the evidence suggests it is not the specific mechanics of forward skating that likely explain the high prevalence of FAI in hockey athletes, but rather potentially the repetitive shear stress applied to the femoral head, particularly during load sensitive periods in adolescence.37
To reduce the likelihood of early FAI, the adolescent hockey athlete should participate in a variety of physical activities, undertake appropriately designed resistance training programs, and have their workload monitored effectively during the reported high-risk phase of 12 to 14 years of age. Such strategies may help reduce the prevalence, or at least delay the development and severity of cam morphology in these athletes by ensuring that a wider variety of loading patterns and stimuli are applied to the femoral head, with adequate rest provided from repetitive stresses. However, despite the high prevalence of cam morphology in elite hockey athletes, several authors have shown limited associations between cam morphology and hip and groin pain, which is a significant performance limiter.35,38 This suggests that cam morphology may not be a direct cause of pain in hockey athletes. Rather, there are various concomitant intra-articular and extra-articular hip pathologies observed in hockey athletes alongside cam morphology, providing a potential explanation of this pain and indicating an indirect relationship. These pathologies include labral, IFL, and LT tears, CMI, and hip flexor and adductor injuries.35
Non-Contractile Tissue Pathology
Intra-articular injuries accounted for 10.6% of all hip and groin injuries in the NHL over four seasons (2006-2010).35 Furthermore, hip labrum tears have been identified in 56-69% of elite hockey athletes,35,38 while LT tears have been reported in 26 out of 28 (~93%) professional hockey athletes’ hips in one study.2 These structures, along with the IFL, have of a large distribution of nociceptors, which elicit a pain response if damaged.39 Furthermore, these non-contractile tissues also play an integral role as passive hip stabilizers, which serve to increase hip joint stability and reduce femoral head translation.40 Given the high incidence of both hip and groin pain in hockey athletes and the presence of non-contractile tissue pathology on imaging, it is possible that the majority of hockey athletes’ hip and groin pain is initiated by an intra-articular hip injury.35 This may also elicit a type of hip microinstability that can increase the opportunity of further hip and groin injuries, and therefore, additional pain.41
Repetitive Skating Mechanics and Intra-Articular Hip Injuries
The hip positions reported to cause the greatest magnitude of compressive and shearing forces on the labrum are positions of: approximately 60° of hip flexion with slight IR, a combined position of hip ER and extension, and hip abduction at an angle of 40° or greater.21,25,42–45 These all increase labral tissue deformation and can result in damage to this structure and other non-contractile tissues through acute or overuse mechanisms.21 Importantly, during the push-off phase of the skating stride, hip extension, abduction and ER are combined to generate forward propulsion, whereas during stride recovery the combination of hip flexion, adduction and IR is required.19,21,22,25 Therefore, forward skating mechanics likely explain the high prevalence of hip labrum injuries.
Hip labrum tears in hockey athletes typically occur in the antero-superior region.35,46 In this region, the anterior fibers of the labrum attach parallel to the bony acetabulum, making them less resistant to shearing forces and more susceptible to injury.47,48 Importantly, the presence of femoral head asphericity, as observed with cam morphology, further reduces the resistance of these fibers to the shearing forces.40,47 As such, the incidence and location of labrum tears in hockey athletes’ hips are likely preceded by the development of a cam morphology, which in combination with the repetitive skating mechanics, can lead to delamination of the labrum from the acetabulum in the antero-superior region.46
The IFL is recognized as the strongest of the three capsular ligaments, and in combination with the labrum provides substantial passive stability to the hip, particularly in limiting excessive hip extension and ER.49 As described above, the cyclical loading pattern during the push-off and recovery phases of the skating stride will likely induce stress-relaxation of the labrum, potentially leading to a labrum tear.46 This subsequently increases the reliance on the IFL and LT to provide passive stabilization of the hip, which may eventually result in fatigue-failure of these tissues too.21,27,50 The data of Johanssen et al.51 supports this suggestion, as it was observed that repetitive hip extension combined with ER induced substantial IFL tissue creep, which is the progressive lengthening of soft tissue that has been subjected to constant load. If these loads are sustained over a long duration of time with minimal recovery (or unloaded) durations, the elastic behavior of the tissues can be reduced, resulting in viscous-like behaviors, and hence, more permanent lengthening.49 Considering the substantial on-ice training durations and cyclical loading patterns of skating, tissue creep of these crucial non-contractile tissues appears likely, particularly in the hockey athlete with a labral injury.
The combination of a labrum tear and IFL lengthening is reported to allow for significantly greater femoral head translation (~2mm), compared to one of these injuries in isolation.49,51 Recent research by Kalisvaart et al.52 defined this increase in femoral head translation relative to the acetabulum as hip microinstability and noted that it is associated with eventual damage of each of the labrum, cartilage, and capsular structures. Therefore, a hockey athlete with a labrum tear and IFL lengthening, is likely to experience an increase in femoral head translation during skating, which will subsequently increase the strain on the capsule and LT. This may lead to failure of the LT as a secondary restraint on femoral head motion, further exacerbating the potential magnitude of femoral head translation during these movements and increasing the opportunity of osteochondral damage and perception of pain.53,54 Together, this evidence suggests that a hockey athlete with cam morphology is likely to exhibit an increased risk of a labrum tear due to the repetitive forward skating mechanics combined with femoral head asphericity. If a labrum tear occurs, there will be an increased reliance on the IFL, LT and capsule to provide passive stabilization to the hip, thereby increasing the strain on and risk of subsequent failure of these tissues.40
Femoral Head Translation and Pain
While potential relationships between hip microinstability and pain are still not understood, there is evidence suggesting a potential connection.52 As the anterior labrum, IFL and LT contain a large distribution of mechanoreceptors and nociceptors, they are crucial structures for hip joint proprioception and stability, and also highly efficient in transmitting pain signals to the central nervous system (CNS).39,54 Therefore, damage to the labrum, and potential IFL and LT lengthening, will likely compromise the feedback loop to the CNS, resulting in poor hip joint proprioception, reduced passive and active stability and exacerbated femoral head translation. Together, this will likely increase tissue irritation, inflammation, and pain in the labrum, IFL and LT, as well as potential osteochondral damage.54 Importantly, it has been identified that bony hip deformities, joint capsule laxity, and muscle dysfunction or imbalance are likely to exacerbate the strain on the anterior hip joint.41,55 As such, a large proportion of hip and groin pain experienced by hockey athletes may be due to a constant cycle of poor mechanoreceptor feedback from a torn labrum, lengthened IFL or LT, and inadequate feedforward adjustments from the stabilizing muscles of the hip, resulting from hip microinstability.
Panjabi’s model of joint stability emphasizes the interplay between the passive, neural, and active sub-systems to optimize joint stability.56 Consequently, deficits in the labrum and ligamentous tissues (passive sub-system) will result in joint instability. However, the inherent protective mechanism of the body is to compensate with the neural and active sub-systems, by way of muscle guarding.49 This guarding can effectively limit excessive femoral head movement and improve overall joint stability, yet the increased muscle activation and tension may result in greater muscular imbalances and tightness around the hip.49,57 The presence of hip microinstability has been reported to cause joint capsule thickening, and importantly, such an increase in anterior hip capsule thickness has been associated with significantly reduced hip flexion and IR ROM in patients with FAI.58,59 Together, this highlights that microinstability of the hip joint appears to evoke a protective mechanism, whereby the muscular and capsular structures respond with adaptations that may further limit hip ROM in a variety of joint actions. While the concept of hip microinstability in hockey athletes is not commonly discussed, practitioners working with these athletes should consider the use of targeted exercise interventions aimed at restoring or improving hip joint ROM and reducing muscular strength imbalances or joint action-specific weakness when they are identified. Specifically, interventions targeting the strength and coordinated co-contraction of the “hip rotator cuff” (deep hip rotators, gluteus medius, gluteus minimus), as well as the iliopsoas and piriformis are believed to increase joint compression and joint stability. Additionally, it is crucial that any inert tissue pathology is appropriately reviewed and treated.
Muscular Injuries
Patients with hip and groin pain often display reduced hip strength, changes in muscle activation patterns, and decreased muscle cross-sectional area.12,57,60–62 These adaptations will likely further reduce hip joint stability and may increase the risk of hip and groin injuries, particularly during movements that exert high stresses on the lumbopelvic complex. This reduced potential of the musculoskeletal system to withstand load is particularly relevant for multi-directional sport athletes, where repetitive changes-of-direction and forceful accelerations and decelerations can strain the lumbopelvic complex and lead to sports-related groin pain (SRGP).63 In addition to the multi-directional nature, the mechanics of shooting and forward sprint skating appear to be significant contributors to the development of three highly prevalent muscular injuries of the lumbopelvic region in hockey: CMI, and hip flexor and adductor injuries. These injuries, with a combined annual prevalence of approximately 20 injuries per 100 elite hockey athletes, can result in significant time-loss from training and competition.64
It is important to recognize that hip and groin pain can result from both pelvic-related or intra-articular hip injuries, and assessments such as the resisted adduction sit-up test have been reported effective in differentiating these pathologies.65 Crucially, pelvic-related injuries can result in uneven contractile abilities between the adductor and lower abdominal muscles, increasing the risk of further soft tissue damage. Conversely, the restricted hip ROM and reduced strength associated with intra-articular injuries, will likely lead to compensatory movements during key hockey activities. Regardless of the underlying pathology, both are likely to significantly alter the mechanics in the lumbopelvic region of the hockey athlete, further increasing the strain on the musculoskeletal system and increasing the risk of these highly prevalent extra-articular hip injuries.
Core Muscle Injuries and Skating and Shooting Mechanics
CMI, characterized by the presence of pain to the groin and lower abdominal regions, are considered overuse injuries resulting from repetitive, high-force rotational movements around the lumbopelvic region, particularly when such activities occur over a fixed lower extremity.66–68 The pubic symphysis acts as a fulcrum for the forces generated by the muscles at the anterior pelvis, with the arcuate ligament recognized as the primary stabilizing ligament of this joint. Therefore, these structures are of great importance for the hockey athlete, as the repetitive rotational activities during hockey, such as shooting and skating, generate substantial shearing forces across the pubic symphysis, the arcuate ligament, and between the parallel tissue fibers.69,70 Due to the commonality of the tendons between the: external oblique and adductor longus (AL), the rectus abdominis (RA) with the adductor brevis (AB) and gracilis, and the transversus abdominis and internal oblique (known as the “conjoint tendon”), CMI can involve disruption to the musculature, fascia or tendons of these adductor or lower abdominal muscles.65,71,72 However, it is becoming increasingly common in the literature for CMI surgical interventions to involve repair of the pubic aponeurotic complex, which is the region where the above described muscles, along with the inguinal ligament and pectineus converge on the pubis.65,73
High-level hockey athletes may be at an increased risk of a CMI due to the significant transverse strain experienced at the pubic symphysis, particularly with the presence of FAI.74 Specifically, the limited hip IR ROM often associated with cam morphology, is reported to significantly increase this shearing force and transverse plane movement during high-force rotational movements.74 This will substantially increase the opportunity for disruption of the numerous components of the aponeurotic complex.70 Supporting this proposed association was the finding that among 38 professional athletes from various sports diagnosed with a symptomatic CMI, 39% (15/38) had all symptoms resolve following FAI corrective surgery alone. Furthermore, the 12 athletes that had previously received surgery for the CMI alone were only able to return to competition following additional surgery to correct the FAI.70 Thus, the reduction in hip IR ROM associated with cam morphology may explain the relatively high prevalence of CMI in hockey athletes, particularly during the key activities of shooting and skating.64
A higher shot velocity requires significantly greater peak trunk rotation away from the puck during the wind-up phase of shooting, to evoke a stretch-shortening cycle action of the trunk muscles.75 This increases the rotational acceleration of the trunk, and hence, the ability to apply a greater impulse to the puck. As the rotation occurs over a fixed lower extremity, the result is a forceful IR of the head of the femur on the ipsilateral side of the body that the shot is directed towards.76 If the athlete has a cam morphology on this side, there will likely be a substantial increase in the transverse strain experienced at the pubic symphysis, arcuate ligament and aponeurotic complex.74 Additionally, during the follow through of the shot a rapid lengthening of the internal oblique and transversus abdominis occurs on the contralateral side, due to the eccentric strength requirements at end range needed to decelerate the trunk. For an athlete with inadequate trunk muscle strength, motor control or rotational ROM, there could be an increase in the risk of disruption to the abdominal muscles and the conjoint tendon.
Current evidence suggests that more than 30% of hockey athletes have RA-adductor dysfunction on MRI, and the mechanics of forward sprint acceleration strides may help explain this prevalence.38,66,71,77 Higher-caliber hockey athletes utilize significantly greater hip extension ROM and angular velocity, combined with increased pelvic tilt and trunk rotation during acceleration strides.25,78,79 Importantly, Economopoulos et al.77 reported that repetitive hip hyperextension combined with trunk and pelvic rotation leads to significant degradation of the RA and adductor tendons. Concerningly, partial disruption of one of these tendons can lead to an uneven distribution of contractile force between the AL and RA. This imbalance further increases the shearing force at the pubic symphysis, particularly at the enthesis of the RA inferior fibers, potentially resulting in a CMI.
During abrupt changes-of-direction, hockey athletes initiate deceleration by rotating the trunk towards the intended direction of the turn, immediately prior to lowering their center-of-mass using a combination of trunk, hip, and knee flexion.80 Simultaneously, there is a deliberate movement of ipsilateral trunk lateral flexion towards the outside leg, along with hip IR, to increase friction between the skate blades (which are perpendicular to the direction of travel) and the ice, facilitating more rapid deceleration. This combined trunk action of contralateral rotation and ipsilateral lateral flexion, with hip IR of the outside leg, will likely increase the eccentric lengthening and force on the contralateral trunk muscles and ipsilateral adductor muscles, which together may increase the likelihood of RA-adductor dysfunction, particularly in athletes with insufficient lumbopelvic control or strength. Interestingly, it has been reported that following effective rehabilitation from SRGP, athletes can demonstrate reduced pelvic drop and ipsilateral trunk lateral flexion during a continuous side-to-side hop task, which may decrease the force experienced at the anterior pelvis, reducing the opportunity of RA-adductor dysfunction.81 Therefore, targeted training prescription aimed at enhancing lumbopelvic control and strength is likely beneficial for hockey athletes.
Lastly, higher-caliber hockey athletes are reported to apply hip abduction force with greater angular velocity through an increased ROM (up to 50° of hip abduction) during propulsive strides, when compared to lower-caliber athletes.21,82,83 While the application of hip abduction force through this large ROM significantly increases strain on the labrum, it may also increase the opportunity of muscular injuries to the hip and groin, particularly in the presence of an intra-articular injury or cam morphology.44,45 A hockey athlete with restricted hip ROM or reduced strength in abduction or extension, will likely utilize compensatory movement strategies to generate the required impulse into the ice surface to achieve a high sprint skating velocity.61,79,84,85 These strategies typically involve increased ipsilateral rotation and anterior tilting of the lumbopelvic region to compensate for limited abduction or extension ROM, while also facilitating visual scanning during play.61,84,86 The abduction and extension demands of the hockey stride lengthens the adductors, while the increased pelvic tilt and ipsilateral lumbopelvic rotation will elongate the lower abdominal muscles on the propulsive leg. Together, these requirements likely increase the strain on these muscles and their common tendons, further enhancing the opportunity of a CMI or RA-adductor dysfunction. This strain will be further magnified with the presence of femoral head asphericity, limited hip ROM, or if these skating mechanics are combined with activities that exacerbate the trunk rotation demands, such as passing, shooting and body checking.74
Hip Flexor and Adductor Injuries
Hip flexor and adductor injuries are highly prevalent in hockey and can significantly limit both short-term and long-term performance.64,87–89 Notably, hip flexor strains have been reported as high as 2.47 per 10,000 athlete exposures in collegiate-level hockey athletes, with these athletes also more susceptible to adductor strains compared to their counterparts in other sports.88,89 While only ~24% of hip flexor strains and ~55% of adductor injuries result in significant time-loss from training and competition, indicating that athletes can still perform, albeit at a lower performance level, the unique skating mechanics and potential intra-articular hip injuries may increase the likelihood of hip flexor and adductor injuries.1,3
Although limited research has examined the risk factors for hip flexor injuries in hockey athletes, hip flexor discomfort can be a common complaint and incite a similar pain response to adductor strains.87 The hip flexors are essential for rapid recovery of the leg under the pelvis during a skating stride, however, it is likely that the majority of discomfort is related to tissue irritation as opposed to a muscular strain.25 Importantly, the hip flexors are crucial for both stabilization of the femoral head, as well as limiting excessive hip extension ROM. As a result, damage to the labrum or lengthening of the IFL, may increase the reliance on these muscles to provide the required stability and restraint, potentially leading to increased muscular tightness.90 Therefore, compression of the iliopsoas against the acetabulum to stabilize the femoral head anteriorly, may result in hip and groin pain due to inflammation of the posterior iliopsoas tendon and acetabular labrum.91 Furthermore, restricted iliopsoas length to limit hip extension ROM can also cause irritation and audible popping as the iliopsoas tendon moves laterally over the iliopectineal eminence or femoral prominence (“coxa saltans”).92 This highlights the importance of screening and regularly monitoring hip extension ROM and hip flexor strength in the hockey athlete.
Originally emphasized by Chang, Turcotte and Pearsall,43 the importance of the adductor magnus (AM) in sprint skating was highlighted with hockey athletes displaying greater activation with increased sprint skating speed and peak activation at ice-contact, suggesting a role in hip stability for single leg stance. Additionally, the AM experienced a greater peak at the end of the propulsive phase, highlighting that the greatest demand on the adductor occurs in a lengthened position. Therefore, the repetitive high-force concentric and eccentric actions during the propulsive and recovery phases of the skating stride may lead to acute strains of the adductor muscles, or the accumulation of fatigue and potential overuse injuries at the musculotendinous junction (MTJ) or tendon.93
The AL is the most typically injured adductor muscle during high-force movements, and research indicates that its proximal tendon exhibits significantly reduced vascularity when compared to the AB and gracilis.71,94,95 This raises the possibility that AL injuries in hockey are commonly associated with tendinopathy or an incomplete and delayed repair at or near the MTJ, where force requirements are high.43 Considering the highly fibrocartilaginous nature of the tendons and entheses of the AL, AB, AM and gracilis, which provide additional strength in the direction of stress, it appears that the contractile components of the adductors may be more susceptible to injury when there is limited ROM or a lack of muscular strength at end range.71 As such, the reduced hip muscle function typically associated with intra-articular hip injuries will likely cause hockey athletes to reach their upper limit of abduction ROM earlier during skating strides, further highlighting the importance of optimizing hip strength and ROM.12,57,60–62
The primary factor associated with future adductor strain injury risk has been reported as an adduction to abduction strength ratio of less than 80%.87 Additionally, preseason adductor injuries in semi-professional hockey athletes have been associated with lower hip abduction ROM and a greater magnitude of decline in adductor strength at a joint-angle position of 50° of hip abduction compared to a position of 25° of hip abduction, when compared to an uninjured cohort.96 Due to the trunk position required to maintain equilibrium during change-of-direction efforts while skating, it is theorized that this increases the eccentric load on the pubic symphysis and adductor muscles.81 Therefore, the reduced hip strength and muscle strength imbalances associated with cam morphology, intra-articular hip injuries, and the presence of hip and groin pain may increase the opportunity of adductor injuries in hockey athletes.1,87,96 Importantly, Suits et al.97 recently identified that hip total rotation ROM, adductor strength and the adduction to abduction strength ratio was significantly reduced following a single on-ice training session. Therefore, with the presence of fatigue or RA-adductor dysfunction there may be a reduced ability to withstand the substantial loads experienced during forward sprint skating and change-of-direction efforts.94,95,98 As such, prescribing training aimed at increasing the adduction to abduction strength ratio, enhancing adductor joint angle-specific strength, and improving or maintaining total rotation, abduction and extension ROM of the hip, are suggested to potentially mitigate the opportunity and severity of these injuries in hockey athletes.
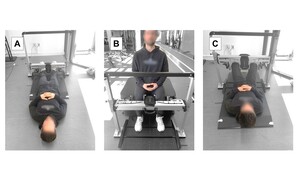
Future research should aim to establish normative ROM and strength data for the trunk and hips in the joint actions specific to hockey athletes. Whilst reductions in hip rotation ROM and adductor strength have been reported following on-ice training, additional research is required to determine whether these reductions are associated with an increased risk of intra-articular hip injuries, CMI, or hip flexor and adductor injuries. In the absence of such research, it is recommended that practitioners screen and monitor hockey athletes’ ROM and strength in the key joint actions and utilize evidence-informed and experience-based judgement to benchmark the data and prescribe targeted exercise interventions aimed at mitigating injury risk. Based upon the current literature and anecdotal evidence, the authors suggestions for screening and monitoring assessments and target values are provided in Table 1 and Figures 2 and 3.
CONCLUSION
FAI is highly prevalent in hockey, with most elite-level hockey athletes exhibiting cam morphology. Previously attributed to the unique skating mechanics, recent research suggests that repetitive joint loading during adolescence, particularly between the ages of 12 to 14 years old, plays a pivotal role in the development of cam morphology in these athletes. Specifically, large shear stresses on the femoral head during skating may disrupt blood flow to the epiphyseal plate, leading to hypertrophic chondrocytes in this region, and eventually callus formation and a cam morphology. Given the increasing incidence of ESS and early-onset hip and groin issues in hockey, early intervention is crucial. Strategies including managing the intensity and volume of hockey activities, promoting participation in other sports, prescribing comprehensive physical training, and developing a variety of movement literacy skills, are suggested to expose the tissues to a variety of loads and allow for adequate recovery from repetitive stresses.
Over half of elite hockey athletes experience hip and groin pain, which are likely attributed to intra-articular hip injuries that result from the unique skating mechanics and are exacerbated by cam morphology. These injuries affect the passive stabilizers of the hip, such as the labrum and ligamentous tissues, which can reduce joint stability and heighten pain perception, due to the large distribution of nociceptors and mechanoreceptors. If tissue creep of the IFL and LT occurs there can be greater femoral head translation, exacerbating pain due to tissue irritation and potential osteochondral damage. The inherent protective mechanism involves increased muscular activation and tension, likely resulting in capsular tightness and reduced hip joint ROM and strength. Moreover, the combination of restricted hip ROM and strength associated with cam morphology, along with fatigue, can evoke compensatory strategies during skating and shooting, contributing to the high prevalence of CMI and hip flexor and adductor injuries in hockey athletes. Specifically, limited hip IR ROM increases shearing forces at the pubic symphysis during rotational movements, exacerbating strain at the aponeurotic complex, while factors such as hip and groin pain, intra-articular injuries, or fatigue may further worsen joint angle-specific weaknesses and increase the risk of adductor strains.
Conflicts of interest
The authors report no conflicts of interest.

__hip_exten.jpg)

__hip_exten.jpg)
