Introduction
Syndesmosis injuries, or ‘high ankle sprains’, are relatively uncommon making up between 1% and 18% of ankle ligament injuries.1,2 This large variation might indicate an under-reporting of these injuries,6 reflecting the difficulty identifying syndesmotic ligament damage.3 Syndesmotic ankle sprains, occur less frequently than the traditional lateral ankle sprain. Syndesmotic injuries result from excessive external rotation or forced dorsiflexion of the foot, often seen in sports involving a cutting motion.4 Injury can also occur following a forced external rotation movement on a fixed foot as can occur during contact sports.4 Unlike lateral ankle sprains, high ankle sprains are notorious for prolonged recovery times and a high rate of residual symptoms, often leading to diminished performance.5–7 Sporting populations are more likely to suffer from syndesmotic injuries due to the forces required to damage the ligaments.3,8 Delayed or inadequate treatment can lead to chronic instability, pain, and early joint degeneration. Not only are syndesmotic injuries associated with higher levels of disability, but they also present with prolonged periods out of sporting participation lasting for 3 – 6 months.5–11 Syndesmotic sprains have often been described as one of the most difficult sporting injuries to treat,3 with rehabilitation potentially taking between twice and 30 times longer than isolated lateral ligament sprains.12 Undiagnosed or incorrectly treated syndesmosis injuries can lead to pain, worsen athletic performance, lengthen recovery, and cause arthrosis.13
ANATOMY
Before delving into treatment options, it is essential to understand the anatomy. An intact distal syndesmotic ligament complex is important for stability in the ankle joint. The distal tibiofibular joint is described as a syndesmosis. It comprises the tibia and fibula, the fibrous interosseous membrane (IOM) between the two bones, the anterior inferior tibiofibular ligament (AITFL), posterior inferior tibiofibular ligament (PITFL), transverse ligament (TL) and the interosseous ligament (IOL).1 (Figure 1)
TREATMENT STRATEGIES
Treatment strategies for high ankle sprains range from conservative management with immobilization and physical therapy to surgical intervention. Conservative management revolves around the RICE protocol (Rest, Ice, Compression, Elevation), bracing, and a gradual approach to rehabilitation. There are several surgical options to consider in maintaining the structural integrity of the ankle joint after a grade II or when a higher syndesmosis injury has occurred. Syndesmotic screw (SS) fixation has traditionally been accomplished with transosseous screws, and it remains the most commonly utilized method of fixation for syndesmosis injury.14 In this procedure, screws are implanted through the fibula into the tibia to stabilize the syndesmosis. This poses problems for the athletic population as screw fixation can lead to syndesmosis malreduction and has been reported in up to 50% of cases.15–18 Additional concerns of this technique include screw loosening, screw breakage, and the potential need for screw removal between 3 and 6 months post fixation, potentially delaying rehabilitation and return to sport.17,19–21 An unstable syndesmosis injury requiring surgical fixation will commonly require 4–6 months before successful return to sport.16 However, this paradigm is shifting with the introduction of the tightrope surgical procedure, which promotes dynamic stabilization of the syndesmosis, and aggressive post-operative rehabilitation.
Tightrope Surgical Procedure
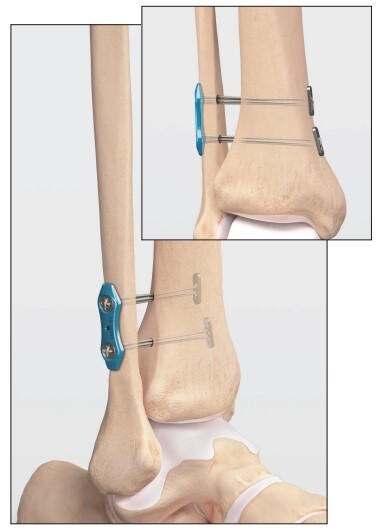
The tightrope procedure has been popularized in high profile sports and gained traction in recent years as a minimally invasive surgical option that provides immediate stabilization of the syndesmosis. This technique uses a suture-button construct, known as the Tight-Rope™ (Arthrex, Inc, Naples, FL).22 This surgical procedure is performed by inserting a No.5 FiberWire® loop (Arthrex) through the tibia and fibula and placing tension on the FiberWire® (Figure 2). (Video animation: https://youtu.be/imsmVQyRGRA?si=9fj7gVY5UoN0UMXq) This provides physiologic stabilization of the ankle mortise and reduces the need for a second procedure to remove the hardware.16 The tightrope procedure has a number of advantages over traditional screw fixation: it allows for a small amount of normal biomechanical movement at the syndesmosis; it rarely requires a second operation to remove the device; it provides significantly better anatomic reduction and it allows for earlier return to weight-bearing, rehabilitation and ultimately sport.8,16,22–24
Advantages
-
Immediate Weight Bearing Stability: The construct creates immediate stabilization of the syndesmosis which allows for early weight-bearing expediting the recovery and minimizing muscle atrophy.
-
Maintains Joint Mobility: Traditional screw fixation can limit tibiofibular motion, potentially altering ankle biomechanics. The tightrope maintains physiologic motion while ensuring stability and reducing the risk of malreduction and hardware failure. This can accelerate rehabilitation and reduce post-operative stiffness.
-
No Need for Secondary Surgery: In many cases, the tightrope remains in place indefinitely and does not typically need to be removed, unlike syndesmotic screws which may require a second procedure in cases of breakage or discomfort.
Post-operative Rehabilitation
Rehabilitation plays a pivotal role in optimizing outcomes post-tightrope surgery. In conjunction with the tightrope procedure, the rehabilitation approach is more intensive and initiated earlier than traditional protocols in order to expedite recovery. This approach challenges traditional protocols by promoting earlier weight-bearing and active motion. The primary goals are to restore range of motion (ROM), enhance muscular strength, improve proprioception, and facilitate a quicker return to full activity. An aggressive post-operative rehabilitation strategy after the tightrope procedure is essential for optimal outcomes.
The approach should be progressive and tailored, focusing on:
-
Early Mobilization: Aided by the tightrope procedure’s stability, early ankle mobilization can combat stiffness, enhance circulation, and facilitate tissue healing. Gentle range-of-motion exercises can be introduced within the first post-operative week.
-
Early Weight-bearing Progression: The stability conferred by the tightrope allows for a quicker transition to partial and then full weight-bearing. Therefore, Controlled weight-bearing can be introduced earlier than traditional protocols. This progression not only aids in functional recovery but also decreases the risk of osteopenia associated with prolonged immobilization.
-
Strength Training: Resistance exercises targeting the calf, peroneals, and intrinsic foot muscles should be initiated as soon as pain allows. Strengthening these muscles ensures dynamic ankle stability and promotes optimal gait patterns. In addition, improving hip and core strength is critical in controlling medial/lateral ankle movements which is important to control with ankle injuries. Proximal stability for distal mobility is critical to restore and improve.
-
Proprioceptive Training: High ankle sprains can impair proprioceptive feedback. Incorporating balance exercises more quickly can restore proprioceptive acuity and reduce reinjury risk. Essential element to successful rehabilitation is the enhance proprioception & improve neuromuscular control of the entire lower extremity.
-
Functional Retraining: Sport or activity-specific drills should be integrated as the patient approaches the final rehabilitation stages. This ensures a safe return to pre-injury activity levels. The authors of this article strongly believe a functional return to play testing protocol and criteria.
Immediate Post-operative (0-1 weeks)
Goals: Manage pain, control swelling, and protect the surgical site.
Immediate Post-Operative Phase (0-1 weeks): The rehabilitation commences within 24-48 hours post-surgery, a stark contrast to the traditional approach of immobilization. Pain management is crucial, utilizing cryotherapy, elevation, and analgesics. During the first 4 days the ankle will be wrapped in a compressive bandage and treated with elevation, pain control, cold compression device, and kept NWB. The dressing is typically removed on day 4 and the focus shifts to rehabilitation, focusing on a weight bearing progression with selling control. Given the dynamic stability offered by the tightrope system, partial weight-bearing progressing begins on day 4 to weight bearing tolerated in CAM walking boot is encouraged, using assistive devices as necessary. The rehabilitation specialist must closely monitor for any signs of excessive pain, swelling, or complications. Early interventions include passive and active-assisted ROM exercises, isometric contractions of the ankle musculature, and gentle mobilizations performed by the therapist to preserve joint mobility.
Strengthening of the hip and core, quads and hamstrings can be successfully & safely performed during the first week following surgery. Intrinsic strengthening of the foot muscles can be performed but we recommend no ankle strengthening during the early healing phase. (See Table 1)
Intermediate Phase (1-3 weeks)
Goals: Gradual restoration of ankle motion, strength, and proprioception. Full weight bearing out of the boot with normal range of motion by day 20.
During this phase, the intensity of the rehabilitation program increases. Weight-bearing is progressed and wean out of the boot day 8 to 12, and progress to an ASO brace for ambulation. Emphasis during this this phase will focus on normalizing gait patterns. Therapists incorporate proprioceptive exercises, such as single leg stands and balance board activities, to restore neuromuscular control. Proprioception and neuromuscular control drill should be emphasized during this timeframe.
During week 2, ankle strengthening exercises are initiated and other lower extremity strengthening exercises employing closed kinetic chain exercises and functional balance drills within pain limits. Pool exercises may also be utilized, to employ the water’s buoyancy to facilitate safe, effective strength exercises and gait training. Continuous reassessment ensures that the interventions align with the healing timeline and patient tolerance. Be sure to restore hip mobility and hip/core strength before beginning a running and agility program in the phase.
It is important to note that during this phase the rehabilitation team does not need to slow the progression down if the athlete is moving faster. (See Table 2)
Functional Rehab Phase (3-5 weeks)
Goals: single leg muscular strength, enhance proprioception & neuromuscular control and restore functional movement patterns.
The objective shifts to restoring full function and a safe return to sport or activity. Exercises are more dynamic, incorporating plyometrics, agility drills, and sport-specific movements. Strength training progresses to include eccentric exercises for muscle-tendon optimization. Gradually progress to agility drills, neurocognitive drills and reactive dynamic stabilization.
During this phase, gait training continues with resumption of a normal gait pattern in a normal shoe. A running progression is implemented after 2 full weeks of pain free walking. The introduction straight line running and cutting are evaluated using functional assessments to gauge readiness for return to play, focusing on symmetry and performance in comparison to the uninjured side. In addition, the athlete must continue lower extremity strengthening, ankle mobility, and dynamic stabilization and neuromuscular control drills. (See Table 3)
Return to Play Phase 4-6 weeks)
Goals: Gradual return to sports or desired activities, improve agility, and enhance performance.
Interventions: Sport-specific drills, plyometrics, and high-intensity functional exercises. Focus on change of direction and deceleration drills.
Return to play testing and criteria: Consider using a reactive T run for time, reactive L run for time, single leg hop tests, single leg squat that’s symmetrical and 15 single leg hops which are pain free and symmetrical.25 (See Table 4)
Clinical Considerations
The tightrope procedure and the associated aggressive rehabilitation model have several implications for rehabilitation:
-
Early Intervention: Given the potential for early weight-bearing, rehabilitation providers must be equipped to manage these patients sooner post-operatively than traditional surgical interventions.
-
Dynamic Assessment: The suture-button device allows for tibiofibular motion. Clinicians should be skilled in assessing this motion and understanding its implications for rehabilitation.
-
Patient Education: Educating patients about the procedure, recovery timeline, and importance of adherence to rehabilitation is crucial.
-
Interdisciplinary Collaboration: Understanding the surgeon’s preferences, post-operative protocols, and any potential complications is essential for individualized patient care. Collaboration between orthopedic surgeons, physical therapists, and other healthcare professionals is crucial for the success of this protocol.
Despite the promising outcomes associated with the tightrope procedure and aggressive rehabilitation, clinicians must remain circumspect. Not all patients with high ankle sprains may be suitable candidates for this approach. Factors like the extent of injury, patient’s general health, activity levels, and goals should be considered. Individual variability in pain tolerance, healing capacity, deltoid ligament involvement, and pre-injury fitness levels necessitates a tailored approach. Furthermore, the definition of “aggressive” can vary significantly; thus, therapists must avoid a one-size-fits-all methodology. While the tightrope procedure with aggressive rehabilitation offers many advantages, clinicians must be wary of potential pitfalls:
-
Over-aggression: Pushing too hard, too soon can exacerbate inflammation and delay healing. Rehabilitation progression should always be pain guided.
-
Scar Tissue Formation: Early mobilization minimizes scar tissue but does not eliminate the risk. Manual therapy techniques, like cross-friction massage or instrument-assisted soft tissue mobilization, can help address fibrotic changes.
-
Residual Instability: Despite surgical stabilization, some patients may report feelings of instability. Bracing or taping techniques can be adjunctive tools in these instances.
Compliance and education are pivotal. Patients who are informed about their recovery timelines and the rationale behind their rehabilitation protocol are more likely to adhere to home exercise programs and post-operative instructions. Additionally, interprofessional collaboration is essential.
Conclusion
The tightrope surgical procedure is a new surgery procedure for high ankle sprains presents a promising avenue for expedited recovery and optimal functional outcomes. When paired with aggressive post-operative rehabilitation, patients can expect a comprehensive approach that addresses not just anatomical integrity but functional prowess as well. The combination of this procedure with an aggressive post-operative rehabilitation approach can lead to faster recovery times, improved function, and a quicker return to sport or desired activities. While initial studies have shown promising results, long-term outcomes and randomized controlled trials comparing this method to conservative treatments are still needed. With interdisciplinary collaboration, evidence-based practice, and patient-centered care, the management of high ankle sprains will continue to evolve, leading to better outcomes for patients. As with all treatment strategies, individualized care, patient feedback, and evidence-based practice remain at the forefront of ensuring optimal outcomes.
There are several keys to successful rehabilitation, these include allow early healing, restoration of normal hip range of motion and strength, improve ankle dynamic stabilization & control and utilize an objective return to play criteria.
Future Directions
Continued research is imperative to validate the long-term efficacy and safety of the tightrope procedure coupled with aggressive rehabilitation. Comparative studies with traditional management strategies, investigations into patient satisfaction, and qualitative research into patient experiences will enrich the existing body of knowledge. Furthermore, developing standardized guidelines for what constitutes “aggressive rehabilitation” will mitigate the risks of overtreatment and ensure consistency in care delivery.