INTRODUCTION
Upper extremity function requires adequate mobility in the upper quarter, including the extremity joints, the scapulothoracic articulation, and the thoracic spine.1–3 For patients with shoulder conditions, clinical testing typically focuses on mobility of the shoulder, and specifically glenohumeral active and passive range of motion (ROM).4,5 Additionally, assessing glenohumeral active and passive external rotation ROM is important during return to sport decision making.6 Total arc of motion is the sum of shoulder internal and external ROM measured at 90 degrees of shoulder abduction7 and has been studied extensively in overhead athletes.5,7–12 A side-to-side difference greater than 5 degrees in total arc of motion has been associated with shoulder and elbow pain and risk for shoulder injury in overhead athletes.7,8,13,14 While shoulder ROM and total arc of motion identify impairments in glenohumeral mobility, they do not integrate scapulothoracic and thoracic spine mobility that might give a more comprehensive indication of upper extremity function.
The seated wall angel (SWA), sometimes referred to as the W-stretch, has been described on the internet and on social media sites as an exercise to improve upper quarter mobility.15–17 The goal of the SWA is to get the entire posterior upper extremity in contact with the wall and some recommend arm elevation (movement) in this position.15,18 Because the SWA requires scapular retraction and thoracic extension, it may give additional information about shoulder complex function compared to glenohumeral mobility testing. In addition, the SWA may be more functional than other glenohumeral mobility tests for overhead athletes and could be used as a screen of upper extremity function in athletes prior to returning to an overhead sport after an injury or as part of a comprehensive upper extremity mobility assessment. The SWA has not been described as a clinical test with a mechanism for scoring.
The purpose of this study was to explore the clinical utility of the SWA as a test with scoring. The authors hypothesized that SWA test scores would be lower on the injured than uninjured side, improve over time, and show stronger association with patient-reported shoulder function compared to other clinical tests of shoulder mobility. Knowledge generated by this study can help clinicians discern the potential for utilizing the SWA test during clinical examination and clinical decision-making.
MATERIALS AND METHODS
Study Overview
This study is a secondary analysis of data acquired for a study focused on developing an upper extremity testing battery. Clinical tests and patient-reported outcomes were collected soon after the physical therapy examination (initial testing) and six weeks later (follow-up testing).
Participants
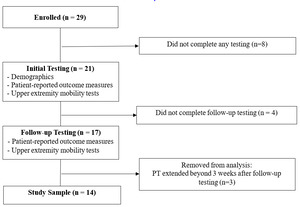
Between April 2017 and March 2020, patients with anterior shoulder instability undergoing physical therapy were recruited for this study (Figure 1). Inclusion criteria for the study were age 16 to 30 years, physician-diagnosed anterior shoulder instability determined by recent traumatic dislocation or subluxation, and participation in at least 50 hours of exercise in the year prior to injury. Patients were excluded from participation if they had resting shoulder pain greater than 5 on the 0 (no pain) to 10 (worst pain imaginable) point Numeric Pain Rating Scale (NPRS),19 an additional episode of shoulder instability before completing the study; or history of another physician-diagnosed shoulder, elbow, or wrist injury to either upper extremity. All patients provided written informed consent to participate in the study on a form approved by the Institutional Review Board.
Study Design
Patients participated in initial testing soon after their physical therapy examination and follow-up testing six weeks later. The interval between test sessions was selected to allow time for improvement in shoulder function and near the anticipated end of the physical therapy episode of care. Testing consisted of collection of demographic information, performance of clinical tests (SWA test, external rotation passive ROM, and total arc of motion), and completion of patient-reported outcomes focused on shoulder function.
Demographic Information
Demographic information was collected by self-report including age, sex, height, weight, the number of prior shoulder instability events, the date of the most recent shoulder instability event, the side of injury, and the arm used to throw a ball (dominant extremity). The NPRS was used to determine the intensity of shoulder pain (0= No pain, 10=Worst pain imaginable).19 Patients rated their current, usual, best, and worst levels of pain, which were averaged to create a composite of shoulder pain intensity. Height and weight were used to compute body mass index (BMI). The time from the most recent shoulder instability event to initial testing and from the physical therapy evaluation to initial testing were computed. The number of physical therapy visits attended was determined from the electronic medical record.
Testing Procedures
Testing was administered by a physical therapist or athletic trainer, each with more than 10 years of clinical experience treating patients with upper extremity conditions. The same clinician administered initial and follow-up testing for a given subject. Before the study was initiated, the clinicians reviewed and practiced the standardized testing and scoring procedures.
Pre-testing warm-up consisted of five minutes of light upper body ergometry, 30 small forward and backward arm circles, and self-stretching as desired by the patient. For all tests, patients were given standardized instructions and a practice trial.
Seated Wall Angel Test
The test was performed with the patient seated on the floor with knees bent, feet flat on the floor, and the lumbar spine and head in contact with the wall (Figure 2). From this position, the patient was instructed to elevate elbows to shoulder height, and externally rotate the shoulders as much as possible. The patient held the position for scoring, which differs from the SWA as an intervention during which the arms are elevated overhead while maintaining contact with the wall. Scoring was based upon the number of contact points with the wall (elbow and fingertips, posterior fingers, posterior forearm). 0: < 2 points of contact, 1: elbow and fingertip contact, 2: elbow and posterior finger contact, 3: elbow, posterior forearm, and posterior hand contact. The injured and uninjured sides were scored separately.
Reliability of the SWA test was assessed during the study with a sample of convenience. Inter-rater reliability of the scoring method was assessed for the right and left sides of two patient study participants and 10 uninjured controls. One rater performed scoring in real-time, and one rater performed scoring from video. Intraclass correlation coefficients [95% confidence interval] were 0.894 [0.681, 0.968] for the right side and 0.867 [0.618, 0.959] for the left side. Additionally, intra-rater reliability of scoring was assessed for the right and left sides of 11 study participants and 11 uninjured controls. Scoring was completed from video on two occasions, 10 days apart. Intraclass correlation coefficients [95% confidence interval] were 0.891 [0.758, 0.953] for the right side and 0.891 [0.751, 0.954] for the left side.
Shoulder External Rotation Range of Motion and Total Arc of Motion
Total arc of motion is the sum of passive shoulder internal and external rotation ROM (Figure 3).7 Testing was performed with the subject in supine and the arm abducted to 90 degrees in the scapular plane with manual stabilization of the scapula at the coracoid process.7 A small towel roll was placed under the humerus to ensure motion occurred in the correct plane. External rotation ROM was measured with a standard goniometer when the end point was perceived by the tester or if a patient had apprehension. Internal rotation was measured in the same position with a standard goniometer when the end point was perceived by the tester. Total arc of motion was determined by summing external rotation and internal rotation ROM.
Patient-Reported Outcomes
The American Shoulder and Elbow Surgeons Shoulder Assessment Form (ASES) is a standardized questionnaire for measuring shoulder pain, instability, and activities of daily living.20,21 Scores range from 0 to 100 points, and higher scores represent better shoulder function. The ASES is responsive to change, and the minimal clinically important difference (MCID) is 6.4 points.20
The Western Ontario Shoulder Instability Index (WOSI) is a disease-specific quality of life questionnaire for patients with shoulder instability.22 Scores range from 0 to 2100 points, with lower scores representing better function. The WOSI is responsive to change, and the MCID is 220 points.22
Statistical Analysis
No a priori power calculations were performed for this study because it is a secondary analysis. All analyses were performed with commercial software (IBM SPSS Statistics version 28). Descriptive statistics were generated for demographic information variables, clinical test variables, and patient-reported outcome scores. Statistical significance was set at alpha less than 0.05.
Paired t-tests were used to compare SWA test scores between sides at initial testing and to compare injured side SWA test scores at initial and follow-up testing. Effect sizes (Cohens d) were calculated for the difference in clinical test values and patient-reported outcome scores from initial testing to follow-up testing using the standard deviation of the difference. An effect size of 0.2 is considered a small effect size, 0.5 is considered moderate, and > 0.8 is considered large.23
Associations among the clinical test values on the injured side (SWA test, external rotation ROM, and total arc of motion) and patient-reported outcome scores were examined at initial testing and follow-up testing with Pearson correlation coefficients. Correlation coefficients less than 0.4 were considered weak correlations, between 0.4 and 0.69 considered moderate correlations, and 0.7 and higher considered strong correlations.24 If more than one clinical test showed significant correlation with a patient-reported outcome score, stepwise linear regression analysis was performed with the clinical tests as independent variables and patient-reported outcome score as the dependent variable to understand the relative contribution of the clinical tests to patient-reported shoulder function. The criteria for removal from the model was p> 0.05.
RESULTS
Demographic information for the patients is found in Table 1. Males comprised 71% of the sample. Initial testing occurred on average about four weeks after the most recent instability event, and approximately a week after the physical therapy evaluation. The number of instability events ranged from one to 20. Patients attended between one and 13 physical therapy visits in the six weeks from initial to follow-up testing. Only two patients had additional physical therapy visits after follow-up testing: one visit and two visits, respectively.
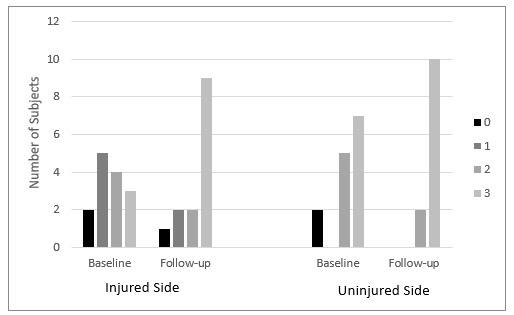
SWA test scores, values for shoulder external rotation ROM, total arc of motion, and patient-reported outcome scores are found in Table 2. Shoulder external rotation ROM was unavailable for two patients at both testing dates and three additional patients at follow-up testing because only total arc of motion was recorded. Thus, analyses involving shoulder external rotation ROM include data from 12 patients at initial testing and nine patients at follow-up testing. At initial testing, the mean injured side SWA test score was significantly lower than the score on the uninjured side (p = 0.045). Also, the injured side SWA test score significantly increased from initial testing to follow-up testing (p = 0.041). The distribution of SWA test scores is found in Figure 4. Only 21% of patients achieved the highest score (i.e., “3”) on the injured side at initial testing, whereas 64% achieved the highest score on the injured side at follow-up testing. Effect sizes for the change from initial to follow-up testing did not cross 0 for injured side SWA test score, injured side total arc of motion value, and patient-reported outcome scores. The magnitude of the effect sizes in descending order was ASES score, WOSI score, injured side SWA test score, and injured side total arc of motion value (Table 2).
SWA test was the only clinical test to show significant correlation with ASES and WOSI scores at initial testing (r=0.597 and r=-0.648, respectively; Table 3). The magnitude of the correlations is moderate, and the direction of association is positive for ASES and negative for WOSI, indicating that a higher injured side SWA test score is associated with better patient-reported shoulder function. SWA test score and total arc of motion on the injured side were both associated with WOSI score at follow-up testing (r=-0.611 and r=-0.574, respectively; Table 4). The magnitude of the correlations is moderate, and the direction of associations is negative, indicating that higher values for the injured side SWA test and total arc of motion on are associated with better patient-reported shoulder function. The linear regression model with these clinical tests retained only the injured side SWA test score, and the correlation to WOSI score as indicated in Table 4. In addition, significant positive correlations of a moderate to high magnitude were found among clinical tests at initial testing and follow-up testing.
DISCUSSION
This study explored the clinical utility of the SWA as a test with a proposed scoring mechanism. This is novel because the SWA has previously been described as an intervention, not as a clinical test. The hypotheses for the study were supported. First, the injured side SWA test score was lower than the uninjured side at initial testing and improved at follow-up testing. Moreover, the injured side SWA test score demonstrated significant associations with ASES score and WOSI score at initial testing and WOSI score at follow-up testing. Injured side values for the other clinical tests (i.e. total arc of motion and external rotation ROM) were not significantly correlated with ASES and WOSI scores at initial testing and total arc of motion was removed from the regression model in favor of the SWA test score for association with WOSI score at follow-up testing. The clinical utility of the SWA test is supported by distinguishing the injured side from the uninjured side and by having stronger associations with patient-reported shoulder function than shoulder mobility tests.
The patient population and the timing of initial and follow-up testing may contribute to the findings of this study. The population for this study was patients with anterior shoulder instability. As opposed to passive shoulder range of motion testing that took place in the scapular plane, the SWA test position of combined shoulder abduction and external rotation in the frontal plane could make patients apprehensive of experiencing instability25–27 and may explain the lower test score on the injured side than the uninjured side at initial testing. Further testing in patient populations with other shoulder conditions is necessary to confirm whether the SWA test discriminates the injured side from the uninjured side. Significant improvement in the SWA test score on the injured side at follow-up testing indicates more body contacts with the wall. It cannot be determined how much of the improvement was the result of increased shoulder external rotation ROM, decreased apprehension, changes in scapular movement and thoracic spine ROM, or improved scapular and rotator cuff muscle strength. At follow-up testing, which was near the end of rehabilitation for the patients, 64% achieved the highest score on the SWA test. The six-week interval between testing time points was intended to allow time for a change in shoulder function and not to coincide with return-to-sport testing. Recovery time after a shoulder anterior instability event varies in the literature but many athletes return to sport within two to three weeks after injury.28–30 If testing took place at return-to-sport, it is unknown if the SWA test would show a ceiling effect. Regardless, experts recommend including ROM as a part of upper extremity return-to-sport testing.6
The glenohumeral joint, thoracic spine and scapula make contributions to maximal external rotation of the upper quarter.1 To achieve the highest score on the SWA test, a patient must have the necessary shoulder external rotation ROM, scapular movement, and thoracic extension to contact the entire posterior upper extremity with the wall. At initial testing, five patients achieved 90 degrees or more of external rotation ROM on the injured side, however, none of these patients received the highest possible score on the SWA test, suggesting apprehension or possible limitations at the thoracic spine or with scapular movement. The SWA test may guide the clinician to examine both the thoracic spine and scapular movement to determine limitations in these areas if the patient has 90 degrees or more of shoulder external rotation ROM.
Change in ASES and WOSI scores exceeded thresholds for MCID, demonstrating clinical improvement over the six-week interval from initial to follow-up testing. The SWA test score demonstrated moderate associations with ASES and WOSI scores at initial testing and WOSI score at follow-up testing. These findings support the validity of the SWA test as being related to patient-reported shoulder function. It is possible that the SWA test was not associated with ASES score at follow-up testing because ASES score approximated the maximum score (ceiling effect). Additionally, the WOSI has been shown to be more responsive than the ASES in patients with shoulder instability.31–33 Interestingly, the shoulder mobility tests (total arc of motion and external rotation ROM) did not show association with the patient-reported outcome scores at initial testing, and the association between total arc of motion and WOSI score at follow-up testing was not retained in multivariate analysis. The authors are unaware of any other studies that have examined the association between total arc of motion and patient-reported shoulder function.
The strength of this study is the exploration of the SWA maneuver, commonly used as an intervention, to a novel clinical test with proposed scoring. The SWA test can be performed quickly in the clinic without special equipment and is less burdensome to the clinician than performing individual measurements of shoulder rotational ROM, thoracic posture and mobility, and scapular function. However, this study has limitations that must be acknowledged. First, the sample size is small and was further reduced for the analyses of shoulder external ROM due to missing data. Second, the patient population is limited to those with anterior shoulder instability and may not be generalizable to other patient groups with shoulder pain. Third, rehabilitation during the six-week study period was not monitored nor was scapulothoracic function, thoracic spine mobility, or scapular or rotator cuff muscle strength tested. Thus, the changes in the SWA test score cannot be interpreted to have occurred with respect to any clinical intervention or changes at the scapulothoracic joint, thoracic spine, or scapular and rotator cuff muscle strength. Future studies of the SWA test should include assessment of scapular stabilizer and rotator cuff muscle strength. Fourth, follow-up was based on time, not clinical milestones, and return to sport status was not recorded, so extrapolation of the study findings to return-to-sport decision-making is not appropriate. Finally, the position of the head was not standardized during testing. Adding criteria for head position may improve the reproducibility of testing.
CONCLUSION
The results of this study indicate that the SWA test distinguishes the injured side from the uninjured side, demonstrates a relationship with patient-reported outcome scores, and could augment clinical assessment of shoulder function alongside other shoulder mobility tests. These data provide initial evidence to support further examination of the psychometric properties of the SWA as a clinic test for future inclusion in functional testing batteries.
Conflicts of Interest
The authors report no conflicts of interest.