Introduction
Ankle sprains are a prevalent issue in sports medicine, accounting for approximately 25% of all sports injuries with 85% affecting the lateral side.1 These sprains affect 1 in 10,000 people per day.2 Ankle sprains represent the second most common cause of emergency room access, second only to low back pain.3,4 The ATFL and CFL are the most frequently injured ligaments during an ankle sprain and constitute a significant portion of sports-related traumas. About 33% of individuals experience reinjury within 3 years, and 25% develop chronic ankle instability.5 Some reports suggest an even greater re-injury rate of 70% at the ankle.6 Accurate diagnosis and early treatment are crucial in preventing long-term complications. While physical examination and radiography are traditional diagnostic tools, these methods have limitations in identifying soft tissue injuries and small avulsion fractures. Magnetic resonance imaging (MRI) and computerized tomography (CT) scans, despite their accuracy, are less frequently used due to high costs and time constraints. These limitations necessitate more effective alternatives. With the advent of MSK diagnostic ultrasound, a window has opened to diagnose and manage lateral ankle ligament injuries more accurately and efficiently and its diagnostic value has been previously described.7–9 Oae and colleagues have previously reported that lateral ankle injuries can be identified with MSK ultrasound with greater than 90% accuracy.10
Advantages of MSK Diagnostic Ultrasound:
-
Point of Care Utility: MSK ultrasound can be used in various settings, enhancing the clinician’s ability to make timely and informed decisions.
-
Accuracy and Precision: Ultrasound allows for a detailed view of the ATFL and CFL which allows for precise identification of injuries at the tender point and adjacent areas. This in turn provides clarity in diagnosing the extent of ligament integrity, tears, or sprains.
-
Cost-Effectiveness and Accessibility: Compared to MRI and CT, ultrasound is a more affordable and readily available option.
-
Real Time Dynamic Imaging: Real-time imaging enables dynamic assessment, crucial for understanding the functional impairment and precise localization of injuries. One advantage of the use of MSK ultrasound imaging is that the clinician can perform a real-time stress ultrasound, meaning a gentle varus stress force can be applied to the ankle while imaging and quickly compare that to the normal contralateral side. Rossi et al11 have shown that when performing ankle and foot sonography, the healthy contralateral side can safely be used as a reference during real-time MSK ultrasound evaluation of multiple structures.
-
Non-Invasive and Safe: Free from radiation, making it suitable for repeated use and in different patient populations.
Clinical Approach and Standardization: To ensure comprehensive and accurate diagnosis, a systematic approach to ultrasound scanning of the lateral ankle is necessary. Clinicians should:
-
Expand Examination Scope: To avoid misdiagnosis, MSK ultrasound scanning should not be limited to the ATFL and CFL but should include a broader examination of the lateral ankle. A wider area should be routinely examined to avoid missing associated injuries.
-
Combine with Physical Examination: Ultrasound should be used in conjunction with medical history and physical examination for a comprehensive evaluation. The thorough physical examination should guide the ultrasound imaging, focusing on tender points and specific ligament structures.
-
Advocate for Training and Standardization: There is a pressing need for standardized protocols for lateral ankle ultrasound scanning to ensure uniformity and accuracy in diagnosis. Standardized training for clinicians in the use of MSK ultrasound will help to promote uniformity and reliability in diagnoses.
Anterior Talofibular Ligament
The probe is placed in the transverse plane at the lateral ankle (Figure 1A and 1B). The lateral malleolus is clinically palpable, and the probe is placed at the most distal aspect of the lateral malleolus in the longitudinal axis of the foot. In this position, the ATF ligament can be seen. Deep in relation to the ligament, a small amount of joint fluid may be seen in the normal ankle. On anatomic slices, the ligament is seen as a bandlike structure extending from the distal fibula to the talus. The ligament is identified as a fibrillar hyperechoic structure that may show anisotropy artifact if the probe is not in the optimal plane of view.
Calcaneofibular Ligament
The probe is placed in an oblique coronal plane at the posterolateral ankle (Figure 1C). Oblique positioning is mandatory for exact localization of the ligament. The CFL is then seen extending from the fibula to the calcaneus. The peroneal tendons are in close proximity to the ligament and may help in precisely localizing the ligament. On MRI, the ligament is seen originating on the fibula and extending to the calcaneus with a course deep in relation to the peroneal tendons. The ligament may be seen as a hyperechoic fibrillar structure, again with the possibility of anisotropy artifact.
Implications for Rehabilitation: Incorporating MSK Diagnostic Ultrasound in rehabilitation:
-
Enhances Treatment Planning: Provides a detailed assessment that informs more tailored and effective treatment strategies.
-
Improves Patient Outcomes: Accurate diagnosis leads to better-targeted interventions, reducing the likelihood of chronic instability and recurrent injuries.
-
Facilitates Monitoring: Enables ongoing evaluation of the healing process, allowing adjustments in treatment as needed.
Conclusion
MSK Diagnostic Ultrasound significantly enhances the diagnosis and management of lateral ankle sprains, particularly involving the ATFL and CFL. Its accuracy, cost-effectiveness, and dynamic imaging capabilities make it a superior tool in the rehabilitation provider’s arsenal. Despite its advantages, the adoption of ultrasound in evaluating lateral ankle sprains is not without challenges, primarily due to the lack of standardization in scanning protocols and interpretation. There’s a need for systematic ultrasound examination of the lateral ankle to avoid misdiagnosis and overlooked injuries. By offering a comprehensive guide on the use of MSK diagnostic ultrasound, this article aims to equip rehabilitation providers with the knowledge and rationale to incorporate this technology into their practice, thereby improving the standard of care for patients with lateral ankle ligament injuries. As technology advances and accessibility increases, its integration into clinical practice is crucial for improving patient care and outcomes in musculoskeletal injuries.
Lateral Ankle Ligaments: Anterior Talofibular Ligament (ATFL) and Calcaneofibular Ligament (CFL)
Figures 1A and 1B: ATFL Patient Position and Transducer Placement
The patient can be supine on the exam table with the hip and knee flexed, and the ankle is in plantar flexion and inversion. The position allows for a static stress test to be applied to the ATFL. An alternative position would be for the patient lying supine with the hip and knee relaxed and the foot resting off the edge of the table. This second position provides allowance for dynamic inversion stress maneuvers to test the integrity of the ATFL ligament. The transducer is placed obliquely longitudinal/LAX on the anterior margin of the round, bony eminence of the lateral malleolus while the remainder of the transducer is placed on the talus.
Figure 1C: CFL Patient Position and Transducer Placement
The patient can be supine or prone on the exam table, and the foot may or may not be resting on a bolster to enhance the required dynamic dorsiflexion for optimal visualization of the CFL. Having the foot in a fixed dorsiflexion position will help place tension on the lateral tendons. The transducer will need plenty of gel (floated) and is placed on the inferior aspect of the lateral malleolus. The angle is considered an obliquely longitudinal/LAX orientation on the anterior-inferior margin of the fibular/lateral malleolus while the remainder of the transducer is placed on the calcaneus angled slightly posterior.
NORMAL VIEW IN OBLIQUE LONGITUDINAL AXIS (LAX): ANTERIOR TALOFIBULAR LIGAMENT (ATFL)
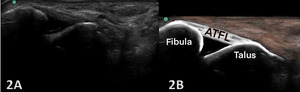
Figures 2A and 2B Oblique Longitudinal/LAX Axis View: Careful transducer placement spans the joint between the proximal fibula and the distal talus. The fibers of the normal ATFL will extend between the bony landmarks in a linear, uniform appearance. The ligament interdigitates with the deeper, anterior joint capsule and may APPEAR to dip into the joint space.
NORMAL VIEW IN OBLIQUE LONGITUDINAL AXIS (LAX): CALCANEOFIBULAR LIGAMENT (CFL)
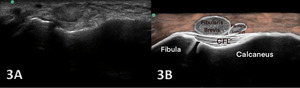
Figures 3A and 3B Oblique Longitudinal/LAX Axis View: Dorsiflexion of the foot tensions the CFL and makes the fibers more visible as they reach from the fibula to the calcaneus. The peroneal/fibular tendons are superficial to the CFL. A careful downward rotation of the probe from a SAX image of peroneal tendons is needed for a LAX of the CFL. A normal, intact CFL shows a curved course with an echogenic fibrillar structure located between the calcaneus and peroneal tendons. If the ankle is kept in a relaxed and static position, the CFL will look slightly concave. With ankle dorsiflexion and inversion, the CFL is being stretched and will straighten resulting in a lifting up of the peroneal tendons a small amount called a “trampoline sign”. Lifting of the tendons and stretching of the ligament is a sign of ligament continuity.
COMPLETE TEAR OF ATFL
Figures 4A: LAX ultrasonography of the ATFL shows hypoechoic discontinuity of the ligament, compatible with a complete tear (blue arrows). An inversion stress image provides more diagnostic confidence regarding the complete tear. LM, lateral malleolus; Ta, talus
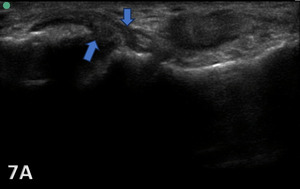
PARTIAL TEAR OF ATFL
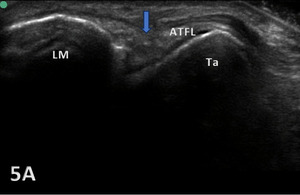
Figure 5A: The ATFL exhibits heterogeneous hypoechogenicity with some calcifications. This finding reveals a chronic partial tear (blue arrow). ATFL, anterior talofibular ligament; LM, lateral malleolus; Ta, talus.
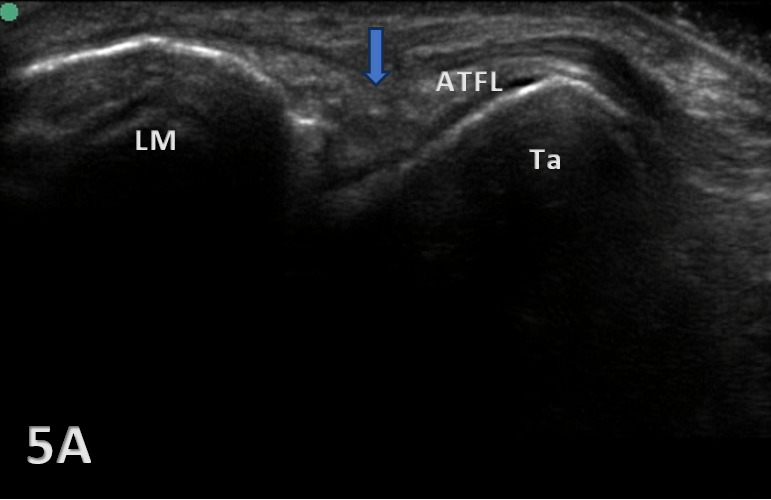
COMPLETE TEAR OF CFL
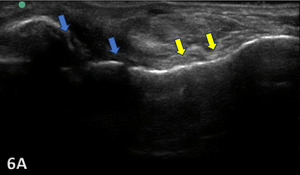
Figure 6A: Complete tears might show anechoic defects (blue arrows) of the CFL along with a hypoechoic and wavy appearance (yellow arrows) of the torn ligament.
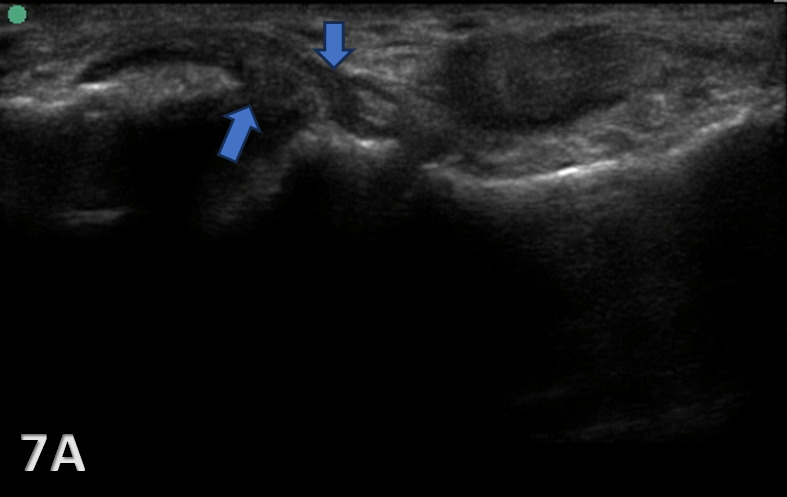
PARTIAL TEAR OF CFL
Figure 7A: The CFL will be hypoechoic and thickened or swollen in case of a partial tear and sprain (blue arrows). Partial tears might show anechoic defects and undulated or irregular ligament fibers.