INTRODUCTION
The triceps brachii tendon, an integral component of the elbow’s musculotendinous system, plays a crucial role in arm extension. Tears of the triceps brachii tendon can lead to significant disability related to loss of elbow extension strength.1 Diagnosis can pose challenges in the clinical setting due to the nature of triceps injury presentation; partial-thickness tears tend to selectively involve the superficial layer of the tendon, leaving the deep layer intact.1 This means that patients with significant tendon tears may still be able to generate sufficient elbow extension force during manual muscle testing, which may obscure the severity of tissue injury.2
Imaging evaluation is often necessary to assess the extent of triceps tendon injury. While radiography is the initial choice for acute elbow injuries, it falls short in assessing soft tissue structures. Magnetic resonance imaging (MRI) excels in soft tissue evaluation; however its accessibility may be hindered by cost, availability, and contraindications.3 In high-grade acute triceps tendon injuries, optimal outcomes are suggested when surgical repair occurs within three weeks of injury onset.1 Therefore, timely diagnosis is crucial in order to facilitate appropriate orthopedic referral.
Musculoskeletal ultrasound (MSK US) can be advantageous in diagnosing triceps brachii tendon injuries due to its capacity for high-resolution, real-time imaging in the clinical setting. While soft tissue contrast is inferior to MRI, ultrasound generates a greater spatial resolution and allows for dynamic assessment of acute muscle and tendon injuries.4 It is adept at detecting changes in tendon tissue composition and integrity, particularly the characteristic sonographic appearance of tendinopathies and partial-thickness triceps tendon tears.5,6 It can also identify tendon retraction and bone fragments, such as with tendon avulsion from the olecranon.6
The purpose of this case report is to describe how MSK US was used to facilitate advanced imaging and timely orthopedic referral for a patient presenting to the physical therapist with a high-grade partial thickness triceps tendon tear.
CASE DESCRIPTION
A 35-year-old male soldier presented to a direct access sports physical therapist (PT) for worsening right posterior elbow pain. The subject’s pain began several months prior concurrent with an increase in upper body strength training activities and was gradually worsening in severity with this activity. The subjects’s history included a right partial triceps brachii distal tendon avulsion eight years prior which was treated conservatively, allowing him to resume unlimited military duty and weightlifting activities in subsequent years. The subject denied red flags including experiencing a new traumatic event, joint swelling, or signs of infection.
Physical examination noted a palpable defect and mild tenderness on the posterior aspect of the elbow at the insertion of the triceps tendon. There was no ecchymosis, erythema, or edema appreciated. Triceps strength (manual muscle test 5/5), elbow range of motion (0-135 degrees), and elbow stability (varus and valgus stress tests) were intact and asymptomatic. Differential diagnoses included triceps strain, triceps tendinopathy, olecranon bursopathy, and symptomatic osteoarthritic changes.
MSK US was performed by the physical therapist using a Sonosite IViz (Fujifilm Sonosite, Bothell, WA) with portable 10-5 MHz 38 mm linear array transducer with the subject lying in supine. The shoulder was positioned in internal rotation with the elbow flexed to ninety degrees and elevated on a bolster so that the hand could rest on the abdomen (Figure 1). The probe was positioned in the sagittal plane over the distal triceps and posterior elbow and maneuvered until the bony landmarks of the olecranon process of the ulna and the distal humeral cortex were visualized. The triceps tendon and portions of the myotendinous junction were visualized superficial to the bony landmarks.6,7
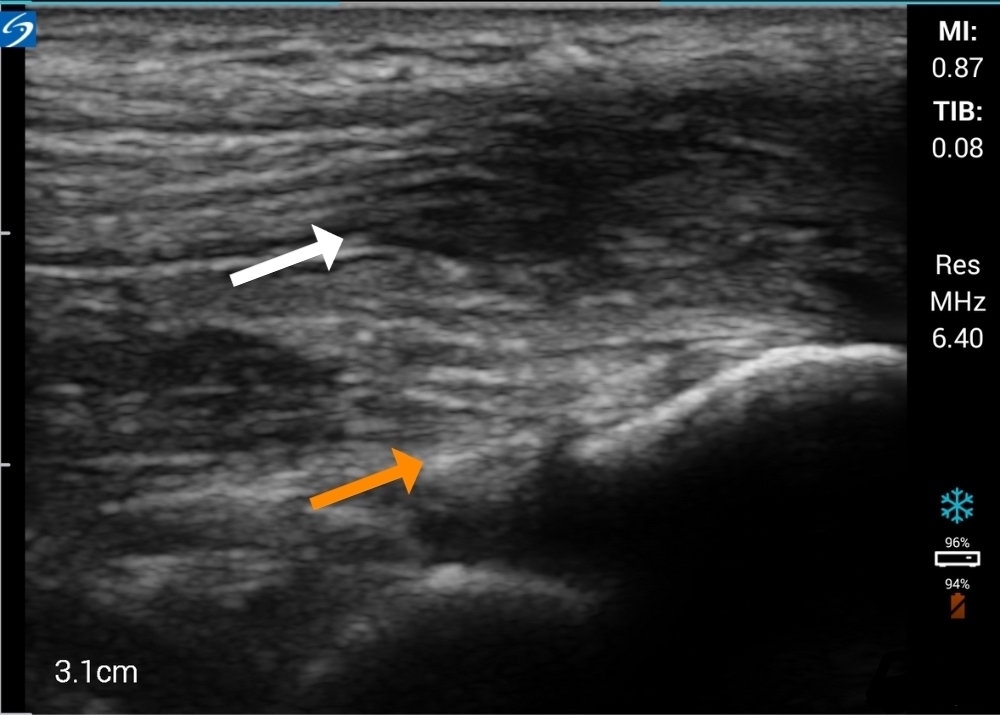
The long-axis ultrasound view demonstrated a thickened distal triceps tendon with a loss of normal fibrous echotexture (Figure 2). There was hypoechogenicity of the superficial layer of the conjoined tendon compared to the deep portion and a loss of the normal tendon tapering conformity at the insertion on the olecranon process. Tendon thickening, hypoechogenicity, and a loss of normal fibrous echotexture are findings consistent with chronic tendinosis.8
A week later, prior to initiating a care plan, the subject reported re-injury while performing resisted elbow extension strength training exercises. Physical examination revealed moderate elbow effusion with a more prominent palpable triceps tendon defect. Triceps strength was 3+/5 through the available range of motion of 15–125 degrees. Differential diagnoses included acute triceps tendon tear, triceps tendon avulsion, and olecranon fracture.
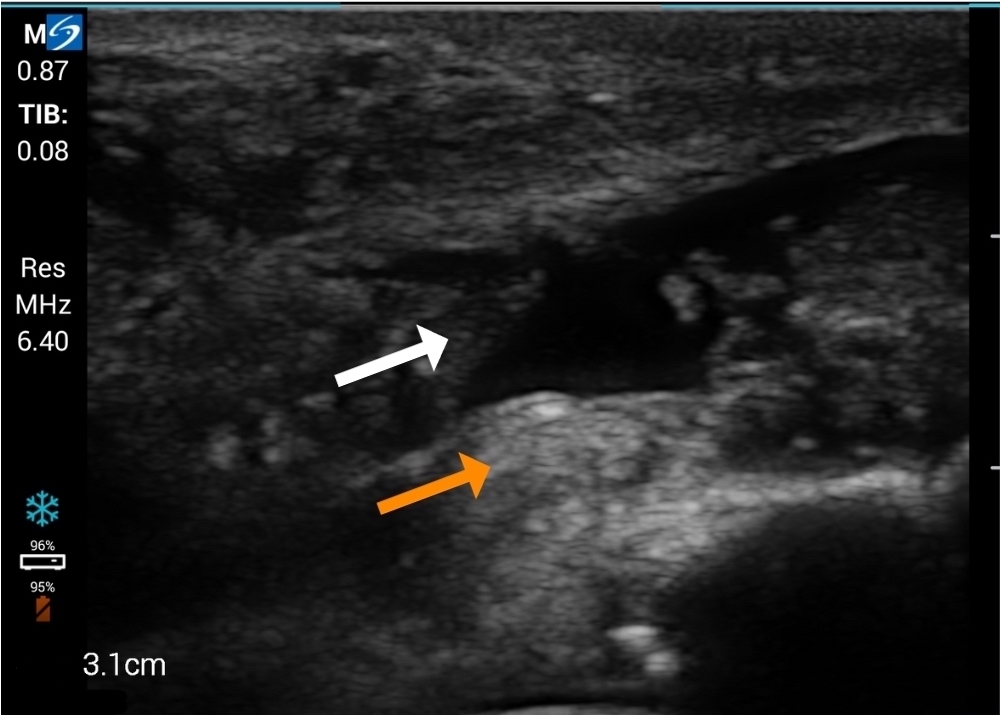
Immediate post-injury MSK US demonstrated a selective area of complete fiber non-visualization of the distal triceps tendon’s superficial portion near its insertion on the proximal ulna, indicating a high-grade partial tendon avulsion (Figure 3). The subject was referred by the physical therapist for MRI two days later. MRI findings confirmed a partial triceps tendon avulsion with a partially retracted conjoined tendon of the long and lateral heads of the triceps and tendinosis (Figure 4).
OUTCOME
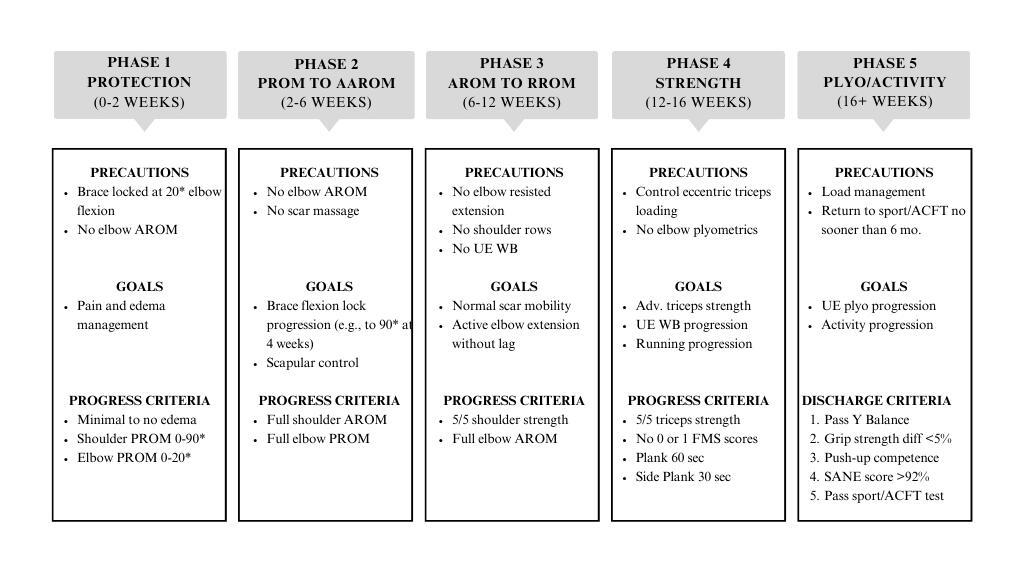
The subject was referred to an orthopedic surgeon and underwent a distal triceps repair within the recommended three-week timeframe from injury.1 Post-operative rehabilitation was informed by the clinical practice guideline for distal triceps repair by Hock.9 Return to duty/sport and physical therapy discharge criteria were informed by the guidelines of Plisky et al. for upper extremity injuries.10 Early rehabilitation phases were timeline-based per the clinical practice guideline; later phases transitioned to criteria-based upper extremity testing to prepare the subject for return to full military duty, including competence on the Army Combat Fitness Test (ACFT).11 An overview of the rehabilitation program is summarized in Figure 5.
The subject successfully completed the rehabilitation program and returned to full active military duties, including heavy strength training and ACFT performance, at eleven months postoperatively. He continued to report pain-free physical and occupational capabilities upon follow-up at two years post-surgery.
DISCUSSION
The purpose of this case report is to describe how MSK US was used to facilitate advanced imaging and timely orthopedic referral for a subject presenting to the physical therapist with a high-grade triceps tendon tear. To the authors’ knowledge this is the first case report to include both pre- and post-injury MSK US imaging of an acute triceps injury. While high grade triceps tears are relatively rare injuries,6 they occur most frequently in athletic and physically demanding occupational populations12 where physical therapists and other sports medicine professionals may serve as the first point of triage and care. As delayed recognition and subsequent surgical care may lead to suboptimal outcomes in high grade triceps tendon injuries,1 MSK US offers several advantages in their assessment.
First, MSK US aids the assessment of injury severity compared to physical examination alone. As demonstrated in this case report, clinical examination findings may not accurately reflect the extent of tissue damage, particularly in partial-thickness tears where active elbow extension is preserved.2 As an extension of the physical examination in this case, MSK US provided clinical utility through real-time visualization of tendon integrity to further define the severity of injury at the initial point of care.
Due to advances in technology, MSK US may provide field-expedient access to initial imaging that is not readily available with other imaging modalities, such as MRI. This feature may be particularly useful in settings where immediate assessment and management decisions are necessary in order to optimize patient outcomes. In the present case report, rapid determination of injury severity was crucial to inform both the subject and their military leadership of recommended limitations to work responsibilities in order to ensure safety. Unlike MRI, which often requires scheduling appointments, travel considerations, and may be subject to availability constraints, ultrasound was performed at the point of care, facilitating rapid diagnosis and expedited referral. Timeliness of diagnosis was particularly advantageous to the subject of the present case report, where prompt surgical planning and early surgical intervention was indicated to optimize outcomes.1
Additionally, MSK US enables ease of repeated examination in real-time and as a patient’s presentation evolves. In the current case report, while the change in clinical examination findings from initial encounter to re-injury may have been sufficient to prompt early orthopedic referral, the change in triceps tendon integrity as visualized on US reinforced the need to expedite this subject’s care plan. MSK US can also be used to provide ongoing assessment throughout the rehabilitative process. Dynamic assessment of tendon function, response to stress maneuvers, and surveillance of tendon healing over time are capabilities of MSK US that may be advantageous for assessing treatment response and guiding more personalized rehabilitation and management strategies.5
Despite these advantages, there are several limitations to the use of MSK US in the diagnosis and management of triceps tendon injuries. Compared to MRI, MSK US provides greater spatial resolution however its soft tissue contrast capabilities are inferior.4 MSK US lacks validity compared to the gold standard of MRI in the diagnosis of triceps tendon injuries. This limitation may be attributed, in part, to the paucity of the imaging literature addressing triceps tendon tears.6 While other upper extremity tendons, such as the rotator cuff, have shown acceptable agreement between MSK US and MRI findings,13 to the authors’ knowledge there are no studies in the current literature specifically addressing the triceps tendon beyond case studies.
MSK US imaging is also limited to a visual window commensurate with the physical size of the ultrasound transducer. As such, ultrasound can provide a focused and relatively superficial examination but cannot provide a global assessment of the injury region, potentially missing concomitant pathologies pertinent to a patient’s presentation.8 While the subject in the present case report sustained a non-contact re-injury to a small area of previously known pathology, a different, traumatic mechanism of injury, common in both military and athletic populations, would require an imaging window beyond the local capabilities of ultrasound.
The upfront costs associated with implementing MSK US into clinical practice, while considerably less than MRI, can present a significant barrier to its widespread adoption. Despite the advances in portable US devices the upfront technology costs are likely to exceed $10,000 which may pose a significant financial challenge to small physical therapy teams and those with limited resources. Obtaining the necessary expertise in musculoskeletal ultrasound interpretation requires specialized training, which may not be readily available to all clinicians. Furthermore, the experience and skill of the ultrasound operator significantly influence the accuracy and reliability of the examination. Interpretation of ultrasound images relies heavily on the operator’s proficiency in probe manipulation, image optimization, and recognition of anatomical structures. Inexperienced operators may struggle to identify subtle abnormalities or may misinterpret normal variations as pathological findings, leading to diagnostic errors and potential delays in appropriate management.
While MSK US has inherent disadvantages compared to MRI, including limitations in validity, upfront costs, and operator dependence, its advantages in providing field-expedient assessment of injury severity and enabling ease of repeated examination made it a valuable diagnostic tool in the evaluation of triceps tendon injuries. In the present case report, MSK US aided in the rapid assessment of triceps tendon injury severity, prompting rapid referral and treatment in order to optimize the subject’s outcomes.
SUMMARY
As active elbow extension is often preserved in cases of triceps tendon avulsion, high-grade injury cannot be ruled out by clinical examination alone. Timely diagnosis of high-grade injuries can facilitate optimal surgical outcomes within the recommended three-week timeframe from injury. MSK US may be a valuable tool in these cases, due to its high-resolution visualization and ability to provide real-time assessment of tendon injuries. MSK US may also play a role in enhancing physical therapist decision-making for advanced imaging studies and time-sensitive orthopedic referral to optimize treatment outcomes.
Disclosure
The opinions and assertions contained herein are those of the authors and are not to be construed as official or reflecting the views of the US Army Medical Department, the US Army, or the Department of Defense.
The authors have no conflicts of interest to report.