Introduction
Greater trochanteric pain syndrome (GTPS) is a prevalent hip condition characterized by lateral hip pain, dysfunction, and diminished quality of life.1 GTPS is considered a multifaceted condition that encompasses pain originating from various traumatic and degenerative changes within the peritrochanteric space, including the tendons, bursae, and trochanteric bone structures.2,3 The etiology of this condition encompasses a broad spectrum, including trauma, infection, avascular necrosis, stress fractures of the femoral neck, and referred pain originating from the spine. Moreover, conditions such as arthritis, tumors, and entrapment neuropathies are also documented contributors to lateral hip pain.2 A subset of patients may experience this pain due to tendinopathy of the gluteus medius and minimus muscles, a condition initially proposed by Schein and Lehmann, who attributed calcifications near the greater trochanter observed in radiographs to injury or degeneration of the gluteus medius tendon.4 Subsequent research by Gordon in 1961 linked trochanteric bursitis to the attachments of the gluteus tendons, proposing a secondary involvement of adjacent bursae akin to the relationship between the rotator cuff and subacromial–subdeltoid bursitis.5 The terms “gluteus tendinopathy” or “greater trochanteric pain syndrome” are now preferred over “trochanteric bursitis,” given the frequent absence of the latter.
This syndrome, which primarily affects the gluteus medius and minimus tendons, represents the most common tendinopathy of the lower limb, with an annual incidence rate ranging from 1.8 to 5.6 per 1,000 individuals.3,6 This pathology typically manifests unilaterally in middle-aged women, particularly those in their fourth through sixth decades of life, and its prevalence escalates with age.3 GTPS is characterized by a dull ache and tenderness on the lateral aspect of the hip, worsened by weight bearing and impairing the ability to sleep on the affected side. The impact of gluteal tendinopathy on function and quality of life is comparable to the effects of end-stage hip osteoarthritis.7
The diagnostic process for GTPS integrates clinical history, palpation, and specific physical examination maneuvers, with magnetic resonance imaging (MRI) serving as the definitive modality for confirming the diagnosis.3,8 Differentiating among these conditions presents a challenge due to the complex morphology of the hip region and the presence of significant adipose tissue overlaying the greater trochanter.1 MRI is regarded as the definitive diagnostic tool, revealing changes in tendon insertions at the greater trochanter, muscle atrophy, and bursal distension.3,8 Despite MRI’s status as a gold standard for diagnosing GTPS, MSKUS imaging has shown considerable efficacy, particularly for early-stage detection of gluteal tendinopathy and other peritrochanteric pathologies, due to advancements in diagnostic capabilities. Westacott et al. highlighted the comparative diagnostic accuracy of MSKUS and MRI in detecting gluteal tears, with MSKUS showing superior sensitivity.8 However, the study primarily focused on tears, without addressing tendinosis or distinguishing between tear types. Docking et al. investigated the ability of MRI and MSKUS to identify the presence of a a pathological gluteus medius tendon in comparison to surgical and histological findings.1 MSKUS identified 17 out of 19 pathological gluteus medius tendons correctly. However, 5 of the 6 normal tendons were incorrectly identified as exhibiting pathology on ultrasound. MRI rated 11 out of 17 pathological tendons as abnormal, with 4 out of 6 normal identified correctly. This study demonstrated that MSKUS can be used reasonably to detect gluteus medius tendon pathology. The limitations in imaging’s capacity to differentiate between tendinosis and partial-thickness tears are further exemplified in studies of the Achilles and shoulder rotator cuff tendons, underscoring the need for refined diagnostic criteria and methodologies in the evaluation of GTPS-related pathologies. Research indicates a significant incidence of gluteal tendon abnormalities in asymptomatic individuals, with findings of gluteal tendinosis or partial tears in up to 50% of evaluated hips.9–11 Despite this, there remains a scarcity of studies focusing on the diagnostic precision of imaging techniques in identifying and distinguishing structural abnormalities within the gluteal tendons.
Principles of Musculoskeletal Ultrasound
MSKUS employs high-frequency sound waves to produce images of soft tissues, joints, and bones. The principal advantages include real-time imaging capabilities, absence of ionizing radiation, and the ability to conduct comparative assessments of the affected and contralateral sides. Furthermore, its portability and lower cost relative to MRI make it accessible in various clinical settings.
Technique and Findings
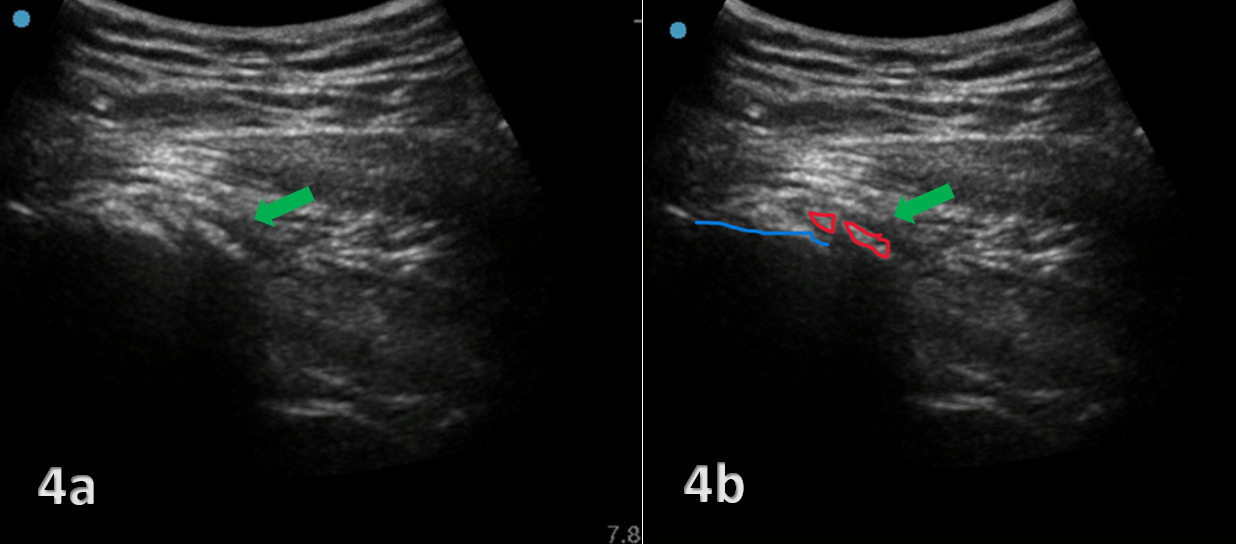
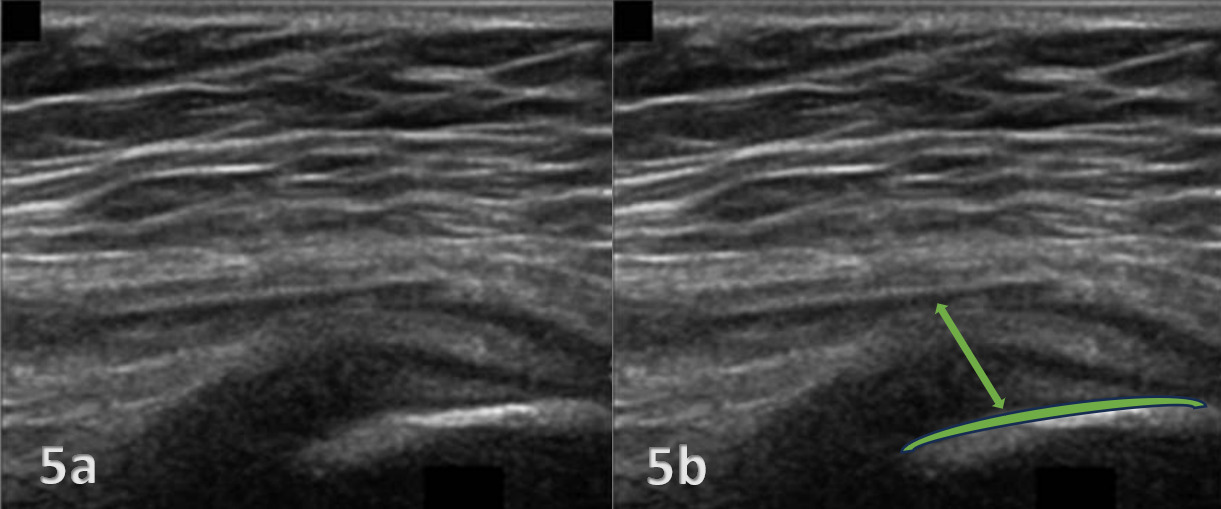
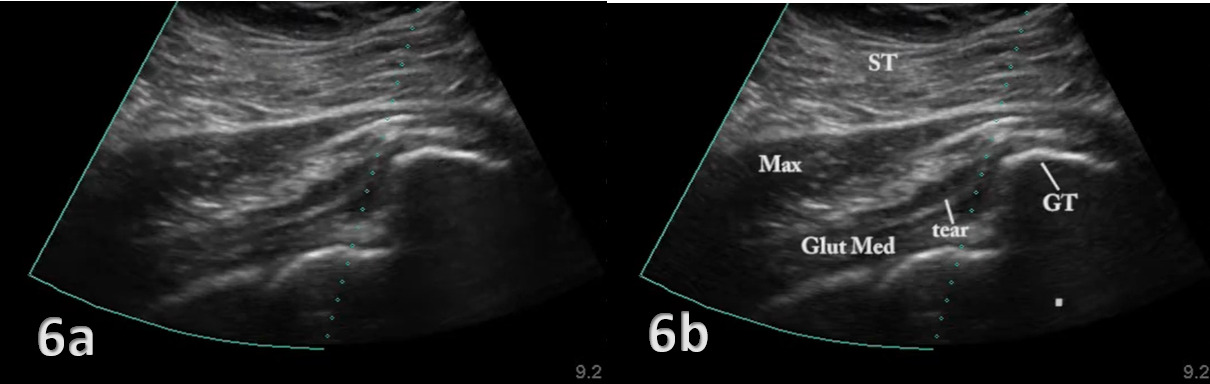
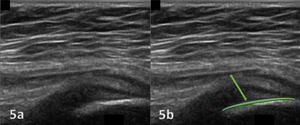
The evaluation of the gluteus medius tendon with MSKUS begins with the patient in a lateral decubitus or standing position, targeting the lateral aspect of the hip. The normal gluteus medius tendon appears as a fan shaped fibrillar structure composed of hyperechoic, striated fascicles with bright, linear bands running within the muscle.2 Pathological changes such as tendinopathy are characterized by hypoechoic (darker) regions within the tendon, tendon thickening, and loss of the normal fibrillar pattern. Tears are identified by discontinuity in the tendon fibers, with partial tears showing as anechoic (black) areas and complete tears as a full separation of the tendon from its insertion.
Clinical Implications
The ability of MSKUS to visualize these pathological changes in real-time provides immediate feedback that can inform treatment decisions. Rehabilitation providers can use this information to tailor exercise programs, guide manual therapy techniques, monitor the progression of tendon healing over time, or refer to another provider in instances of tears or ruptures that may require further imaging or surgical intervention. Additionally, ultrasound-guided interventions, such as injections, can be performed with greater accuracy and safety.
Advantages and Limitations
While MSKUS offers several advantages, including patient comfort and dynamic assessment capabilities, it also has limitations. Operator dependency, a steep learning curve, and variability in image interpretation are notable challenges. Therefore, comprehensive training and experience are essential for maximizing the diagnostic utility of this modality.
Conclusion
Diagnostic MSKUS represents a valuable adjunct in the evaluation of gluteus medius tendon pathology for rehabilitation providers. By facilitating an accurate and detailed assessment of tendon condition, it supports more informed clinical decision-making and personalized patient care. As technology advances and proficiency in MSKUS techniques grows within the rehabilitation community, its application in clinical practice is likely to expand, further enhancing the management of musculoskeletal conditions.

.png)
.png)


.png)
.png)