INTRODUCTION
The Anterior Cruciate Ligament (ACL) is one of the most commonly injured ligaments in the body with as many as 200,000 ACL injuries occurring each year in the United States.1 The injury rate for females is nearly double that of males, 2.10 compared 1.12 respectively per 10,000 athletic exposures. The injury rate increases to 4.80 per 10,000 athletic exposures for athletes in fixed-object high impact rotational landing sports such as gymnastics.2 The gold standard for treatment over decades has been an ACL reconstruction using either autografts or allografts.1,3
Some researchers suggest the ACL has potential to heal without reconstruction for acute tears that occur in the proximal ACL.4–6 Specifically, Sherman type 1 ACL tears (proximal avulsions of the ACL at the femoral attachment) may benefit from an ACL repair with internal bracing.7 The advantages include decreased donor site morbidity pain and weakness, maintaining proprioception of the native ACL , earlier recovery, minimizing osteoarthritis, and fortification of the repair with biological healing of the proximal ACL.8–11 There are a number of different surgical techniques utilized to repair the ACL including: Suture Anchor Repair (SAR), Internal Brace Ligament Augmentation (IBLA), Dynamic Intraligamentary Stabilization (DIS), or Bridge Enhanced Anterior Cruciate Ligament Repair (BEAR).1 Attempts at repairing the ACL have been used since the 1970's, but were previously associated with less than favorable outcomes including a high failure rate in athletes and long periods of immobilization.12 Since then, improved surgical techniques and appropriate patient selection have demonstrated favorable results in terms of subjective and objective outcomes while restoring function in patients who receive a primary repair compared to those with an ACLR.13–16
The surgical technique described in this case report involves an ACL repair using IBLA. It is suggested the use of IBLA in conjunction to repairing the ACL preserves the native proprioceptive fibers of the ACL while acting as a secondary stabilizer.14,17 IBLA consists of an ultra-high strength 2mm wide synthetic polyethylene tape as an internal brace to provide additional external support to bridge the healing ACL from tibia to femur.14,18,19 In addition to the anatomical repair, the IBLA is reinforced with femoral fixation via a button anchor, while the tibial fixation is held with a knotless bone anchor.18 The internal brace acts as secondary stabilizer, reducing elongation and peak loads on the ACL repair, restricting gap formation to less than 3mm at loads up to 350 N.20 This is crucial in stabilizing the ACL from loads that occur through daily activity while allowing for an earlier progression through the rehabilitation protocol compared to an ACLR.14,17,20
Variability exists in the literature regarding an appropriate rehabilitation progression in terms of bracing, range of motion (ROM) restrictions, exercise progression, and return to sport for patients who undergo an ACL repair, specifically those with internal bracing. The ACL repair is gaining popularity as a potential treatment alternative for acute ACL ruptures.14 Therefore, there is a need for surgeons and physical therapists to collaborate and provide technique specific rehabilitation guidelines for these procedures. The purpose of this case report is to provide an example of a rehabilitation progression used for a high-level female gymnast after an ACL repair with IBLA.
CASE DESCRIPTION
The subject was a 16-year-old female who was actively competing in high level gymnastics and was committed to a Division 1 gymnastics program. The subject originally hurt her right knee roughly four weeks prior, while competing in a gymnastics event. She was performing a twisting double Salto dismount on the bars, when the side of her tibia collided with the upper bar, resulting in knee pain as she landed on her injured leg. She attempted to continue competing the same day and over the next week, but consistently experienced pain, clicking and persistent swelling in her knee. She reported developing a mild extension deficit which inhibited her ability to compete. Three weeks after her injury, the subject sought out care. An MRI was obtained which revealed a disruption of the anterior cruciate ligament, avulsed from the femoral attachment. After all treatment options were provided to the subject and her mother, they elected to proceed with a right knee ACL repair with internal bracing for an expedited return to sport.
Outcome Measures
The subject was examined at baseline prior to treatment, and then re-examined every four weeks until discharged from physical therapy. Performance measurements were obtained every eight weeks, starting at week eight post-operatively and continuing until discharged from therapy.
Patient Reported Outcomes
To measure symptoms, function, and sports activity the International Knee Documentation Committee (IKDC) Subjective Knee Form was used. It is a reliable and valid knee-specific questionnaire that is appropriate for patients with a wide variety of knee problems.21–23 The IKDC consists of 18 questions (7 items for symptoms, 1 item for sport participation, 9 items for daily activities, and 1 item for current knee function). The score ranges from 0 to 100, where 100 indicates no limitation with daily or sporting activities and the absence of symptoms.23 Irrgang et al. determined that the normal rating of knee function for those who have undergone an ACLR was an IKDC score of 95.2, nearly normal was 91.2, abnormal was 84.9, and severely abnormal was 75.4. In addition, based on test-retest reliability, the MCID is 11.5 points.21–23
The Anterior Cruciate Ligament Return to Sport After Injury (ACL-RSI) scale is a reliable and valid tool for evaluation of psychological readiness to return to sport after ACL injury.24 The ACL-RSI consists of three domains: emotions, confidence, and risk appraisal. Scores for each domain are summed and averaged for a total score between 0 and 100. Higher scores indicate greater psychological readiness.24 The shortened version of the scale, which contains six of the original items, was the version used in this study. Webster et al. found a cutoff score of 60 on the short version, when assessed at six months post-operatively, having a high specificity and moderate sensitivity that the athlete will return to their preinjury level of sport by 12 months.25 In another study Webster et al. also determined the minimally important change (MIC) on the short form was 15.1 points.24
The Optimal Screening for Prediction of Referral and Outcome Yellow Flag (OSPRO-YF) tool which assesses negative mood, fear-avoidance, and positive coping was used.26 This tool is a reliable and valid multidimensional psychological assessment tool for individuals with musculoskeletal pain.26 The OSPRO-YF assesses 11 psychological constructs within three broad psychological domains including: self-efficacy and acceptance (pain self-efficacy, rehabilitation self-efficacy, and chronic pain acceptance), negative pain coping (fear avoidance beliefs surrounding work and physical activity, pain catastrophizing, kinesiophobia, and pain anxiety), and negative mood (depression, anxiety, and anger).27 Based on patient responses, the OSPRO-YF generates a score estimate for each of the 11 constructs. Scores above the 75th percentile in negative pain coping or negative mood constructs or below the 25th percentile in self-efficacy/acceptance constructs are marked with a “yellow flag” for their respective domains.27 A summary OSPRO-YF score for a patient is a simple count of the number of constructs with yellow flags.27 The higher the number of yellow flags indicates higher pain associated distress and can help understand the patient's treatment response and overall pain experience.
Performance Measures
To objectively test muscular strength and performance, a battery of tests was used to help assess physical preparedness for return to sport. Performance testing included both strength and hop testing, but only strength testing was assessed during the original eight-week measurement. Isokinetic strength testing was measured at 60 deg/sec, using the Biodex System 3 dyanamometer. In addition, hop testing included single leg hop, single leg triple hop, and single leg cross-over hop. Historically, a Limb Symmetry Index (LSI) of 90% or greater between limbs following ACL reconstruction has been regarded as satisfactory for both strength and hop performance.28 Buchanan et al. studied females aged 15-17 years old and suggested that they have a strength to bodyweight ratio of 70%, which was the goal for return to sport for this athlete.29
Surgical Procedure
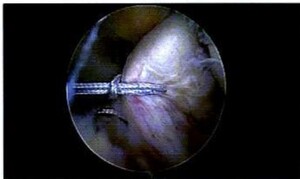
During the procedure, the initial arthroscopic findings revealed that the subject 's ACL was partially torn with posterolateral bundle laxity and the anteromedial bundle avulsed from femoral footprint. (Figures 1 and 2) Her PCL was intact, and there was no other significant pathology in the patellofemoral joint or the medial and lateral compartments.
The surgical description was as follows: The standard lateral portal site was created, and the knee joint was surveyed in the usual fashion with the arthroscopic findings mentioned above. Under direct visualization, the medial parapatellar portal was created. The physician then turned their attention to the ACL repair.
The central aspect of the ACL footprint on the femur was identified to place several evenly spaced holes in the notch, including, a large imprint at the center of the ACL footprint to prepare for drilling. Then, a passing pin was drilled into the center of the ACL footprint in the notch and out the lateral aspect of the femur. Following the placement and removal of a tibial guide and cannulated pin, a wire lasso was then loaded through the cannulated pin and pulled out of the anterolateral portal. A passport cannula was placed in the anteromedial portal. The FiberRing (Arthrex) was then loaded and pierced through the mid-substance of the ACL. (Figure 3) The free end was loaded through the loop and the suture was cinched on itself. This process was repeated twice for a total of two sutures through the stump of the ACL. The sutures were then loaded on the tightrope. (Figure 4) The tightrope sutures were shuttled out through the lateral femur and the button flipped on the lateral femoral cortex. The shortening strands were then pulled to hoist the ACL stump towards the femoral footprint. (Figure 5)
Examination
The subject was referred to physical therapy the day following her ACL repair. The subject ambulated with standard axillary crutches and a knee immobilizer, weight bearing as tolerated (WBAT) with a step-to gait. She reported decreased daily function, increased knee pain, and altered quality of life during the subjective portion of her evaluation evidenced by patient reported outcomes (PROs). During the initial evaluation, post-op dressings were removed, and new dressings were applied. The subject presented with moderate 2+ swelling and the incisions were stabilized by sutures and were clean and dry. There were no signs of infection and the subject reported tenderness to palpation around the surgical incisions. Her post-operative pain was rated a 4/10 on the numeric pain rating scale (NPRS) during evaluation, but at its worst the subject would rate her pain as 8/10. She described the pain as sharp and throbbing, along with feelings of perceived weakness and instability. Objective measures were taken and are listed in Table 1. Her primary goal for therapy was to compete nine months later in her upcoming gymnastics season.
Clinical Impression
This subject presented with typical post-surgical limitations including functional limitations in terms of strength deficits, ROM limitations, pain, joint inflammation, and gait abnormalities. She did not demonstrate signs of any other red flags that would warrant further medical attention or referral. The subject in this study completed physical therapy two times per week. She was given a home exercise program of similar exercises to be completed on days not in clinic.
Interventions
While evidence is limited, it has been accepted that the ACL is inherently stable following repair with IBLA.30 Therefore, only a short period of bracing is recommended until quadriceps control is restored. In addition, obtaining full knee extension is a top priority along with progressively increasing knee flexion.30 Early weight bearing is recommended as it allows the joint to begin tolerating loads in a safe manner with the use of crutches.19 As the subject progresses through rehabilitation, there is consistency across the literature that the use of IBLA allows return to running as early as three months post-operatively. However, the subject must demonstrate appropriate strength and psychological readiness through objective testing and PROs, similar to those used for ACLR.18,19,31 Lastly, based on current literature, sport specific training can begin between 17 and 20 weeks postoperatively and should continue until the subject demonstrates the appropriate functional capacity to progress to full return to sport (RTS), passing similar criteria used for an ACLR.19,31
Prior to beginning physical therapy, the therapists (CH, GZ) and physician (MM) discussed the proposed protocol below including any precautions, time-line restrictions, and criteria for advancement through the phases.
Phase I – Protective Phase (Days 1 –7)
The focus of this phase is to restore normal ROM, particularly full knee extension, which is critical to attain early in the rehabilitation process to achieve long term success and to return to sport.32,33 In addition, there is a large emphasis on maintaining quadriceps and gluteal activation during this phase, while also working to restore ambulation without compensations or the use of an assistive device.34ACL deficient patients can develop a habit of walking with a flexed knee gait, potentially complicating the restoration of the tibiofemoral and patellofemoral biomechanics.33,35
The first day of treatment consisted of restoring knee extension via a heel prop exercise. Other exercises to restore ROM included ankle pumps, patellar mobilizations and heel slides. Isometric quadriceps sets were initiated to begin restoring quad activation. Education consisted of pain and swelling management techniques including icing, compression via an ace wrap, and elevation. Furthermore, post-surgical precautions were emphasized including keeping the incision drying during bathing, sleeping in the knee immobilizer, and using the crutches and knee immobilizer during all ambulation. In the days following, straight leg raises (SLR) into flexion and abduction with the knee locked in extension via the knee immobilizer were initiated to continue restoring strength in the quadriceps and gluteal muscles. Neuromuscular Electrical Stimulation (NMES) is a modality that causes the muscles to contract mimicking the action potential coming from the central nervous system.36 NMES is used to build muscle activation and prevent atrophy, especially with immobilized patients.35,36 NMES was incorporated in conjunction with the isometric quad sets and SLR into flexion exercises to assist in restoring quadriceps strength. The Excel Multi IV (Excel Tech LTD, Oakville, Ontario, Canada). electrical stimulation machine was used with an amplitude that produced a tetanic muscle contraction, using a ramp of three seconds along with an on: off ratio of 10 seconds: 30 seconds, and a total treatment time of 15 minutes. The subject was educated on the proper gait sequencing, emphasizing a heel to toe gait using bilateral crutches while in the knee immobilizer. The criteria required to progress to the next phase of rehab consisted of achieving a knee extension within 5° of opposite leg, obtaining > 90 degrees of knee flexion, and demonstrating the ability to perform a strong quadriceps set and a SLR without quadriceps lag. (Appendix 1)
Phase II – Early Mobility (Week 2 - 3)
This next phase of rehabilitation continued to build upon the previous. The knee immobilizer and crutches were removed once the subject could demonstrate quadriceps control via repetitive SLRs without lag, full knee extension, and the ability to ambulate without gait compensations. ROM remained a primary focus with the goal of maintaining full knee extension compared to the contralateral side while progressing knee flexion to >110° flexion. The subject began using the recumbent bike for cardiovascular exercise and to facilitate knee flexion once she demonstrated >105 degrees of active assisted knee flexion. SLRs were progressed via load using ankle weights. Closed kinetic chain (CKC) exercises were used to continue building strength and proprioceptive capacity in the quadriceps and gluteal muscles of the involved lower extremity. Exercises included: leg press, mini-squats, terminal knee extension with resistance bands, calf raises, as well as forward and lateral step-ups and heel taps. Blood flow restriction (BFR) was used due to the ability to improve strength and hypertrophy with low loads.37 The subject performed the recommended repetition scheme of 30/15/15/15 with 45 seconds rest between sets and the cuff remaining inflated at 80% of occlusion.38,39 The total tourniquet time never exceeded 10 minutes in duration per session. BFR was used for several exercises including SLRs, leg press, and mini squats. To progress to the next phase, the subject had to demonstrate knee extension ROM equal to the opposite side and >110° of knee flexion, perform a SLR without a quad lag, and independently ambulate without an assistive device or compensations. (Appendix 1)
Phase III – Strengthening (Week 4 – 12)
The focus of Phase III is a continued progression from Phase II. The subject continued to focus on normalizing ROM to the uninvolved side. Loading in CKC was progressed in terms of load and depth to continue working on eccentric control.40 Step-ups and heel tap exercises progressed from 4 inch boxes to 12 inch by week 12. Open Kinetic Chain (OKC) exercises were initiated starting with knee extension, limiting knee flexion ROM from 90° to 40°, with low load and the weight at the proximal tibia at week six.41 Early knee extension exercises were performed with BFR with the parameters mentioned above. OKC knee extension progressed to full ROM by week eight. Proprioceptive drills evolved from Phase I with weight shifting, to single limb stance in Phase II, to performing balance exercises in single leg stance on a solid surface with the addition of external/ internal perturbations. This was further progressed by replacing the stable surface with an unstable surface without perturbations, and finally, perturbations were reintroduced while on an unstable surface. The next phase looked to progress the subject to straight line jogging and early plyometric activity. The criteria to progress the subject to Phase IV included: achieving ROM within 5 degrees of flexion and full extension equal to contralateral side, without complaints of patellofemoral symptoms, as well as isokinetic strength limb symmetry index (LSI) for quadriceps and hamstring strength >75% of the uninvolved side.31,42–44 By week 12 the subject demonstrated full knee flexion and hyperextension ROM compared to the contralateral side. The first round of performance testing was completed via isokinetic dynamometry via the Biodex at a speed of 60 deg/sec at week eight. The subject’s isokinetic strength measurements at 60 deg/sec demonstrated quadriceps strength LSI deficit of 40.1% and a hamstrings LSI deficit of 17.6%. In terms of normalizing her strength to bodyweight, she kicked at a ratio of 44% of her bodyweight. She remained in this phase until she demonstrated sufficient strength to tolerate light plyometric activity in Phase IV. (Appendix 1)
Phase IV - Light Plyometric/Return Running (3 – 4 Months)
The focus of Phase IV is to continue building strength within the lower extremity while also introducing the subject to light impact. Many of the same OKC and CKC exercises were performed without restrictions with the intent of increasing load per session. Jogging was initiated at week 13 which consisted of a walk: jog ratio starting at 1 min: 1 min for 10 minutes. This was repeated on three separate occasions with at least one day of rest between sessions prior to progressing to the next phase in the return to jogging program. Early plyometric activity consisted of double leg bounding on the leg press with an emphasis on equal push-off and equal soft landing while minimizing dynamic knee valgus. This progressed to a double limb push-off with a single limb landing to eventually single leg jumps on the leg press machine. Once the subject tolerated all plyometric activity on the leg press, land based plyometrics were introduced, starting in the sagittal plane, using both limbs. Over the course of Phase IV, plyometric activity progressed to include multiple planes of movement and from double to single limb exercises. (Figures 6,7,9 ( BlazePods (BlazePod LTD, Tel Aviv, Israel) were incorporated in later phases of plyometrics to improve reaction time and provide unpredictability to the environment. (Figure 8) The next phase consisted of agility and sport specific drills. The criteria to progress to Phase V included the ability to demonstrate a strength LSI of quadriceps strength >80%, hop testing >85%, and a Y-Balance test composite score >85% (Appendix 1).45 At her 16-week assessment, the subject’s Y-Balance test composite score was >95%, and her isokinetic strength testing demonstrated a quadriceps strength LSI deficit of 21%, a hamstrings strength LSI deficit of 2%, and a strength to body weight ratio of 72%.
Phase V – Agility/ Sport Specific Drills (4 – 6 months)
Phase V consisted of initiating sport specific agility drills while also continuing to normalize strength compared the contralateral limb. Running and plyometric activity had a larger emphasis on gymnastic-related activity to mimic routines performed on the vault, floor, and beam events. The subject also began performing agility drills starting in a singular plane progressing to multiple planes of movement. Early exercises consisted of Figure 8 cutting drills, lateral side shuffle, sprints forward and backpedaling, and ladder drills. Eventually as her confidence and the quality of movement improved, drills progressed to include multiple planes of movement including agility work such as the T drill or box drills. Plyometrics involved the subject landing on unstable surfaces such as an Airex foam pad or BOSU ball and from varying heights and depths including multiple planes of movement, progressing from bilateral to unilateral dismounts, to mimic gymnastic related activity. The subject continued to progress through the strength, agility, and plyometric exercises until she achieved the criteria to completely return to sport. As she neared return to sport she began training with her gymnastics coach to work on appropriate progressions to return to the vault, beam, bars, and floor. This was led by her coach, but communication continued between the coaching staff and the therapy team to determine what would be appropriate for the athlete. Criteria for physician release and complete return to sport consisted of a: strength LSI of > 90% compared to the contralateral limb, a normalized strength to body weight ratio of > 70%, as well as > 90% LSI on single leg hop, triple hop and crossover hop.31 In addition to performance testing, the subject had to score > 90 on the IKDC subjective questionnaire, > 60 on the ACL-RSI, and report zero yellow flags on OSPRO-YF.
OUTCOMES
Three different patient reported outcomes were utilized for this case study including the IKDC, ACL-RSI, and the OSPRO-YF (Table 2). The subject’s IKDC score improved from 60.92 (severely abnormal) to 96.6 (normal) by the time of discharge. This is much larger than the MCID of 11.5 points as well as places the subject in the highest classification of knee function. In terms of ACL-RSI, the subject had an improved score of 71 to 95. This achieves both the MCID of 15.1 and demonstrates psychological readiness to return to sport as a perfect score for the ACL-RSI is 100. Lastly the OSPRO-YF was used, however, the subject never reported yellow flags through the course of treatment demonstrating an overall positive treatment response and pain experience.
Performance testing was completed every eight weeks. The subject continued to demonstrate improvement in terms of performance testing throughout the course of treatment and achieved all RTS criteria at six months post-operatively. This includes isokinetic strength and hop testing LSIs of > 90% as well as a normalized strength to bodyweight ratio of > 70%.
DISCUSSION
The purpose of this case report was to provide a template of a rehabilitation and return to sport progression based on the available research for the treatment of an elite gymnast who had an ACL repair with IBLA. Female athletes, specifically those in fixed object high impact rotational landing sports, such as gymnastics are at an increased risk for an ACL injury.2 While many athletes choose to pursue the standard ACL reconstruction, an ACL repair with IBLA provides an alternative to an ACLR with associated advantages of maintaining proprioception, preserving the biology, minimizing surgical morbidity and allowing for faster recovery with adequate rehabilitation.8 In a study by Ortmaier et al., 91% of patients who underwent ACL repair with IBLA returned to sport.46 Furthermore, ACL repair with IBLA appears to show signs of increased stability and superior patient reported outcomes at levels greater than those accepted following ACLR.47,48 However, ACL repair is not suitable for all patients and careful selection is imperative to its success. Consideration for an ACL repair is typically reserved for Sherman type I ACL tears that occur in the proximal ACL as it requires sufficient tissue length and quality, typically within the first three weeks from injury.7,48 van der List et al. suggest that Type 1 ACL tears only account for 16% of all tears for those aged between 19-55 years old, with type III being the most common.49
ACL repair has gained momentum as an alternative to ACL reconstructions as of recent.7 Currently, ACL primary repair techniques have shown promising results in treatment of an ACL rupture; however, there is no common consensus on an appropriate rehabilitation protocol. The therapists who participated in this case report followed a short period of bracing until quadriceps control and full knee extension were restored. Early weight bearing was recommended to build tolerance to loads through the knee with the use of crutches. She began running around 13 weeks post-operatively and began sport specific training around 4.5 months postoperatively. She remained in the agility/ sport specific drills phase working with both the rehab team and coaching staff until she passed all the RTS criteria, similar to what occurs after an ACLR. Once she passed the RTS criteria, she was allowed to participate fully in gymnastics related activity and returned to competition at six months post-operatively.
There are several limitations for this case report, including the inclusion of only one subject, as is typical of a case-reports. In addition, due to time constraints, the follow up following rehabilitation was a short duration of only a few months and therefore long-term outcomes are unknown at this time. Furthermore, due to clinical constraints in space and technology, vertical jump LSI and gymnastics sports specific drills were not assessed prior to return to sport. The athlete was assessed via horizontal hop testing, however, there is an opportunity for the athlete to test well on these types of hops by utilizing compensation strategies, therefore limiting the reliability of the performance testing to determine true RTS readiness. Lastly, the findings from this report may not translate to other patient populations presenting with type 1 ACL tears as the case report design does not allow determination of cause and effect. Nonetheless, this case report is helpful in describing the clinical decision-making process and application of a rehabilitation progression in a female gymnast who underwent a primary ACL repair with internal brace ligament augmentation.
CONCLUSION
The results of this case report provide an example of an ACL repair protocol that was used in an elite female gymnast who achieved full return to sport at six months post-operatively. The intent this report was to provide evidence to help direct orthopedic surgeons and physical therapists regarding an appropriate rehabilitation guideline for their ACL repair patients. There is much variability related to surgical technique regarding bracing, ROM and weight bearing restrictions, and return to sport timeline which may affect implementation of these guidelines. Future research should focus on larger scale studies to explore the use of these suggested guidelines.
Subject Consent
Subjects were informed prior to treatment that data concerning the case would be submitted for publication.
Resident’s Case Report
Case report was completed during University of Florida Health Sports Residency approved by the American Board of Physical Therapy Specialties (ABPTS)
The authors report no conflicts of interest.