Introduction
Piriformis syndrome (PS) is recognized as an entrapment neuropathy where the sciatic nerve is compressed by the piriformis muscle (PM), often resulting in significant lumbar, gluteal, and thigh pain.1–3 This condition is characterized by symptoms such as lower back and buttock pain, muscular weakness, unilateral numbness, and hip and spine mobility challenges.2 The pain frequently radiates down the leg, sometimes extending into the medial foot, and is commonly accompanied by numbness in the posteriomedial lower limbs.1 Despite its resemblance to L5 or S1 radiculopathy in symptomatology, PS is typically attributed to either an anomalous PM or direct compression and irritation of the sciatic nerve. Its clinical presentation can be similar to those of lumbar disc herniation, stenosis, radiculopathy, and neurogenic pain, complicating the diagnostic process.4
Historically, the diagnosis of PS has relied primarily on physical examination and has been considered a diagnosis of exclusion due to the absence of direct, compelling imaging evidence.5 Traditional diagnostic approaches include clinical assessments, magnetic resonance imaging (MRI), and computed tomography (CT) scans.1,6–8 However, these methods are often hampered by high costs, limited availability, and occasionally inadequate resolution for distinguishing soft tissue abnormalities.8 Electrodiagnostic evaluations are frequently utilized to differentiate between PS and radiculopathy, though electromyography (EMG) has limitations such as low specificity and poor repeatability which challenge the precise localization and understanding of the lesion’s etiology.7
In recent developments, musculoskeletal ultrasound (MSK US) has emerged as a valuable diagnostic tool for PS, offering high-resolution imaging of muscles, tendons, joints, and nerves.9 The use of high-resolution ultrasonography has particularly enhanced the visualization of anatomical details, thereby expanding the utility of ultrasound in peripheral nerve imaging.9 Ultrasound provides a real-time, dynamic assessment and serves as a more accessible and cost-effective alternative to MRI, maintaining reliable accuracy.10 Early and accurate diagnosis through advanced imaging techniques is crucial for the effective management of PS and preventing diagnostic delays.
Epidemiology
The incidence and prevalence of PS remain uncertain, though estimates suggest that it accounts for 6% to 36% of cases involving low back pain and “sciatica.”11 Accurately determining the true prevalence is challenging due to the predominantly clinical basis of its diagnosis, which is typically one of exclusion.12 PS is most commonly observed during the fourth and fifth decades of life and affects individuals across various occupations and levels of physical activity. Research conducted by Jawish et al. indicated that among 3,550 individuals reporting sciatica symptoms, only 26 were diagnosed with PS. Furthermore, up to 50% of patients with PS report a history of trauma, often related to direct buttock contusion or torsional injuries affecting the hip or lower back.13
Anatomy
The PM, characterized by its flat, pyramid-like shape, generally functions as an external rotator, and provides weak abduction and flexion of the hip. The PM plays a critical role in maintaining postural stability during both standing (statically) and walking (dynamically) activities. Anatomically, it originates from the ventral surface of the sacrum, specifically lateral to the sacral foramina, extending from the margin of the greater sciatic foramen to the pelvic surface of the sacrotuberous ligament near the sacroiliac joint, spanning vertebral levels S2 to S4. The muscle attaches to the superior medial aspect of the greater trochanter and receives innervation from spinal nerves S1 and S2. In most individuals, the sciatic nerve exits the pelvis through the greater sciatic foramen, passing beneath the PM. However, variations occur wherein the sciatic nerve may either pierce or divide the PM. Such anatomical variations significantly increase the susceptibility to PS in affected individuals.
Technical Considerations
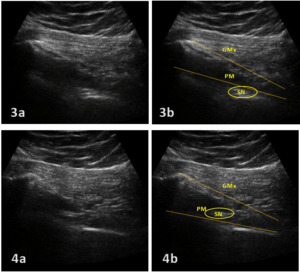
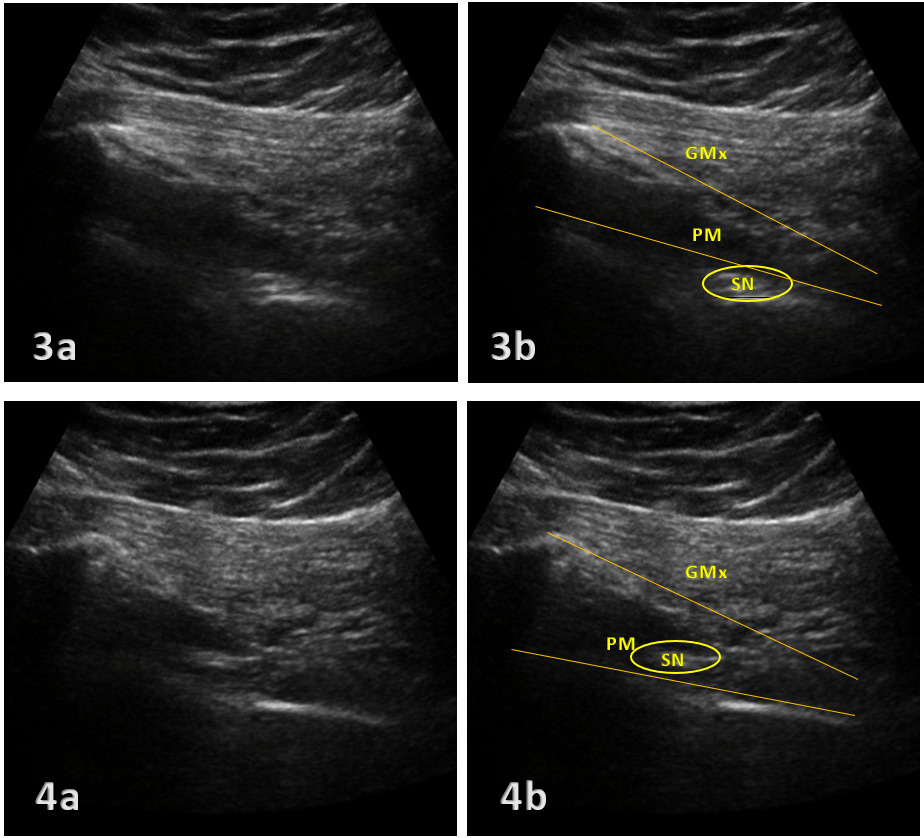
MSK US involves the use of a high-frequency linear transducer to obtain detailed images of the targeted area. When examining the PM using ultrasound, the patient should first assume the prone or lateral decubitus position to best visualize the PM and sciatic nerve.1 Placing a pillow or towels between the bed and the patient’s inguinal area can help increase the pelvic tilt. This allows better visualization of the PM via ultrasound. A curvilinear transducer is placed in a transverse orientation to first identify the sacral cornua and is then moved toward the greater trochanter until the lateral edge of the sacrum is observed. The transducer is moved further laterally until the greater trochanter and ilium are both observed (Fig. 1). The PM will appear as a hyperechoic band lying between the lateral edge of the sacrum and the greater trochanter and deep in the gluteus maximus muscle. The sciatic nerve appears as an oval shaped hypoechoic structure lying deep in the PM (Fig. 2).
Interpretation of Ultrasound Findings
Key ultrasound findings in PS include:
-
Hypertrophy of the PM
-
Echotexture abnormalities indicating muscle strain or tears
-
Increased vascularity suggesting inflammation
-
Compression or displacement of the sciatic nerve
These findings must be correlated with clinical symptoms and other diagnostic tests to confirm the diagnosis of PS.
Integration into Clinical Practice
For rehabilitation providers, integrating MSK US into clinical practice requires training in sonographic techniques and interpretation of images specific to musculoskeletal disorders. MSK US can guide interventions such as targeted physiotherapy, injections, and minimally invasive procedures by providing precise anatomical details.
Advantages of MSK Ultrasound
MSK US offers several advantages over other imaging modalities:
Non-invasive: Does not require ionizing radiation, making it safer for repeated use.
Cost-effective: Generally, less expensive than MRI and computed tomography, scans.
Dynamic imaging: Allows real-time visualization of the PM during motion, aiding in dynamic assessments.
Point-of-care: Can be used in various settings, including clinics and bedside evaluations, providing immediate feedback to guide treatment decisions.
Conclusion
Diagnostic MSK US is an effective and efficient tool in the evaluation of PS, offering detailed visualization of soft tissue structures. It enhances diagnostic accuracy and assists in the formulation of targeted treatment plans in rehabilitation settings. As technology advances and accessibility increases, MSK US is poised to become an integral part of the diagnostic process for musculoskeletal disorders such as PS.