INTRODUCTION
The utilization of anatomic total shoulder arthroplasty (TSA) in the United States has increased dramatically in recent years, with growth projected to outpace that of total hip and knee arthroplasty by 2025.1–3 As the rate of TSA procedures continues to rise, there has been considerable modification to surgical technique, implant design, and peri-operative care strategies.4 Specifically, there has been ongoing debate regarding the optimal rehabilitation protocol after TSA.1
Adherence to a postoperative rehabilitation protocol has long been regarded as essential in optimizing patient outcomes after TSA.5,6 Generally, rehabilitation is broken into three phases: passive range of motion and stretching, active range of motion with isometric exercises, and resistance exercises with progression of higher-level activities. Despite this, the current literature reports significant heterogeneity in rehabilitation activities and timelines.7 A recent review of 16 studies found significant variability between rehabilitation protocols after TSA, with strategies based on biomechanical principles rather than clinical milestones.1 Furthermore, 75% of the included studies were Level 5 evidence, highlighting the paucity of high-quality evidence available to guide rehabilitation practices. Limitations in the available literature have led providers and institutions to create their own rehabilitation protocols and guidelines, many of which are published online in order to increase clarity and coordination of care for patients and their therapists. However, the variability and abundance of these protocols may lead to additional confusion among patients and therapists.
The American Society of Shoulder and Elbow Therapists (ASSET) published an evidence-based consensus statement in 2020, outlining postoperative rehabilitation guidelines following anatomic TSA.8 These recommendations are based on a rigorous synthesis of practice patterns from ASSET members and American Shoulder and Elbow Surgeons (ASES) members. Despite the availability of this consensus statement, it is unclear to what extent existing rehabilitation protocols align with these recommendations.
The purpose of this study was to (1) quantify the variability in online anatomic TSA rehabilitation protocols, and (2) assess their congruence with the ASSET consensus guidelines. The authors hypothesized that there would be significant variability among published protocols, and that there would be significant divergence between these protocols and the 2020 ASSET consensus statement.
METHODS
Collection of Protocols
This study was a cross-sectional investigation of publicly available, online rehabilitation protocols following anatomic TSA. A web-based search was conducted on April 1st, 2022, of publicly available rehabilitation protocols for TSA from websites of all Accreditation Council for Graduate Medical Education (ACGME)–accredited academic orthopaedic institutions identified on the Electronic Residency Application Service (ERAS). Protocols were identified on the institutions’ websites. If they could not be located, a Google search using the search term “[Program/hospital affiliate/medical school affiliate] total shoulder arthroplasty rehabilitation protocol” was performed.
To supplement the original search, a second Google query was performed using the general terms “total shoulder arthroplasty rehabilitation protocol”, “total shoulder replacement rehabilitation protocol”, and “TSA rehabilitation protocol” to identify programs published online from private practices, individual practitioners, or non-academic institutions. TSA rehabilitation protocols appearing on the first 10 pages (corresponding to the first 100 hits on Google) of this query’s results were included. Articles were included from this secondary search if they commented on rehabilitation protocols following anatomy TSA. Duplicate protocols, those not in English, or those published outside the United States were excluded. Figure 1 demonstrates a flow diagram demonstrating protocol selection.
Data Extraction
Two separate reviewers independently conducted all searches and reviewed related protocols for inclusion. Disagreements among these reviewers were settled by a third independent reviewer. Each collected protocol was similarly independently reviewed by two authors to identify recommendations regarding immobilization, initiation, and progression of passive and active range of motion (ROM), initiation and progression of strengthening, and post-operative exercises and activities. The time of initiation was recorded as the time at which the activity or motion threshold was permitted by the protocol. Therefore, all time-related metrics reported as ranges were recorded as the early limit (i.e., 4-6 weeks was recorded as 4 weeks). Activities permitted within the first post-operative week were recorded as week 1.
Metrics for range of motion included time to initiation of passive ROM and active ROM, as well as the time after which various motion thresholds were permitted. Various components of ROM were collected as specified by each protocol, including forward flexion, abduction, external rotation, and internal rotation.
Strength metrics were recorded when explicitly permitted by each protocol. Collected metrics included time to initiation of strengthening, strengthening modalities (including isometric versus resistance exercises), specific exercises permitted by the protocol, and return to higher level activities such as sports.
Statistical Analysis
All statistical analyses were conducted in Microsoft Excel (version 16.51; Microsoft Corp., Redmond, WA, USA). Descriptive statistics including means, ranges, and standard deviations (SD) of the initiation times for passive and active ROM thresholds, immobilization, and exercises were performed. Percent recommending various active and resistance exercises and sports specific activities were summarized as percentages of all reporting protocols. Comparisons between ASSET start dates and mean start dates from included protocols were performed. One sample t-tests were conducted to compare mean (SD) start dates and ASSET recommendations with resulting p-values reported. Statistical significance was set at p<0.05.
RESULTS
Of the191 academic institutions queried, 46 (24.08%) had publicly available protocols online. The remaining 45 protocols were identified following the secondary search query which resulted in a total of 91 protocols in included in the analysis.
Post-Operative Immobilization
A total of 81 (89.01%) of included protocols commented on immobilization. Table 1 displays a breakdown of mode of immobilization, with most protocols utilizing a sling alone (n=53, 58.24%) or a sling with an immobilizer and/or abduction pillow (n=26; 28.57%). A total of 10 (10.99%) of protocols specified the use of a sling and abduction pillow in accordance with the ASSET recommendations. Of the 72 (79.12%) protocols addressing sling discontinuation, the average (± SD) reported time to discontinuation was 5.31 ± 1.18 weeks (ASSET recommendation: five weeks; p=0.03). Average time of complete immobilization was two weeks, however only one center recommended a period of complete immobilization.
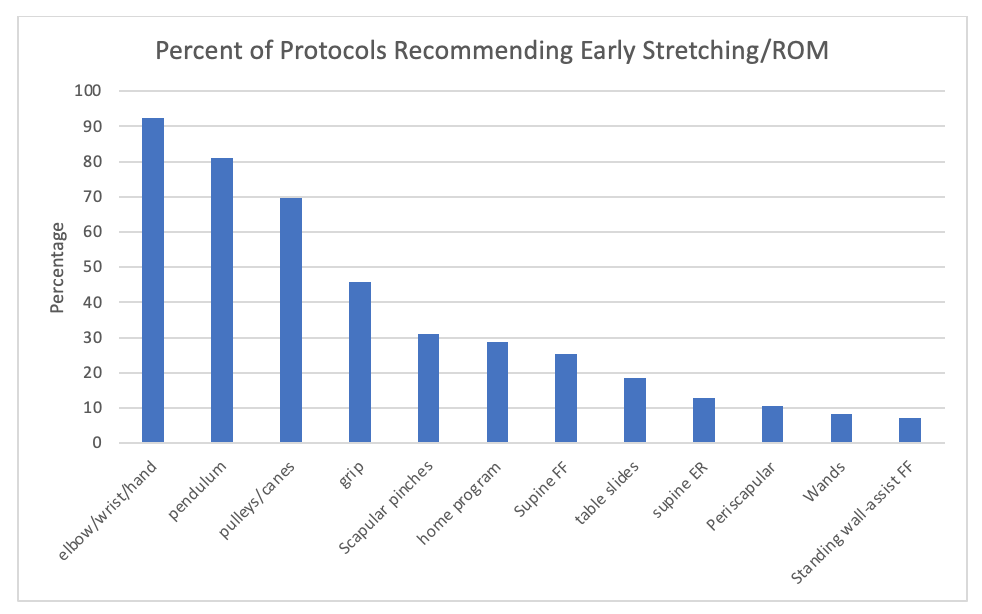
Initiation of Range of Motion
The most commonly reported early ROM exercises can be found depicted in Figure 2. “Early” was defined by initiation before six weeks. The majority of programs recommended early elbow/wrist/hand ROM (n=81, 89.01%) and pendulum exercises (n=71, 78.02%), as well as pulley/cane exercises (n=61, 67.03%). However, there was wide variability with respect to the recommended start dates for these exercises (Figure 3). The mean (±SD) start date was significantly later among included protocols for the initiation of pulleys/canes (3.05 ± 1.87 vs. one week; p<0.01) and table slides (2.31 ± 1.85 vs. one week; p=0.01) compared to ASSET recommendations.
Passive Range of Motion
There was wide variability regarding when programs recommended initiating various passive ROM (PROM) exercises (Figure 4). Included protocols recommended starting any passive ROM at an average of 1.19 weeks postoperatively (range: 1-6 weeks). Passive forward flexion (PFF) was initiated at an average of 1.20 weeks (range: 1-6 weeks) with passive external rotation initiated at an average of 1.21 weeks (range: 1-6 weeks). Passive abduction (PAb) was initiated at 1.35 weeks (range: 1-6 weeks) and passive internal rotation (PIR) was begun at an average of 1.65 weeks (range: 1-6 weeks). Unrestricted passive ROM was permitted at an average of 7.08 weeks postoperatively (range: 1-13 weeks) (Figure 4).
There were significant differences between the mean (±SD) start date among included protocols and ASSET recommendations for a majority of start dates for various PFF, PER, PIR, and PAb cut-offs (Figure 4). Notably, unrestricted PROM was significantly later for the ASSET recommendation (7.08 ± 2.64 vs. 12 weeks; p<0.01).
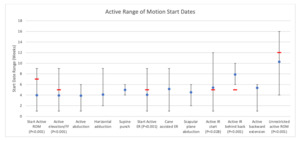
Active Range of Motion
Similarly, there was wide variability among start dates for active ROM (Figure 5). Active ROM was initiated at an average of 3.96 weeks (range: 1-9 weeks), active elevation/forward flexion at 3.94 weeks (range: 1-9 weeks) and active abduction at 3.87 weeks (range: 1-6 weeks). Active external rotation was initiated at an average of 4.07 weeks (range: 1-9 weeks), active internal rotation at 5.40 weeks (range: 1-12 weeks) and unrestricted active ROM allowed at an average of 10.29 weeks (range: 4-16 weeks) postoperatively.
Reported values for active ROM were significantly different than the ASSET recommendation for the initiation of active ROM (3.96 ± 1.95 vs. 7 weeks; p<0.001), active IR behind the back (7.90 ± 2.02 vs. 5 weeks; p=0.001), and unrestricted active ROM (10.29 ± 2.68 vs. 12 weeks; p<0.001).
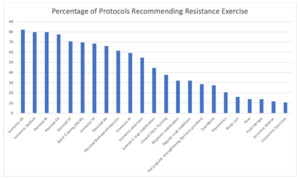
Isometric and Resistance Exercises
The most commonly recommended resistance exercises included isometric external rotation, isometric abduction, resisted forward flexion, resisted external rotation and resisted internal rotation (Figure 6). There was wide variability in the way these exercises were be performed (i.e., bands, dumbells). There was also considerable variability in the reported start dates for these exercises (Figure 7). The start dates for the initiation of resistance exercises recommended by the ASSET consensus protocol were significantly later than the mean (±SD) reported among included protocols. Specifically, there were differences seen for the start date of band training (6.97 ± 2.42 vs. 12 weeks; P<0.01), bicep curls (6.50 ± 2.38 vs. 12 weeks; P<0.01), upper extremity closed chain exercises (9.58 ± 3.48 vs. 12 weeks; P<0.01), and dumbbells for shoulder strengthening (8.79 ± 3.83 vs. 12 weeks; P<0.01).
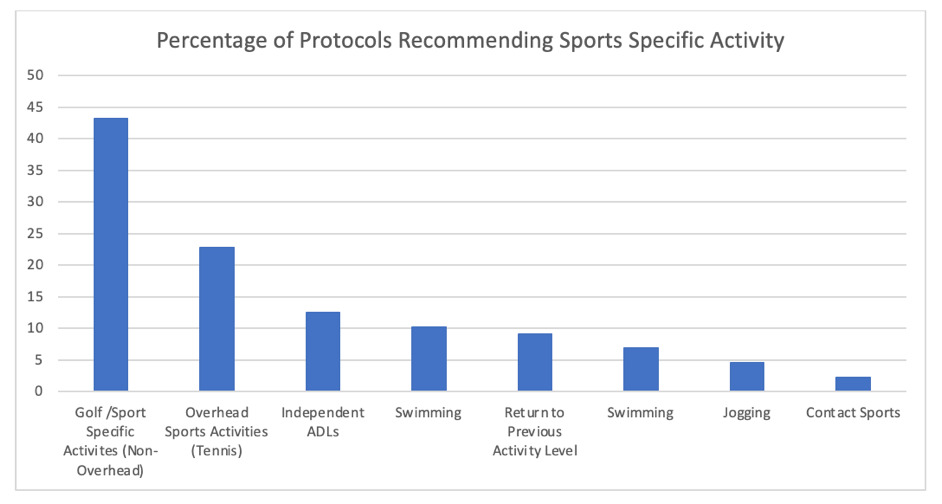
Return to Work/Sports and Activities of Daily Living
The included protocols demonstrated significant variation in the time to return to work (average 15.50, range: 6-24 weeks). Some sport specific activities were recommended (Figure 8). Return to golf and other sport specific activities without overhead components averaged 15.53 weeks (range: 10-24 weeks), with contact sports initiated at an average of 24.00 weeks postoperatively (Figure 9). Return to previous activity level occurred on average at 19.50 weeks (range: 12-23 weeks) and return to independent activities of daily living at 10.36 weeks (range 6-16 weeks). Protocols reported initiation dates for golf/sport specific activities (non-overhead) (15.53 ± 3.42 vs. 12 weeks; p<0.01), overhead sports activities (including tennis) (16.80 ± 4.02 vs. 12 weeks; p<0.01), swimming (16.67 ± 5.10 vs. 12 weeks; p=0.03), return to previous level of activity (19.5 ± 5.13 vs. 24 weeks; p=0.04), and independent activities of daily living (10.36 ± 3.11 vs. 5 weeks; p<0.01) that were significantly different than those recommended by the ASSET.
DISCUSSION
This investigation was focused on assessing the variability across online postoperative anatomic total shoulder arthroplasty rehabilitation protocols as well as their concordance with published ASSET guidelines. The authors hypothesized that there would be significant variability among published protocols, and that there would be significant divergence between these protocols and the 2020 ASSET consensus statement. Overall, considerable variability was found amongst current online protocols in terms of the time course for the initiation of specific planes of motion and strengthening exercises. Furthermore, substantial differences were found between these protocols and the ASSET guidelines, with surgeon protocols generally initiating activities at earlier timepoints than those recommended by ASSET.
Post-Operative Immobilization
Protection of the subscapularis tendon is paramount during the early phase of healing after anatomic TSA. In accordance with the ASSET guidelines, a large majority of online protocols included the use of a sling for immobilization in the post-operative period to facilitate this healing process. Interestingly, the average time for discontinuing the sling was longer among the included protocols than the ASSET guidelines, although this difference was small (5.31 weeks vs. 5 weeks) and perhaps not clinically significant. It is important to note that the consensus guideline supports discontinuation of a sling anywhere between the 4-to-6-week post-operative period given variability in subscapularis take-down methods and both pre- and intra-operative ROM assessments. This variability may help to explain why method and duration of immobilization differed from protocol to protocol, which has also been shown in prior studies.7
Range of Motion
The timetable for the initiation of early ROM remains a subject of ongoing debate. While the average time to initiation of various ROM exercises was relatively comparable to that recommended by the ASSET protocol, there were many protocols that did not allow these movements until a later post-operative time. For example, although the initiation of supine forward flexion was recommended to start at post-operative week 1 by the ASSET protocol, multiple protocols did not allow for this movement until six weeks post-operatively. Theoretically, prolonged immobilization has the potential to lead to stiffness. However, several authors have found no differences in patient reported outcomes or ROM in patients undergoing immediate or delayed therapy following shoulder arthroplasty at 12 months postoperatively.9,10 Although early mobilization is safe, it is not necessary to achieving a positive outcome in the long term, but may have an overall impact on earlier improved function and quality of life within the first 12 months.
Initiation of Passive and Active Range of Motion
Based on the evidence-based protocol proposed by Jackins11 the ASSET recommendations for post-operative mobility progress from initial gentle stretching in Phase 1 to active assisted movement and fully active ROM during Phase 2 of rehabilitation (weeks 7 through 12). Similar to the trends regarding post-operative immobilization/early ROM, there were substantial inconsistencies between included protocols in the initiation of various passive and active ROM thresholds. For example, wide variability was seen in the start dates reported for unrestricted passive (range: 1 week to 13 weeks) and active (range: 4 weeks to 16 weeks) ROM. Similarly, the average values for this start date among included protocols were significantly earlier than the ASSET recommendations (unrestricted passive and active: 12 weeks). Furthermore, there were discrepancies among protocols regarding the angles reported for passive and active ROM goals. Notably, although the ASSET guidelines comment on passive external rotation to 30-40 degrees and to 60 degrees, included protocols reported nine different external rotation cutoffs (0-10, 15, 10-20, 25, 20-30, 30-40, 40-45, 45-60, 60). It is unclear if the nine different cutoffs were clinically significant versus the concept of assure a slow and gradual progression.
Resistance Exercise/Strengthening
Early strengthening after anatomic TSA focuses on the periscapular musculature with gradual inclusion of rotator cuff exercises. As was demonstrated by Baumgarten et al., improvements in post-operative strength have been associated with greater improvements in ROM and patient reported outcomes.12 The inclusion of resistance training begins within Phase 3 of the ASSET rehabilitation consensus protocol, with strengthening primarily limited to below shoulder and frontal plane exercises. As was seen previously, wide variations were demonstrated for when each resistance exercise should be initiated, with a majority of included protocols reporting start dates within the first 2-3 months post-operatively. As Phase 3 does not begin until post-operative week 12, significantly earlier start dates were seen for band training, bicep curls, closed chain exercises, and dumbbells among these protocols. However, these variations may be partly attributed to the limited information among the current literature regarding the exact timing and type of strengthening post-operatively.13 Furthermore, exercises against resistance can be initiated for many different reasons, including for neuromuscular activation and/or motor control. When designing protocols for these patients, specific attention should be paid to goals of each specific resistance exercise.
Return to Work/Sports and Activities of Daily Living
While rates of return to sport have generally been high following anatomic TSA,14–18 there remains considerable variability in the current literature regarding the optimal time for this rehabilitation stage.13 Obviously, the details of the particular vocational or avocational activities influence timing of return. Although the ASSET recommends waiting until post-operative week 12 to initiate return to sports,19 full return is not indicated until post-operative month six to ensure adequate subscapularis healing. In a similar way, ASSET allows gradual return to work at 12 weeks. However, given that strengthening begins in earnest at 12 weeks, many careers would dictate a more conservative timeline for actual return to work. Overall, for a majority of post-operative sports specific activities, the ASSET guidelines were significantly more conservative than start dates among the included protocols. Notably, although the ASSET consensus allows for swimming, non-overhead, and overhead sports to begin at post-operative week 12, the average initiation date for these activities for most protocols was after post-operative week 15. Conversely, included protocols allowed return to previous level of activity significantly earlier (i.e. at 12 weeks post-operatively), despite concerns related to glenoid loosening and failure associated with higher activity levels within this post-operative period.20
Limitations
The investigation has several limitations to note. Despite the authors’ approach to identifying online protocols for analysis, there was a relative paucity of online protocols and as such, assuming that institutions have protocols that are not on the world wide web, the analyzed sample may not be representative of all ACGME institutions. Additionally, given the fairly recent publication of ASSET in 2020, there is a chance that current online protocols may be outdated and thus may not reflect the recent consensus guidelines. It is also possible that these websites have not been recently updated to reflect the current protocols of these institutions. Similar to a previously published comparison comparing online rehabilitation protocols following rotator cuff repair to ASSET guidelines, the nature of such an evaluation has limitations that warrant mention.21,22 The content of the ASSET statement was primarily developed by therapists with additional input from ASES surgeons.8 Although this procedure was inherent to the methodology for the development of these guidelines, there is the possibility for differing perspectives, opinions and approaches for surgeons and postoperative rehabilitation. This is also potentially true in the context of a large variety of prosthetic options presently available that may offer improved fixation strategies, mechanisms for bony in-growth of the implant, and options for subscapularis repair. In addition to wide ranging surgical variables, there is also a wide range of patient variables in the TSA cohort. Each patient has unique combination of characteristics (age, activity level, comorbidities) which dictate the pace of their rehabilitation. Although the ASSET guidelines provide a consensus statement driven by current literature, they cannot be interpreted as the gold standard for postoperative rehabilitation for every patient. Perhaps this is one of the factors that led to such a wide variation between protocols analyzed in this study. Regardless, the optimal protocol should have options for individualization based on each patient and their specific surgeon. To better elucidate specific time points for the initiation of ROM exercises and strengthening, high-quality literature is needed to assess muscle activation patterns, muscle force patterns and subsequent outcomes that might dictate when certain rehabilitation elements can be safely started.
CONCLUSION
Considerable variability was found among the included online post-operative protocols for anatomic TSA in terms of the time course for initiation of specific planes of motion and strengthening exercises. Notably, substantial deviation was found between these protocols and the ASSET guidelines. These findings highlight the lack of standardization in rehabilitation protocol following anatomic TSA. Subsequently, the current findings highlight the importance of a more standardized and specific rehabilitation protocol following anatomic TSA. Further investigation is warranted to assess the true impact of these variations and to identify optimal recommendations for the initiation of elements of postoperative rehabilitation.
Conflicts of interest
There are no financial biases or conflicts of interest for any author related to this study. The study was exempt from International Review Board approval as no identifiable patient information was used.


.jpg)
._passive_a._forward_flexion_(pff)__b._abduction_(pab)__c._external_rotation_(per)__an.jpg)
_for_resistance_exercises.png)

_for_various_postoperative.png)

.jpg)
._passive_a._forward_flexion_(pff)__b._abduction_(pab)__c._external_rotation_(per)__an.jpg)


_for_resistance_exercises.png)
_for_various_postoperative.png)