INTRODUCTION
Barbell exercises are gaining in popularity in resistance training for health, rehabilitation and performance and are also performed in competition (for example in powerlifting, Olympic weightlifting, and CrossFit).1–4 Notably, resistance training and use of free-weight barbell exercises has been one of the top fitness international trends the last few years.5 A common exercise during barbell training is the barbell back squat (BBS), which is performed by squatting down with a barbell placed on the upper back and shoulders. The BBS can be performed with various lifting techniques depending on purpose; mobility, strengths and weaknesses, anthropometry etc., while in the sport of powerlifting, the execution has been standardized to enable strict judging during competition. For example, sufficient depth (i.e. range of motion [ROM]) of the squat is considered to be reached when the upper side of the thigh is clearly below the top of the knee joint.4
In powerlifting, injuries that cause lifters to abstain from training and competition are rare.6 However, it is common for powerlifters to experience pain in the low back, hips, and/or knees that interferes with their training, with the onset of these pain problems frequently associated with BBS training.7 Although lifting technique in barbell training generally is considered important for performance and preventing injury,8 there is a lack of robust evidence and an ongoing discussion regarding the extent to which specific aspects of lifting technique affects performance and injury risk.9
Notably, the position and movement of the low back and pelvic area (i.e., lumbopelvic region) while lifting has been specifically discussed and investigated in research. For example, a study by Sjöberg et al.10 aimed to develop evidence-based guidelines regarding aspects of lifting technique which could influence the risk of injury during the BBS and the barbell deadlift. Powerlifting experts agreed that deviation from a neutral spine position into lumbar flexion during BBS and deadlift training could increase the risk of injury.10 It should be noted that other studies have shown that the lumbopelvic region naturally flexes significantly while performing squats,11,12 i.e., it does not remain in the proposed neutral position during the exercise, and when powerlifters perform the deadlift, the lumbar spine typically does not move into its outer ranges of motion.13 Additionally, a review by Saraceni et al.14 investigated if lumbar flexion during occupational lifting influenced severity or incidence of low back pain but found no such relationship. To date, the evidence regarding the importance of spinal alignment of the lumbopelvic region and risk of injury in the BBS is inconclusive. Nevertheless, there are indeed occasions when it is appropriate to both analyze contributing factors to, and limit, lumbopelvic flexion, e.g. during rehabilitation when gradually progressing an individual into activities requiring lumbopelvic flexion.
Although several studies have investigated and quantified movements of the lumbopelvic region during the BBS,11,12,15 there is a lack of studies describing which factors could influence the magnitude of movements. According to motor control theories16 there are many factors that could contribute to an individual’s ability to perform a BBS, including anthropometric factors, ROM of the lower extremity, and movement control of the lumbopelvic region. During the BBS, the hip, knee, and ankle joints move from an extended starting position into flexion and then return. The degrees of flexion needed in the hip joint to perform a deep squat varies between individuals primarily depending on anthropometric factors and available ROM in the involved joints, for example squats without a barbell requires a mean hip flexion of 95°±27°.17 Generally, if the ROM in the ankle joint is greater, less flexion will be needed in the hip joint, since the trunk can be maintained in a more vertical position.18,19 For example, by restricting movement of the ankle and restricting anterior knee displacement in the BBS an increased trunk lean18 and movements of the thoracic and lumbar spine19 have been observed. Variations in BBS lifting technique could also have an influence on the amount of lumbopelvic flexion, and a previous study by McKean et al.11 demonstrated that stance width had a small effect on lumbopelvic flexion. However, there are no previous studies that have investigated if the ROM of the hip and ankle joints can affect lumbopelvic flexion during a BBS.
Anthropometric ratios or bodily proportions, have also been proposed to affect the general performance and lifting technique during barbell exercises,20 and have been measured in relation to the BBS in previous studies.21 For example, it is commonly suggested that an individual with a long trunk and short femurs will, generally, perform the BBS with a more vertical trunk than if the ratios were the opposite. However, no studies have explored if anthropometric factors are associated with lumbopelvic flexion during a BBS. Another factor that could influence performance and lifting technique during a BBS is the movement control/coordination of the lumbopelvic region.22 Evaluating movement control of the lumbopelvic region with tests that challenge the ability to keep the lumbopelvic region in neutral position while moving other joints during low load tasks is common in clinical practice when assessing patients with low back pain.22,23 During the BBS, the hips and lumbopelvic region are placed under high stress and movement control of the area is of importance, however, there are no previous studies that examine if low load movement control tests are associated with movement control during high loads, in for example the BBS.
As mentioned previously, it is unclear whether deviation from a neutral position of the lumbopelvic region could be a risk factor for injuries when performing the BBS. It is also unclear how this deviation could affect performance during the exercise. However, considering the popularity of the BBS both in sports, recreation, and rehabilitation, it is essential that the strength and conditioning professionals and/or physical therapists can make informed assessments of a client/patient when implementing the BBS in their practice. It is therefore meaningful to investigate which factors might affect the movement pattern of the lumbopelvic region during the BBS. Therefore, the purpose of this study was to investigate the association among anthropometric measurements, ROM of hips and ankles, lumbopelvic movement control tests and flexion of the lumbopelvic region during execution of the BBS. The authors hypothesized that longer femur length, lower ROM in the hips and ankles, and poorer performance in lumbopelvic movement control tests would be associated with higher lumbopelvic flexion during the BBS.
METHODS
This cross-sectional study included experienced powerlifters and Olympic weightlifters. The data collection included measurements of the dependent variable: mean ROM of the lumbopelvic region from the start position to the bottom of the BBS (i.e., lumbopelvic flexion), measured with wearable movement sensors at the second lumbar vertebrae (L2) and sacrum (S2), during three repetitions of BBSs at 70% of 1RM (repetition maximum). The independent variables included physical examination of anthropometrical measures (length of trunk and extremities, measured with measuring tape), ROM in the hip and ankle joints (measured with a manual goniometer), and lumbopelvic movement control tests. Linear regression was used to establish predictive models to analyze which factors could explain flexion of the lumbopelvic region.
Participants
The participants were recruited from powerlifting and weightlifting clubs in Umeå, Sweden. Initially, 19 participants were- recruited, but one participant had to be excluded due to data-error. Therefore, a total of 18 participants, eleven male, seven female; twelve powerlifters and six Olympic weightlifters, were included. To be included, participants had to have at least two years of resistance training experience and either training to compete or competing in power- or Olympic weightlifting. Further, they had to be injury free, i.e., without an injury preventing them from training and performing the BBS or any medical conditions preventing them from performing the BBS. They also had to be at least 150 cm tall, to avoid the movement sensors touching each other during movements.
On inclusion, all participants completed a questionnaire detailing their background information, performance in the BBS, training experience, and training regime. All participants also provided written consent and were informed that they could end their participation at any time without further explanation. Risk of harm or injury was considered not to exceed the risk of their standard training routine since the load used was set at 70% of the participants estimated 1RM. The study protocol was approved from the Regional Ethical Review Board (2014-285-31M).
Procedures
The data acquisition process comprised two distinct phases. The initial phase (part one) involved the collection of lumbopelvic movements during the BBS, while the subsequent phase (part two) encompassed the gathering of anthropometric measures, ROM of hips and ankle joints, and lumbopelvic movement control test data.
Part one: Following a self-administered warm-up, participants executed three repetitions of the BBS, conforming to competition standards established by the International Powerlifting Federation, i.e. hip crease below the top of the knee joint,4 with a load of 70% of 1RM (based on self-reported estimation from the participants) with their preferred lifting technique, including bar placement, stance width etc. The load was chosen to represent a weight that lifters normally use during training, while also lowering the risk of any adverse events occurring, as could happen with loads closer to the lifters’ 1RM. During the lifts their lumbopelvic movements were recorded with an inertial based movement analysis system (MoLabTM AnyMo AB, Sweden). Two wireless movement sensors were attached on the participants directly on to the skin over the spinous processes of L2 and S2. The sensors were attached with double-sided adhesive tape and secured with elastic adhesive bandage wrapped around the trunk. A third sensor was also attached over the spinous process of T11 but data from that sensor was not included in the present study. A fourth sensor was attached to the lateral aspect of the distal thigh to measure depth/ROM and stance width of the BSS. Depth/ROM was assessed by the difference in the sagittal plane angle between habitual standing and the bottom position of the BBS. Stance width was measured by the difference in the frontal plane angle between habitual standing without the barbell and the squat stance. Positive values indicated greater depth for ROM, while negative values indicated a wider stance compared to habitual standing. The participants were allowed to use wrist wraps and shoes of their choice, but no other equipment that could improve stability (e.g., lifting belt) was allowed.
An in-depth description of the movement analysis system and technical specifications in regard to measurement of lumbopelvic movements during the BBS have been provided earlier.12 The system is inertial based and has been used to analyze the BBS in previous studies.12,24 The sensors (60*45*10 mm) incorporate a three-dimensional gyroscope, accelerometer, and magnetometer. These sensors are interconnected to a computer using a Wi-Fi connection and controlled with the AnyMo software. The movement analysis system has been validated25 and tested for reliability in both inter- and intrarater contexts.26
Part two: Data collection consisted of anthropometry, ROM of the hips and ankle joints, and lumbopelvic movement control tests with the instruments and methods described below. Measurements were conducted by two physical therapists possessing considerable expertise in palpation, assessment of passive ROM, and movement control assessments and training. Both therapists held a master’s degree in orthopedic manual therapy (i.e., a post-graduation specialization in neuro-musculoskeletal disorders for physical therapists) and each therapist had over five years of clinical experience specifically within the power- and weightlifting population. The physical therapists assisted each other when taking the ROM measurements, while all reading of measurements was done by the same therapist for all participants.
Anthropometric measurements were collected in a standardized manner to assess both trunk dimensions and the length of the lower extremities.27 Tibial length was measured between the superior point of the medial condyle and the most distal point of the medial malleolus. Femur length was measured from the superior point of the lateral condyle and the most superior point of trochanter major. Length of upper body was measured in sitting position from the surface of the chair to acromion’s lateral edge. Measures were double checked and on discrepancies, and an average was noted.
Range of motion (ROM) was measured with a manual goniometer (in degrees) and with a tape measure (cm) in the case of the weight bearing lunge test. A single measurement of ROM was taken for each joint and movement direction. The two physical therapists assisted each other in all measurements so that one of them performed the passive movement and stabilized the participants body, while the other positioned the goniometer and took the measurement. Overall, manual goniometry has demonstrated a good reliability for ROM measures in the hip and ankle joints.28–30
Hip flexion with straight knee: Measured in supine position with hip in zero position (no rotation/abduction/adduction) and extended knee until flexion in the lumbopelvic region could be palpated.31
Hip flexion with bent knee: Measured in supine position with hip in neutral (no rotation/abduction/adduction) and flexed knee joint until flexion in the lumbopelvic region could be palpated.31
Hip abduction with straight knee: Measured in supine position, wherein the test leader simultaneously abducted the participant’s leg while at the same time stabilizing the anterior superior iliac spine (ASIS) on the contralateral side.
Internal and external rotation of the hip: Measured in a sitting position with the feet hanging above the floor and hips flexed at approximately 90°.32
Dorsiflexion of the ankle joints: Measured one leg at the time in a weight-bearing lunge test position33 during which two measures were taken: 1. the ankle dorsiflexion angle (degrees), and 2. the distance (cm) the knee moved anteriorly relative to the distal part of the great toe. Standing with one foot in front of the other, participants pushed their anterior knee forward over the foot as far as possible without lifting the heel. The physical therapist then measured the dorsiflexion angle with a goniometer, using the lateral foot (fifth metatarsal) and fibula as reference points, and used a tape measure to record the distance the knee moved past the great toe.30,33
Movement control was assessed with four reliable clinical tests used as a test battery.22 The aim of the tests was to examine if the participant could maintain a neutral lumbopelvic position while moving the lower limbs. The selection of tests considered the relevance of joints and movement directions in the context of the BBS. Each test passed was awarded one point if the participant could perform the test as described below, which gave a maximum score of four points in the test battery. All tests were performed for three repetitions and to be passed as a correct test the participant needed to perform one repetition correctly.
Standing “trunk lean test”:22 The participants started the test in standing and were instructed to bend forward by flexing the hips to 50° while keeping the lumbopelvic region in neutral position, and then return from this position without moving the lumbopelvic region into flexion or extension. The test has shown a substantial inter-rater reliability between experienced raters, Kappa coefficient = 0.71 (CI 95% 0.5-0.92), and substantial intra-rater reliability, Kappa coefficient = 0.75 (CI 95% 0.55-0.95) to 1.0.22
Forward rocking test22: The participants started the test in four-point kneeling with 90° flexion of the hips and knees and the lumbar spine and pelvis in neutral position. The participants were instructed to rock forward until the hips were extended to 0°, while keeping the lumbopelvic region in neutral position. The test has shown a substantial inter-rater reliability between experienced raters, Kappa coefficient = 0.66 (CI 95% 0.39-0.93) and low to substantial intra-rater reliability, Kappa coefficient = 0.22 (CI 95% 0.00-0.64) to 0.8 (CI 95% 0.56-1.00).22
Backward push test22: The participants started the test in four-point kneeling with 90° flexion of the hips and knees and the lumbar spine and pelvis in neutral position. The participants were instructed to push backwards to flex the hips to 120° while keeping the lumbopelvic region in neutral position. The test has shown a substantial inter-rater reliability between experienced raters, Kappa coefficient = 0.68 (CI 95% 0.45-0.91) and substantial intra-rater reliability, Kappa coefficient = 0.70 (CI 95% 0.48-0.92) to 0.73 (CI 95% 0.44-1.00).22
Sitting double knee extension22: The participants started the test in sitting with the pelvis and lumbar spine in neutral position with the feet unsupported in the air. The participants were instructed to extend the knees to approximately 10-15° from full extension while keeping the lumbopelvic region in neutral position. The test has shown a substantial inter-rater reliability between experienced raters, Kappa coefficient = 0.80 (CI 95% 0.61-0.99) and low to substantial intra-rater reliability, Kappa coefficient = 0.90 (CI 95% 0.77-1.00) to 1.0.22
Statistical analysis
Means and standard deviation were used for descriptive statistics. To compare differences between male and female participants, an independent samples T-test was used for normally distributed variables and a Mann-Whitney U-test for non-normally distributed variables. To evaluate which factors that could explain lumbopelvic flexion during the BBSs, separate univariate linear regression was performed for each of the independent variables, i.e., anthropometry, ROM of the hips and ankle joints, and lumbopelvic movement control tests, with the mean value for ROM of the lumbopelvic region during the three repetitions of the BBS as dependent variable. Second, multiple linear regression analyses were performed with the significant (p<0.05) variables from the univariate analysis, where the independent variable with the highest adjusted R2 were first entered into the multiple regression model. Afterwards, the remaining significant independent variables from the univariate analysis were added one at a time, starting with the highest adjusted R2 and kept in the model if significant and if the explained variance (adjusted R2) was increased. In the multivariate analysis the p-value was adjusted using the Bonferroni’s method, with the p-value for the multivariate analysis model adjusted to p=0.0167 (p=0.05/3). Since there is an inherent risk of multicollinearity between independent variables when measuring both left and right sides of the body, for example the ROM of the hips and ankles, these variables were summed to a single variable and analyzed as a single variable if both left and right side was significant in the univariate linear regression. To assess possible correlation of the participants depth/ROM during the BBS and lumbopelvic flexion, a bivariate correlation analysis was performed (Pearson correlation).
RESULTS
Background characteristics of participants are presented in Table 1. There was a statistically significant difference between male and female participants in height, weight and 1RM squat (p<0.05). Eight participants reported that they had a current pain condition in the low back area or lower extremity (low back and hip n=1, hip n=4, knee n=3), but none of the participants reported that it hindered their ability to perform the BBS.
Descriptive statistics of the independent variables used for the linear regression analysis, i.e., ROM in hips and ankles, anthropometric measures and lumbopelvic movement control tests are shown in Table 2 and Table 3. There were statistically significant differences between male and female participants in the femur/tibia ratio (p=0.01), Movement control test battery (p=0.02), hip flexion with bent knee, left side (p=0.02), ankle dorsiflexion, left side (cm) (p=0.02) and ankle dorsiflexion right+left (cm) (p=0.04).
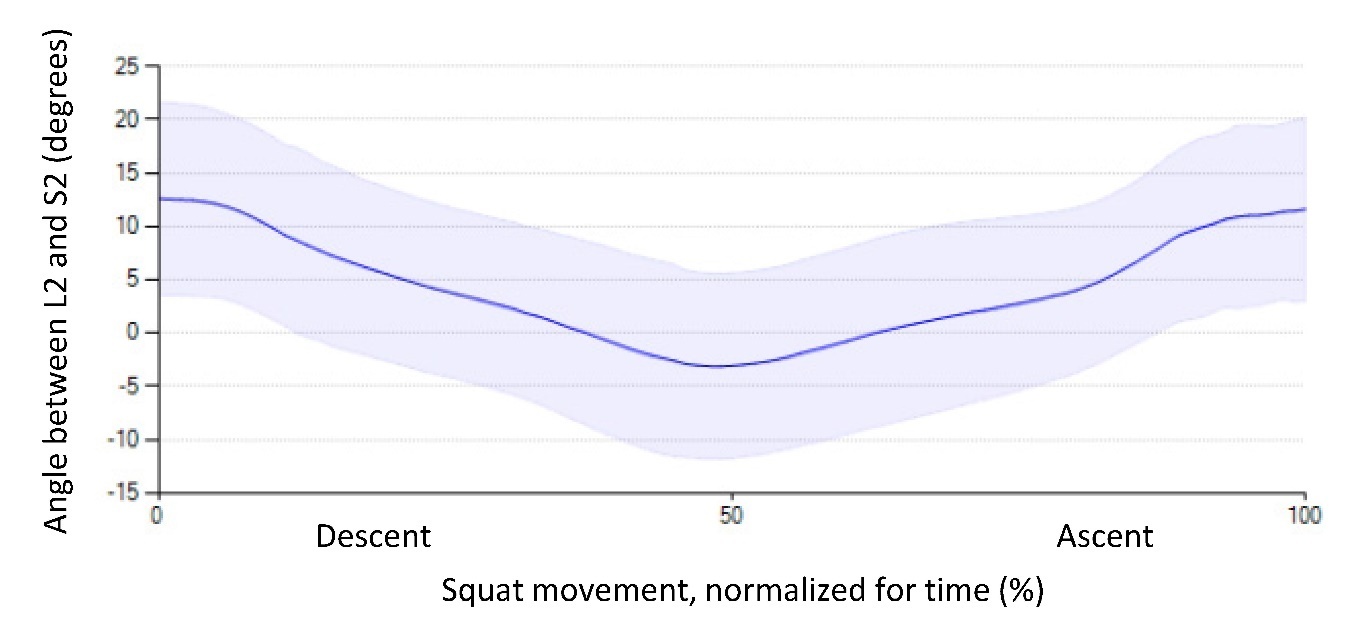
During the BBS, all participants flexed their lumbopelvic region, mean 18.4° (SD 4.7°, minimum 9.3°, maximum 27.9°). The angular displacement between L2 and S2 during the BBS movement is presented in Figure 1. The mean depth/ROM of the BBS movement from habitual standing to bottom position, was 100.6° (SD 13.4°, minimum 67.8°, maximum 120.6°). There was no statistically significant correlation between the depth/ROM in the squat and lumbopelvic flexion (r= 0.29, p=0.24). The mean stance width was -2.3° (SD 3.2°, minimum -9.2°, maximum 3.0°).
The results of the univariate linear regression analyses showed that neither anthropometric factors nor the Movement control test battery had any statistically significant relationship with movement of the lumbopelvic region during a BBS. Neither did the variables regarding ROM of the hips. The results of the univariate linear regression analyses for all the non-significant independent variables are presented in Table 4.
Four variables, all measures of ROM in ankle dorsiflexion, from the univariate linear regression were statistically significant. Ankle dorsiflexion (°) on the left side (unstandardized B-value (95% CI), 0.29 (0.03, 0.55), adjusted R2 = 0.21, p=0.03), and, ankle dorsiflexion (cm) on the right (unstandardized B-value (95% CI), 0.66 (0.06, 1.3), adjusted R2 = 0.21, p=0.03), and left side (unstandardized B-value (95% CI), 0.76 (0.16, 1.4), adjusted R2 = 0.27, p=0.02) and the combined ankle dorsiflexion (cm) for both right and left sides (unstandardized B-value (95% CI), 0.37 (0.07, 0.68), adjusted R2 = 0.25, p=0.02).
No multiple linear regression analyses were performed since the significant variables from the univariate linear regression, noted above, were highly correlated (Pearson correlation 0.82-0.98, p<0.001).
DISCUSSION
This study aimed to evaluate the association between anthropometry, ROM in hips and ankles, lumbopelvic movement control tests and lumbopelvic flexion during the BBS. The results indicate that higher ROM in dorsiflexion of the ankle joints was associated with higher lumbopelvic flexion during the BBS. Surprisingly, no other associations were found.
The authors hypothesized that the relationship would be reversed, as traditionally suggested within the field of biomechanics/kinesiology, i.e., the principle that movement will take the path of least resistance.34 This principle is often exemplified with a scenario of limited ROM in an extremity joint leading to increased movement occurring in the lumbopelvic region,34,35 e.g. limited ankle dorsiflexion or limited hip flexion leading to increased lumbopelvic flexion during different activities such as the BBS. In contrast to this principle, higher ankle dorsiflexion and hip flexion ROM has previously shown association to greater squat depth36 which in turn has shown association to increased lumbopelvic flexion occurring with increasing depth of the squat.11 However, this was also contradicted by the findings in the present study, where there was no correlation between depth/ROM of the BBS and lumbopelvic flexion, therefore indicating that it is likely that other biomechanical and motor control factors better can explain the results. For instance, lifters with overall greater ROM also have more movement options in the BBS, i.e., are more likely to be able to perform the BBS with more/less anterior knee displacement or trunk lean, i.e., greater demands of coordinating and timing movements of each joint, including the lumbopelvic region. In comparison to a lifter with, for example, very limited ankle dorsiflexion or hip flexion ROM, i.e., fewer movement options, they are more likely to be restricted to perform the BBS with a specific movement strategy and less likely to utilize ROM in the lumbopelvic region. There is also a possibility that a greater anterior knee displacement leads to the lifter also shifting the center of mass forward. To maintain balance, the forward shift of the torso and the knees could lead to an increased lumbopelvic flexion. Interestingly, a study by Demers et al.21 found a significant correlation between ankle dorsiflexion, knee flexion angles, and femur/tibia length ratio, but surprisingly not with hip flexion angles during unloaded squats. Thus, demonstrating a compensation for their relatively longer femur with increased anterior knee translation, rather than increased trunk lean. Likewise, participants in the present study might have used similar movement strategies.
Another variable possibly affecting the results is the spinal curvature in the starting position of the BBS. In the present study, the starting position was self-selected (participants used their normal squatting technique) and lumbopelvic flexion was measured from the start to the bottom position of the BBS. Participants that may have initiated the BBS with a greater lumbopelvic extension will also start the movement in greater hip flexion, possibly resulting in a larger lumbopelvic ROM during the BBS. Future studies should examine how the lumbopelvic position in the starting position of the BBS could affect lumbopelvic kinematics since technical instructions and cues given to the lifter could impact this position.
Regarding anthropometric factors, the present study found no relationship between anthropometric factors and lumbopelvic flexion. Although anthropometric factors determine, to a certain extent, how much the trunk is bent forward in the sagittal plane and thus could contribute to the requirements for mobility in the foot and hip joint and subsequently lumbopelvic region, the results of the present study did not show this relation. One reason for this may be because the anthropometric measurements did not deviate substantially within the group, thus a larger group of participants with a greater variation would be required to study these factors more accurately. However, the results are in line with a study by Fuglsang et al.,37 which failed to show a relation between trunk lean in the BBS and segment length ratios.
Regarding passive ROM in hips and ankle joints, all variables except ankle dorsiflexion ROM were non-significant. The authors had hypothesized that hip flexion ROM would influence the lumbopelvic flexion during the BBS, as a limited hip flexion would require the lifter to utilize the mobility of close by joints according to the principle of least resistance.34 As stated previously, performing a BBS requires a mean hip flexion of 95°±27°.17 In the present study the participants had a mean hip flexion of 99.8°±11.3°, suggesting adequate hip flexion ROM without limitations that would hinder their ability to perform the exercise. It is also possible that lifters adapt to a depth that is suitable to their own personal movement capabilities, including joint ROM, while still abiding to the requirements of the sport, i.e. only squatting as deep as is needed and to a depth that enables the best performance and comfort. This could also be a possible explanation as to why depth and lumbopelvic flexion was not correlated.
The lumbopelvic movement control tests did not show any association with lumbopelvic flexion during the BBS at 70% of 1RM. This lack of association is also an important finding for coaches and therapists examining individuals with pain during BBS. Petty38 underscores the importance of performing clinical tests, relevant for the situation were pain/discomfort is triggered. If pain/discomfort is triggered in high load situations like the BBS, then tests and movement assessments need to be performed in this situation. The result indicates that examining the ability to keep the lumbopelvic region in neutral position during low load tests may not be relevant if the pain/discomfort only is triggered in high load situations. These indications are also confirmed by a recent study of movement control tests in powerlifters with/without low back pain which showed no difference in performance of these types of tests.39 Also, a common perception in rehabilitation and fitness is that correct technique and spinal alignment with bodyweight or light loads are prerequisites for progressing to heavier loads. However, this study suggests that lumbopelvic movement control with low loads may not predict lumbopelvic kinematics with heavier loads.
Finally, some variables related to both anthropometry, hip and ankle ROM and the Movement control test battery differed significantly between male and female participants. Differences in anthropometry between male and females have been documented in studies of bony anatomy and limb length.40,41 The difference for the Movement control tests have not been described earlier and might simply be explained by chance. However, due to the small sample size it was deemed inappropriate to make further sub-analysis or adding sex as a control variable in the linear regression analysis. Future studies should increase sample size or plan for separate analysis between male and female lifters to consider potentially confounding effects of sex in relation to kinematics of the lumbopelvic region during the BBS and other barbell exercises.
Methodological considerations
There are some methodological considerations related to the data collection procedure. As in all studies using sensor technology, e.g., reflective markers for motion capture or as in the present study, inertial movement units, the sensors are attached to the skin and although enhanced with tape it is possible that, even though it may not be visible to the eye, the sensors might have moved and therefore the measures might have deviated some due to movements of the skin. However, this is true for all kinematic studies and for all participants.
Moreover, the measures of anthropometry, ROM, and lumbopelvic movement control were performed by one physical therapist, with manual assistance from a second physical therapist when taking the ROM measures using a goniometer. While no reliability calculations for these measures were included in the analysis, the measurements are widely used and accepted in practice. Previous studies have also shown acceptable reliability for goniometer measures of passive ROM and movement control tests when performed by physical therapists with similar or even less experience than those in the present study.22,28–30 However, tape measurements of limb lengths are generally less valid and reliable compared to gold standard instruments.42 It should be noted that the absence of reliability testing does not necessarily invalidate the study’s results, however, the results should be interpreted with caution. Further studies including reliability analysis needs to be performed to help interpretation of the results.
Further, as mentioned, the BBS depth/ROM was only standardized to a minimal acceptable depth/ROM. Further standardization including the maximum allowed squat depth could have helped the analysis. However, as mentioned earlier, there was no correlation between depth/ROM in the BBS and lumbopelvic flexion. Also, a methodological problem with standardizing depth would be that lifters who are used to descending deeper than the specified minimum depth would have to change their habitual movement strategy, thereby probably affecting the lumbopelvic alignment. Notably, previous kinematic studies of the BBS have used the same instructions regarding depth/ROM in the BBS.11
A second kinematic variable which should be discussed is the stance width used. The width was not standardized, but also did not vary to any significance among the participants. A study by McKean et al.11 indicated that stance width, when standardized as narrow or wide, where narrow stance was equal to pelvic width and a wide stance was defined as twice the pelvic width, could affect lumbopelvic flexion. Namely, a narrow stance resulted in a statistically significant but very slight increase in lumbopelvic flexion (~2 degrees difference in the maximal lumbar flexion ROM during the BBS).11 Therefore, standardizing or controlling for the stance width was not prioritized in the present study.
The current investigation involved the examination of eighteen variables in relation to a single dependent variable, with 18 participants included in the study. Each univariate linear regression satisfied the criterion of 15 participants per dependent variable,43 however, the elevated number of variables raises the potential for both Type 1 and Type 2 errors. The present study, while possibly underpowered, is valuable as it is the first of its kind to investigate these factors influencing lumbopelvic flexion during the BBS, thereby guiding future research methodologies in this area. Given the complexity of the BBS exercise and its multifactorial nature, it must be acknowledge that individual movement patterns are intricate and there are many ways to perform a BBS. To gain a more comprehensive understanding of why flexion of the lumbopelvic region occurs during BBSs, further research with a larger sample is needed.
Regarding the participants, eight reported a pain condition in the low back, hip or knee. This could possibly have influenced the movement strategies of the participants, including the alignment of the lumbopelvic region. However, all the participants reported that they performed the BBS as part of their weekly training regimen using the selected load, and also that their performance in the BBS was not hindered by their condition, thus they were eligible to participate in the study. Notably, by most injury definitions, these participants would not be considered injured. Seeing that pain conditions are prevalent in about 70% of powerlifters,7 it could be argued that these are a common feature in the population itself and that the included participants are representative of most experienced competitive lifters. However, to further assess the extent of how pain conditions affect lifting performance and kinematics, further comparative studies need to be undertaken.
CONCLUSIONS
Based upon the results of the current study, strength and conditioning coaches and physical therapists who instruct and assess lifting technique in the BBS and/or use the BBS to assess performance or as an intervention, should consider that not only limited ROM, but also a higher ROM in dorsiflexion of the ankle joints could be related to movements of the lumbopelvic region. The results of the present study did not identify any relationship between anthropometric factors, lumbopelvic movement control tests, or measures of ROM in the hip joints and lumbopelvic flexion during BBSs at 70% of 1RM, thus emphasizing the importance of an individual assessment of lifting technique focusing on the goal of the movement.
Acknowledgments
The authors with to thank Jimmy Falk, MSc, and Victor Bengtsson, MSc, for their work with the data collection in part one, and likewise Ulrika Aasa, PhD for help planning of part one. Also, the authors are very grateful to all participants who gave their time and to Boxen Umeå, Sweden, for allowing us to collect data in their facilities.
Declaration of conflicting interest
FÖ is shareholder of AnyMo AB but has not received any financial payments for the study.
All other authors have no conflicting interests.
Corresponding author
Lars Berglund
Umeå University, Department of Community Medicine and Rehabilitation
Umeå University
901 87 Umeå
Lars.Berglund@umu.se
Phone. +4690 786 80 41