Introduction
The medial collateral ligament (MCL) of the knee is frequently injured during sports and physical activities, resulting in various degrees of pain, swelling, and instability. Despite the fact that the MCL is one of the most commonly injured knee ligaments,1 literature on this structure is relatively poor.2 The MCL is a crucial stabilizer of the medial knee joint and is the most commonly injured knee ligament, typically due to direct blows or sudden directional changes during activity producing a valgus forces.3–6
The MCL complex consists of three structures: the superficial medial collateral ligament (sMCL) which is composed of anterior vertically oriented and posterior oblique oriented fibers, and the deep medial collateral ligament (dMCL) which is made of from a thickening of the medial joint capsule, the meniscofemoral and meniscotibial ligaments.7 Injuries to these components often result from combined valgus and external rotational forces on the tibia.5,8 Interestingly, even though the sMCL is farther from the joint axis of rotation of valgus stress, due to the relatively short length of the fibers of the dMCL, it may actually tear before the sMCL when the knee is subjected to a valgus stress.8,9 Most MCL injuries can be managed nonoperatively with good functional outcomes.6,10–12 However, reconstruction is indicated in cases of persistent grade 3 medial knee laxity.3,13,14 Untreated or inadequately treated medial knee injuries can lead to persistent instability, which may result in the failure of meniscal repairs, cruciate reconstructions, and damage to the articular cartilage.15,16 Therefore, accurate diagnosis and management of medial knee injuries are critical.
Accurate and timely diagnosis of MCL injuries is essential for effective management and optimal return to function. Physical examination is the first step in diagnosing MCL injuries, but its reliability can be affected by factors such as the examiner’s expertise, patient tolerance, and the presence of other injuries. Consequently, advanced imaging techniques are frequently employed to confirm the diagnosis and assess the extent of the injury. Stress radiography is a common diagnostic tool used to assess MCL injuries. It allows for the quantification of medial joint space opening under valgus stress, providing valuable information for therapeutic decision-making. However, stress radiography involves radiation exposure and necessitates multiple images to ensure proper femoral and tibial rotation. In addition to stress radiography, magnetic resonance imaging (MRI) is widely used for assessing knee ligament injuries and is considered the gold standard. However, MRI has limitations, including its high cost, limited availability, and inability to provide real-time functional assessment of the ligaments. Additionally, MRI is not suitable for patients with metal implants, pacemakers, or claustrophobia.
Musculoskeletal ultrasonography (MSK-US) is gaining recognition as a reliable and cost-effective method for assessing knee ligament injuries, including those of the MCL. MSK-US offers dynamic, real-time imaging that can be performed in an office setting without the need for radiation. Stress can be applied during the examination to evaluate the opening of both the medial and lateral tibiofemoral compartments. Functional MSK-US is now being used as a diagnostic tool to enhance postoperative radiological outcome measurements. Recently, mean values of medial joint space width in unloaded and standardized loaded conditions using a fixation device have been published.17 Studies have shown that MSK-US is a reliable and accurate tool for assessing medial knee injuries, with comparable results to MRI.13,14 Despite these advantages, MSK-US is not yet a standard modality for assessing MCL injuries, with stress radiography and MRI being more commonly used. However, the increasing use of ulstraound (US) in musculoskeletal conditions highlights its potential as a valuable diagnostic tool, particularly given its portability, low cost, and ability to visualize and compare healthy and injured structures under applied stress.
Advantages of Musculoskeletal Ultrasound
MSK-US employs high-frequency sound waves to produce images of soft tissues, joints, and bones. The principal advantages include real-time imaging capabilities, absence of ionizing radiation, and the ability to conduct comparative assessments of the affected and contralateral sides. Furthermore, its portability and lower cost relative to MRI make it accessible in various clinical settings.
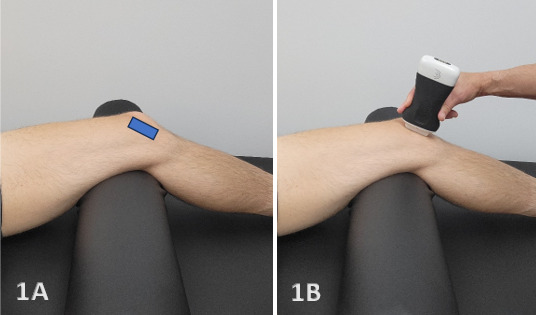
Ultrasound Technique and Diagnostic Criteria for MCL Injuries
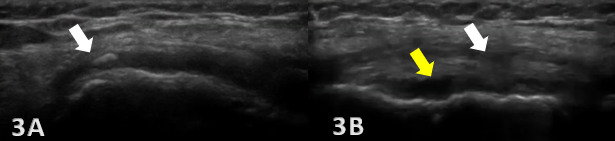
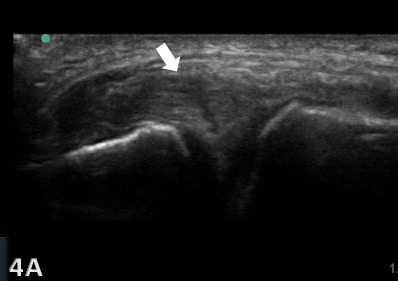
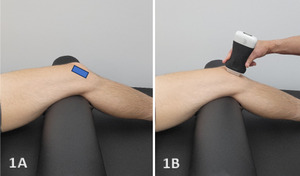
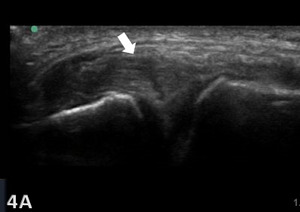
MSK-US is highly effective in identifying the presence and severity of MCL injuries. The ligament’s superficial location makes it readily accessible for US examination, which can be enhanced with high-frequency linear transducers to produce detailed soft-tissue images. Dynamic imaging during knee flexion and extension, not possible with MRI, further improves the diagnostic accuracy of US by demonstrating the static functional integrity of the MCL. The examination involves scanning in both longitudinal and transverse orientations, assessing the ligament for echotexture, continuity, and any associated anechoic (fluid) collections indicating acute injury. Diagnostic criteria for MCL injuries are based on ligament thickness, loss of the normal fibrillar pattern, and the presence of preligamentous fluid. One tip when assessing the femoral insertion of the superficial fibers of the MCL is gently tilt the probe along the MCL curved course to avoid the anisotropic effect of a false hypoechogenicity.18
Clinical Implications
Diagnostic MSK-US offers the ability to visualize these pathological changes in real-time and provides immediate feedback that can inform treatment decisions. Rehabilitation providers can use this information to tailor exercise programs, guide manual therapy techniques, monitor the progression of ligament healing over time, or refer to another provider in instances of tears or ruptures that may require further imaging or surgical intervention. Additionally, ultrasound-guided interventions, such as injections, can be performed with greater accuracy and safety.
Limitations of Musculoskeletal Ultrasound
While MSK-US offers several advantages, including patient comfort and dynamic assessment capabilities, it also has limitations. Operator dependency, a steep learning curve, and variability in image interpretation are notable challenges. Therefore, comprehensive training and experience are essential for maximizing the diagnostic utility of this modality.
Conclusion
MSK-US is an effective and efficient tool for diagnosing MCL injuries of the knee. Its ability to provide immediate, detailed insights into soft tissue integrity makes it an invaluable component of the diagnostic and rehabilitation process. Ongoing training and standardization of ultrasound techniques among rehabilitation providers will be essential to fully realize the potential of MSK-US in clinical practice.
_.png)

_.png)