INTRODUCTION
Anterior cruciate ligament (ACL) injuries are common in sports and the most common treatment for athletes is surgery and rehabilitation.1,2 In this specific population, the rate of reinjury can reach up to 20% and only 65% of athletes returned to their preinjury level.3,4 One possible explanation for these poor outcomes is the persistence of some defiencies that are not targeted during the rehabilitation such as proprioception, proprioceptive adjustment, or neuromotor deficits.
It has been shown that postural control impairments related to a central origin persist in the short and long term after ACL reconstruction (ACLR) and are considered as potential risk factors for reinjury.5–9 Recent evidence has identified neuroplastic adaptation of the central nervous system (CNS) following ACL injuries in particular in afferent pathways.10–12 Ligament injuries significantly disrupt proprioceptive signals and induce nociceptor hyperactivity due to associated inflammatory processes. These factors alter sensory information and its processing by the CNS, leading to cortical reorganization in injured athletes.13–15
A recent studies has revealed that six weeks post-surgical reconstruction, patients show increased cortical connectivity during an unipedal balance tasks without vision compared to healthy subjects.5 This heightened functional connectivity in somatosensory and visual areas may indicate a compensatory mechanism to control postural stability of the injured leg. Long-term (up to 20 years post-injury) injured individuals exhibit reduced adaptability in postural control and greater effort to maintain balance compared to healthy individuals.16 This decreases motor control flexibility in unexpected situations.17,18 These postural control deficits are primarily attributed to alterations in sensory reweighting.
A fundamental contributor to optimal postural control is sensory reweighting.19 It reflects the ability of the CNS to identify and select the most appropriate signal according to balance conditions. For instance, in eyes-closed postural conditions, the CNS mainly relies on proprioception to maintain optimal postural control while in eyes-open balance situations, a reweighting towards vision is observed. The systematic review by Wikstrom et al. confirms an overreliance on visual information during postural tasks in ACL injured athletes.20 This increased dependence on visual signals is considered as a central mechanism of sensory reorganization, compensating for degraded proprioceptive signals due to ligamentous damage to maintain effective postural control and joint stability.21,22
In addition to this intermodal reweighting (proprioception vs vision), an intramodal modality has also been identified (i.e. proprioceptive reweighting). Proprioceptive reweighting is defined as the ability of the CNS to integrate sensory signals from different anatomical locations and select the most appropriate cue according to balance conditions. For example, when standing on a firm surface individuals mainly rely on ankle signals. Conversely, on a foam surface a shift toward a lumbar proprioceptive strategy is observed.19,23,24 However, it appears that in certain pathological conditions such as chronic low back pain or diabetic neuropathy, this ability to reweight proprioceptive signals when postural conditions are changing is impaired.25–28 In addition, recent investigations revealed that a large heterogeneity exists among healthy athletes regarding this proprioceptive strategies.29,30 Most athletes are indeed able to switch from ankle to lumbar proprioceptive signals when moving from a firm to a foam surface (i.e. flexible athletes). However, some individuals seem to adopt an ankle-steered strategy, even on unstable surface (i.e. rigid athletes). It could be considered as a suboptimal strategy since it has been shown that rigid athletes exhibited at-risk determinants for ACL injuries during side-cutting maneuvers.29
Therefore, the primary aim of this study was to compare proprioceptive reweighting between ACLR and control elite athletes. The authors hypothesized that following ACLR, athletes would exhibit a lower ability to switch from ankle to lumbar signals than healthy athletes. The secondary aim of this study was to compare postural control between control and ACLR elite athletes. It was hypothesized that ACLR athletes would exhibit poor balance control.
MATERIALS AND METHODS
Population
This cross-sectional study was conducted in the European Sports Rehabilitation Center of Capbreton, France, from June to September 2023. Based on the primary aim of this study, a priori calculation of the number of subjects required to obtain a statistical power of 0.90 and type 1 error of 0.05 with an effect size of 0.8, showed that at least 68 subjects were needed.29
The inclusion criteria for the ACLR group were as follows. Patients were high-level athletes (top national and international division) who had undergone ACL reconstruction (for first or reinjury) and had to be able to stand on two legs with their eyes closed without pain or instability. For these reasons, the minimum postoperative inclusion period was set at 30 days. Individuals in the control group were high-level athletes free from any recent (six months) lower limb injuries but involved in a rehabilitation process primarily for shoulder, elbow, or wrist injury/surgery. The exclusion criteria for both groups were known neurological or vestibular impairments and spine or lower limb injuries in the prior six months, and pain during the procedure or significant destabilization leading the examiner to prevent the athlete from falling. This study was performed in accordance with the principles of the Declaration of Helsinki. All subjects provided written informed consent, and this study received Institutional Ethics Approval (IRBA02114-49).
Protocol
The procedure was the same as previously detailed by Picot et al.29,30 Participants stood barefoot in a bipedal stance with their arms relaxed by their sides and their head in neutral. Feet position was standardized and vision was prevented using opaque goggles. Two conditions were evaluated: “firm” (standing on the force plates) and “foam” (Physiopad®; 50x41x5cm; 52 kg/m3) surfaces. Four muscle vibrators (VB115, Techno Concept, France) were placed bilaterally on the triceps surae (TS) and the lumbar paravertebral muscles (LPM) by the same experienced experimenter.25 Vibration frequency was set at 80 Hz with an amplitude of 0.5 mm to stimulate the muscle spindles. Computer software automatically and randomly triggered the site of vibration. This also ensured that neither the participant nor the experimenter could anticipate the next vibration site. Each trial lasted for 60s. Recordings began at 20s prior to vibration, then vibration was applied for 20s and the recording continued for another 20s during the re-stabilization period. Force and moment data were collected using portable, uniaxial, dual force plates (Force Decks, FDLite, V.2, VALD, Brisbane, Australia, 200 Hz) to determine center of pressure (CoP) displacement. Raw data were extracted by Force Decks software. Signals were filtered using a Butterwoth low-pass, fourth order filter with a cut-off frequency of 10 Hz. Anterior/Posterior CoP displacement (dCoP) was calculated using custom software developed in Matlab (The MathWorks, Inc., Version: 9.13.0 (R2022b).
Proprioceptive Strategy
Relative Proprioceptive Weighting (RPW) is the ratio between the effects of vibration of the TS and the LPM (absolute TS / (absolute TS + absolute LPM)) on CoP displacement. It provides a reliable indication of individual proprioceptive strategies: an RPW of 1 indicates 100% reliance on ankle afferent input while an RPW of 0 indicates a 100% reliance on lumbar afferent input.
RPW has been shown to be the most reliable indicator of the response to muscle vibration and to establish proprioceptive strategy.25,27,31 The evolution of the relative proprioceptive weighting (eRPW) between the firm and foam surfaces (expressed as a percentage of the RPW on the firm support) was then calculated.29,30
Participants were then dichotomized according to their proprioceptive profile using the eRPW by a second blind assessor. A change < 95% corresponded to a reallocation of signals from ankle to lumbar when standing on foam surface and indicated a flexible proprioceptive profile. Conversely, a change ≥ 105% indicated a rigid profile with an inability to reweight proprioceptive reliance reflecting ankle-dominated strategy.26,29,30 Participants with an eRPW value between 95% and 105% were not characterized to avoid incorrect characterization due to variability in the index.25,29
Postural Control
Postural stability was determined by analyzing the CoP ellipse and CoP velocity area during the 20s of the pre-vibration period on the two different surfaces (firm and foam).32 The data were averaged for trials performed on the same surface and under the same conditions. Higher values indicated poorer postural stability.33
Statistical Analysis
Normality and equality of variances were assessed using the Shapiro-Wilk and Levene’s tests. For the primary aim of the study, eRPW was compared between the groups using a nonparametric independent t-test. The proportions of flexible and rigid subjects in each group were tested using the chi-square (Chi²) test. RPW values were compared using a two-way (Group x Surface) repeated measure ANOVA and post-hoc analysis (Scheffé’s correction) were performed if needed. As postural control data (vCoP and EA) were not normally distributed, they were compared using independent (between-group) and paired (between-surface) nonparametric t-tests. The level of significance was set at 0.05. Effect sizes (Rank biserial correlation, Cramer V or partial η2) were calculated for all comparisons and compared using the Hopkins scale. The statistical analysis was performed using JASP (Amsterdam 0.12.2.0) and G*Power (Version 3.1, University of Dusseldorf, Germany).
RESULTS
Population
Fifty-two ACLR (17 females and 35 males, 23.2±4.9 years) and 23 control elite athletes (8 females and 15 males, 28.2±5.3 years) were included (Table 1). Among ACLR athletes, five underwent reinjury surgery (9.6%). The mean post-operative delay was 162.1 days (SD: 65.1) (Table 1).
Proprioceptive Strategy
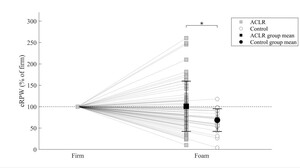
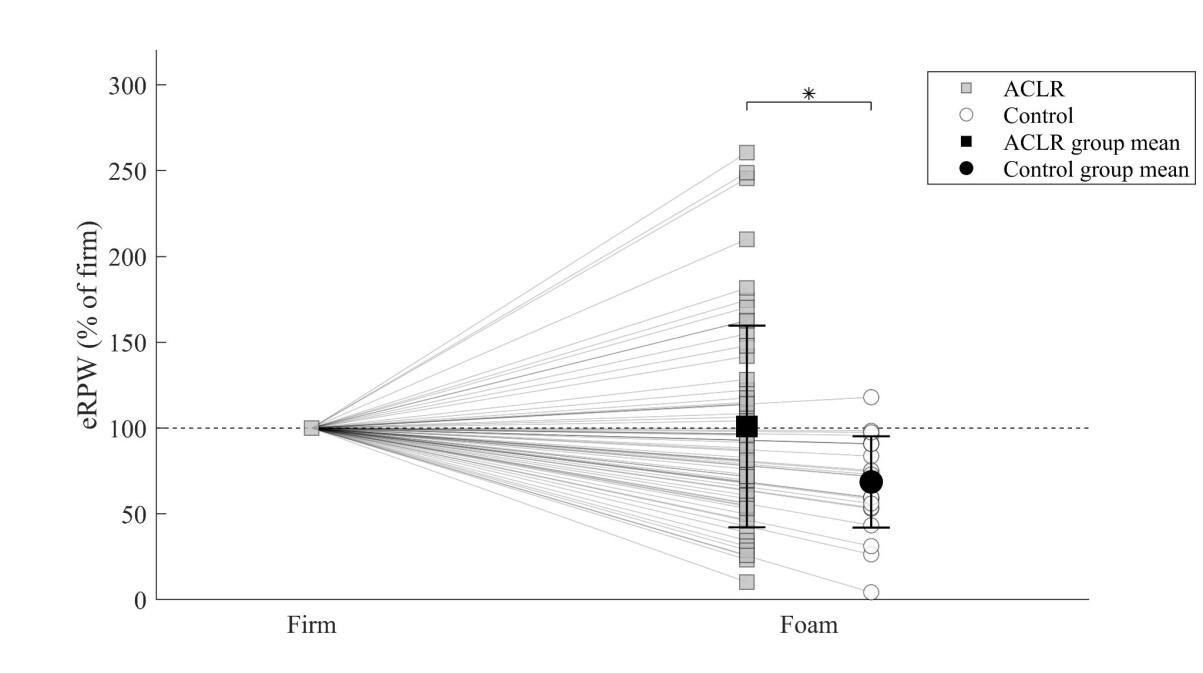
The ACLR group exhibited a higher eRPW value than the control group (100.9 ± 58.8% vs. 68.6 ± 26.6%; p=0.031; Rank biserial correlation=0.314; medium) (Figure 1). In addition, the ACLR group had a significantly lower proportion of flexible athletes and a higher proportion of rigid athletes than the control group (p=0.01, Cramer’s V=0.351, large) (Table 2).
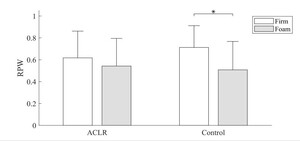
There was a significant interaction (Group x Surface) for RPW values (p=0.05; partial η2=0.014; small). Post-hoc analysis revealed differences only in the control group where RPW values were significantly lower on the foam compared to the firm surface (0.51 ± 0.26% vs. 0.71 ± 0.20%; p=0.002, Cohen’s d=0.845; big) (Figure 2).
Postural Control
On the foam surface, the ACLR group showed increased mean CoP ellipse area compared to the control group (7.95 ± 4.57 cm² vs. 6.25 ± 4.40 cm²; p=0.019; Rank biserial correlation=0.343; medium) indicating poorer postural control. No other differences were observed between the two groups (Table 3). CoP velocity was significantly higher on the foam than on the firm surface for both ACLR (p<0.001) and control groups (p<0.001), as well as the CoP ellipse area for both ACLR (p<0.001) and control groups (p<0.001) confirming the higher difficulty to maintain postural control on foam surface (Table 3).
DISCUSSION
The primary aim of this study was to compare proprioceptive reweighting between elite athletes following ACL reconstruction and a control group. Results revealed higher eRPW values in the ACLR group indicating an inability to reweight proprioceptive signals according to balance conditions.29,30 More specifically, it appears that only the control group was able to significantly shift from an ankle strategy on the firm surface to a lumbar strategy when standing on foam surface (i.e. decrease RPW value, Figure 2). On the contrary, the ACLR group maintained an ankle-dominated strategy regardless of the surface stability. The mean eRPW of ACLR elite athletes was 100.9%, reflecting a strategy close to a rigid profile for the entire group. On the contrary, mean eRPW value of the control group (69%) was similar to values from a previous study obtained from a group of flexible athletes (72%).29 The higher eRPW values found in ACLR athletes can be explained by lower RPW on firm surfaces, which do not decrease on foam surface (Figure 2). It reveals an inability to shift from ankle reliance when the reliability of the signals from this joint is altered by the instability of the support.23–25,34 Conversely, more than 80% of controls were able to operate a proprioceptive reweighting to lumbar signal on foam surface. This reveals a suboptimal proprioceptive postural strategy in ACLR group.30,35 When examining RPW values on firm and foam surfaces, both groups exhibit higher values than those previously reported among healthy populations.26,27,31,36,37 This might be explained by the characteristics of our population, since high level athletes tend to increase reliance on ankle proprioceptive information.33,38
When comparing the proprioceptive strategies between the two groups, a significantly higher proportion of rigid athletes was observed in the ACLR group (38.5% vs. 4.4%). Additionally, the control group exhibited a remarkably high proportion of flexible athletes (83%). Only one study among young healthy athletes reported the proportion of flexible/rigid individuals with 43% of rigid and 57% of flexible.30 Contrary to Picot et al. who used an eRPW cut-off value of 100% to distinguish between rigid and flexible individuals, in the present study, the dichotomization was made using an eRPW > 105% for rigid and eRPW < 95% for flexible athletes in order to avoid incorrect characterization of participants due to the variability of this index.25,29,30 In addition, the population studied by Picot et al. was composed of young subelite healthy handball players.30 Both type of sport and level of practice may play a role in proprioceptive reweighting strategy.24,33,38,39 It might be possible that most healthy elite athletes exhibit flexible strategy compared to non-expert individuals. Further studies with larger sample sizes are needed to better understand the specific proportion of flexible/rigid and the role of sports expertise in proprioceptive postural strategies according to the type of population.
The secondary aim of this study was to compare postural performance between ACLR athletes and a control group. Data confirm previous results revealing bilateral deficits in both static and dynamic postural control, in single-leg and double-leg stances following ACLR. Single-leg assessments showed impairment for both the affected and unaffected limb. These bi and unilateral deficits are found in the short and long term.7,40–43 It is worth mentioning that only significant differences between the two groups were observed on foam surfaces. The moderate effect size as well as the absence of difference on firm surface between the two groups could be explained by the fact that individuals were elite athletes and bipedal tasks might not be challenging enough.44 It seems assessment of postural control deficits in challenging tasks, such as unstable surfaces, single-leg tasks may improve the characterization of postural control deficits.44,45
Overall, the results indicate possible functional modifications of the CNS in elite athletes following ACLR, especially in areas involved in postural control. Over-reliance on visual signals after ACL injury have been identified as a probable consequence of altered proprioceptive signal.20 Indeed, an hyperactivation of lingual gyrus has been shown after ACLR which could be considered as an adaptation mechanism of the CNS to maintain postural control by reweighting altered proprioceptive signals to visual signals.46–48 Although the CNS attempts to compensate for this proprioceptive impairment, central alterations persist, which may explain the ongoing postural control deficit after an ACL injury. Indeed, Grooms et al. found greater activation of the contralateral cerebellum and the pre-motor area, and the ipsilateral secondary somatosensory cortex in individuals who underwent an ACLR, all of which are highly implicated in postural control.47 The recent scoping review from Vitharana et al. confirmed impaired central processing within the somatosensory and visual systems and underlined the impact of these neuroplastic changes on balance control.22 These results suggest that cortical and subcortical deficiencies after ACLR may be involved in the persistence of a postural control deficit after ACLR.6,46,47 Further imaging studies are needed to better understand which brain regions are involved in the proprioceptive reweighting process and whether functional connectivity between brain regions responsible for posture and sensory integration is impaired among rigid individuals.
It has been shown that several regions of the CNS involved in proprioceptive reweighting such as the somatosensory, pre-motor and motor cortex exhibit altered activity after an ACL rupture.46,47,49 This could explain the lack of proprioceptive reweighting found in ACLR subjects in this study. In addition, impaired functional connections between the left primary sensory cortex and the right posterior lobe of the cerebellum were observed in athletes who go on to suffer an ACL injury. These connections are considered essential for motor control, thus functional impairments of the CNS especially between brain regions implicated in sensory integration during postural control might increase the risk of ACL injury.50,51 It has been suggested that these central adaptations could be responsible for reinjury after ACLR, since it limits the ability of athletes to adapt to complex and unplanned game situations.52
Recently, Picot et al. showed that lack of proprioceptive reweighting in postural strategy is associated with at-risk biomechanics and neuromuscular control for ACL injuries during sidecutting maneuvers.29,53,54 Poorer postural control was also observed among rigid athletes during bipedal stance tasks which is also a major risk factor for primary and secondary ACL injuries.8,9,30,40
These results suggest that following ACLR elite athletes exhibiting suboptimal (i.e. rigid) proprioceptive strategies could be more likely to suffer from a reinjury. Further studies are needed to determine whether a lack of proprioceptive reweighting is a risk factor of ACL (re)injury.
Strengths and Limitations
This is the first study to evaluate proprioceptive reweighting abilities in athletes undergoing ACLR. It is also the first to use vibration as a method to probe the CNS in this population without imaging or electroencephalography, which is more functional and closely approximates postural control. This could be considered as a CNS assessment tool that can be easily used in clinical practice to personalize rehabilitation and be part of return-to-sport criterion.
This study had several limitations. First, due to the design of this study, it is not possible to determine whether the lack of proprioceptive reweighting observed in ACLR athletes was present before the injury. Future studies should examine preinjury data to confirm the link between proprioceptive reweighting and ACL rupture.
Furthermore, the exact effects of rehabilitation on proprioceptive reweighting remains to be established. The mean post-operative delay for the ACLR group was five months. It remains unclear whether proprioceptive reweighting impairments persist in the long term. Thus, further research is needed to determine the progression or potential recovery of these proprioceptive deficits over time. Future longitudinal studies should evaluate the evolution of proprioceptive reweighting during rehabilitation, and whether exercising can transform rigid to flexible patients. Since athletes who suffer an ACL lesion are 30 to 40 times more prone to recurrences than those who did not, lack of proprioceptive reweighting and impaired postural control should be evaluated and targeted during the rehabilitation.3,55
On another note, as bipedal testing on a unilateral injury may have limitations and could fail to reveal important asymmetries in weight-bearing strategies for each individual limb, it would be valuable to conduct a bilateral single-leg assessment to identify potential differences in proprioceptive reweighting capabilities between the injured and healthy limbs.55
Additionally, the authors did not conduct a subgroup analysis based on the type of graft (hamstring or quadriceps), associated injuries (antero-lateral ligament suture or lateral tenodesis, meniscal resection or suture), or first or reinjury surgery because of the low number of athletes. Future studies should include larger cohorts to evaluate the effect of these differences on proprioceptive reweighting.56
Moreover, the small sample size likely contributed to the high variability observed. This variability is especially in the ACL group and is possibly due to variable postoperative times. Such variability in proprioceptive reweighting is common with this methodology.
The average age of the ACLR group was lower than that of the control group (23.2 vs 28.2 years). Even if it has been shown that age could influence proprioceptive reweighting capabilities in elderly, a difference of five years seems insufficient to induce variations in proprioceptive reweighting capabilities.24,39 Furthermore, given that the proprioceptive system is fully matured at this age it seems unlikely that this could have influenced the results.57
CONCLUSION
Elite athletes who underwent ACL reconstruction exhibit a lack of proprioceptive reweighting, and a higher proportion of rigid individuals compared to a control group. More specifically, they show a lack of ability to reweight proprioceptive signals when moving from a firm to a foam surface. In addition, poorer postural control was observed on foam surface among ACLR athletes. These results highlighted central alterations associated with suboptimal strategy that could increase the risk of reinjury. Further studies are needed to assess whether these alterations exist prior to injury and if these can be considered potential risk factors for reinjury.
Conflicts of Interest
The authors report no conflicts of interest.