INTRODUCTION
Anterior cruciate ligament (ACL) injuries are prevalent in the United States, with 1 in 3000 persons sustaining an ACL rupture, and the incidence appears to be increasing.1 The current standard of care for athletes and active individuals with an ACL injury is arthroscopic ACL reconstruction (ACLR), and roughly 100,000 ACLR surgeries are performed annually.2 Patients with ACLR participate in months of rehabilitation to address impairments in knee range of motion, lower extremity strength, and lower extremity neuromuscular control before attempting to return to activity and/or sport participation.3 Despite extensive rehabilitation after ACLR, the risk for a secondary ACL injury is high.4–6
A patient’s readiness to return to sport participation after ACLR is often determined from clinical tests, including single-leg hop tests.7 Research suggests that patients might demonstrate good performance on motor tasks like single-leg hop tests but require greater attention and neural effort to perform the motor task.8 This neural compensation, called neurocognitive reliance,9 could put patients at risk for secondary injury during sport participation because visual, auditory, and tactile information in the sporting environment must also be processed. Neurocognitive reliance can be exposed by pairing a motor task with a cognitive task (i.e., dual task training), such as reaction tests.9 Few studies have administered reaction tests to patients with ACLR, and these have focused on reaction time during simulated driving10 and tapping lights while standing.11
Advanced neuromuscular training is recommended to prepare patients for the physical demands of sport participation.12–14 Typical interventions including plyometrics, dynamic stability exercises, and agility drills to provide physical challenges that exceed traditional rehabilitation and address residual neuromuscular deficits that could increase risk for re-injury.12–14 Post-training improvements include better hop test performance, agility, and self-reported knee function.14–16 Dual-task challenges, such as ball catches, may be implemented during training to challenge motor control and improve dynamic knee joint stability while simulating sport conditions, but these are not the primary focus. It is unknown if advanced neuromuscular training improves performance on reaction tests, including physical and cognitive measures.
This study examined changes in performance on visuomotor reactions tests and single-leg hop tests following advanced neuromuscular training in patients with ACLR. The hypothesis was that performance would improve less on reaction tests than on single-leg hop tests. Study findings can provide insight into dual-task performance after ACLR and the impact of advanced neuromuscular training.
METHODS
Study Overview
This study used a quasi-experimental pretest-posttest design. Study participants completed testing immediately before and after participating in an advanced neuromuscular training program.
Participants
Patients with ACLR who enrolled in an advanced neuromuscular training program between January 2014 and June 2015 were eligible for this study. Inclusion criteria were: (1) age 14–30 years at the time of surgery; (2) primary ACLR; (3) participated in organized sports that require cutting, jumping, or pivoting before injury; (4) intention to return to pre-injury activity level at the time of study participation. In addition, patients had to meet eligibility criteria for participating in advanced neuromuscular training: (1) at least five months postoperative; (2) symmetrical knee extension and knee flexion within five degrees of the contralateral knee; (3) able to hop vertically on the surgical leg without knee instability or pain; (4) trace effusion or less; and (5) surgeon approval. Exclusion criteria included previous lower extremity surgery or concomitant surgical procedures that alter postoperative rehabilitation (i.e., concomitant meniscal or ligamentous repair or cartilage stimulating procedure). Study criteria were meant to identify patients with good potential to return to sport after ACLR. The study protocol was approved by the Institutional Review Board at the authors’ facility.
Demographic Variables
Demographic variables collected from the electronic medical records included age, gender, body mass index (BMI), graft source, surgical side, concomitant surgeries, pre-injury sport, and time from surgery to pre-training and post-training testing.
Advanced Neuromuscular Training Program
The advanced neuromuscular training program has been described previously.16 Briefly, the training program is cash-based (USD 300 at the time of the study) and offered to patients after they finish standard rehabilitation and received surgeon clearance to initiate a return to sport participation. Patients in the study were enrolled in the training program and were not compensated for the cost of the training. Training sessions were held in group format at a frequency of two times per week over five weeks and duration of two hours per session for a total of 20 hours of training. Groups consisted of up to six patients supervised by a physical therapist and athletic trainer who provided feedback on movement patterns.16,17 Each session began with a dynamic warm-up that lasted approximately 20 minutes, then patients performed the neuromuscular exercises prescribed for that session for approximately one hour, and the session ended with cool down exercises of stretching or foam rolling. Neuromuscular exercises were categorized as dynamic stability, plyometric, agility, and strengthening, and exercises were progressed in physical demand over the course of training (Table 1). If necessary, exercises were modified for patient safety. Some exercises incorporated a partner ball toss (e.g. ball catch while kneeling on or jumping on/off the BOSU ball) or were performed with reaction to a verbal command (e.g. cone drills) or ball-bounce (e.g., partner race to reaction ball), but this was intended to improve dynamic knee stability,18 not to resolve neural compensation. The volume of dual-task challenges in the advanced training program was low and did not exceed more than two exercises per session.
Testing
Reaction tests were administered on a commercially available system consisting of a platform with five yellow dots on the surface connected to an electronic visual display (The QuickBoard, QuickBoard LLC, Memphis, TN) (Figure 1). The arrangement of the dots is two on the right side of the platform, two on the left side of the platform, and one in the center as on the number five side of a dice. Force sensors are located underneath the dots, and the arrangement of the dots is replicated on the visual display. For the double-leg reaction test, patients stood with their feet positioned on either side of the center dot. Target dots were randomly presented on the visual display. The patient used the right leg to touch targets on the right side, the left leg to touch targets on the left side, and either of the legs to touch the center target. After the patient touched a target correctly, the next target was shown on the visual display. The test was performed for 20 seconds, and the number of correct touches and incorrect touches (i.e., errors) were recorded. The single-leg reaction test was first completed with the non-surgical leg. Patients stood on the non-surgical leg positioned on the ipsilateral side of the center dot (e.g., right side of the center dot when the right leg was tested). Target dots were randomly shown on the visual display, and the patient hopped to the corresponding dot on the platform. When the target dot was touched, the next target was shown on the visual display. The test was complete when the patient had correctly hopped to 10 targets. Hop time was recorded in seconds, and the number of errors (i.e., incorrect touches) was recorded. The test was then repeated with the surgical leg.
The single leg hop tests were forward hop for distance, triple hop for distance, crossover triple hop for distance, and a six-meter timed hop.19 The non-surgical leg was tested first. For each hop test, patients received one or more practice trials and then performed three maximal effort test trials. The best performance was recorded in centimeters. A limb symmetry index was calculated as [(surgical limb performance/non-surgical limb performance) x 100] for distance measures and [(non-surgical limb performance/surgical limb performance) x 100] for the timed hop test. Testing was then repeated on the surgical leg.
Statistical Analysis
No power analysis was conducted for this study. Data were analyzed with SPSS version 28 (IBM Statistics,). Descriptive statistics were computed for all variables, including means and standard deviations for continuous variables and frequency distributions for categorical variables. The Shapiro-Wilk test assessed normality of the measures.20 The double-leg reaction test measures were found to have non-normal distribution due to outliers with a high number of errors; however, the data points were confirmed and the variables are continuous, so parametric statistics were used for all analyses. Alpha was set at 0.05 to determine statistical significance.
Pre- to post-training changes in the number of correct touches and errors on the double-leg reaction test were examined with paired t-tests. Separate repeated measures general linear models (limb x time) examined changes in hop time and the number of errors on the single-leg reaction test. Although not the primary purpose of this study, pre-to-post training differences in the limb symmetry indexes on each single leg hop test were examined with paired t-tests. This analysis was intended to confirm expected improvements in physical performance following advanced neuromuscular training.15 Effect size (Cohen’s d) was computed for the pre- to post-training difference in number of correct touches on the double-leg reaction test, surgical side hop time on the single-leg reaction test, and surgical side hop distance or hop time on the single-leg hop tests. An effect size of 0.2 is considered a small effect size, 0.5 is considered moderate, and > 0.8 is considered large.21
RESULTS
Participant Demographics
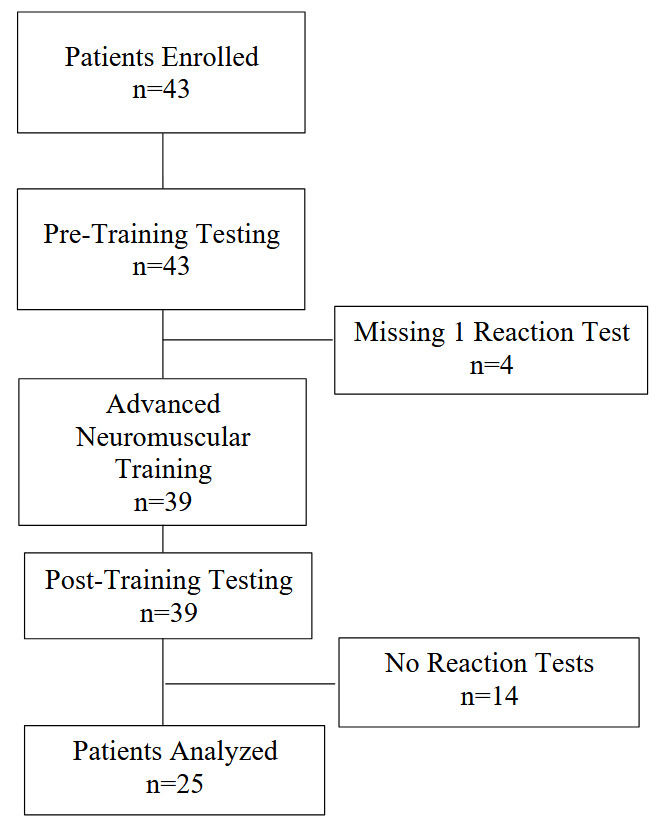
A total of 43 patients were enrolled in the study and completed pre-training testing, but four patients were excluded from analysis for missing data at pre-training and an additional 14 patients were excluded for missing data at post-training (Figure 2). The missing data resulted from a combination of technological issues and a change in the testing protocol. Thus, only the data from the 25 patients who completed the entire study were included in the analysis.
Demographic information is found in Table 2. No significant differences were found in gender or age between patients analyzed and those excluded from the analysis (p>0.05). The patients in the analysis included 54% females and 73% had ACLR with bone-patellar tendon-bone autograft.
Pre- to Post-Training Change in Performance on Reaction Tests
Scores on the reaction tests are found in Table 3. For the double-leg reaction test, the number of correct touches significantly increased from pre- to post-training (p<0.001), but there was no significant change in the number of errors (p=0.637). The highest number of errors at pre-training and post-training was 12. For the single-leg reaction test, the main effect of time was significant for hop time (p=0.003), indicating that hop time improved in both the surgical and non-surgical legs. No significant main effect was found for number of errors on the single-leg reaction test (p>0.05). At pre-training, the highest number of errors on the surgical side was 9 and on the non-surgical side was 12. At post-training, the highest number of errors on the surgical side was n=6 and on the non-surgical side was n=9.
Effect Sizes for Change in Performance on Reaction Tests and Single-Leg Hop Tests
Scores on the single-leg hop tests are shown in Table 4. Limb symmetry indexes on each single-leg hop test significantly improved from pre- to post-training (p<0.05). Effect sizes for the pre-to post-training change in test performance varied according to the difficulty of the test; specifically, effect sizes decreased in magnitude from single-leg hop tests to double-leg reaction test to single-leg reaction test (Table 5). All effect sizes were moderate to large.
Exploratory Post-Hoc Analysis
In the dataset, 13 patients had post-training limb symmetry indexes ≥90% for all single-leg hop tests and 12 patients failed to achieve the criteria for at least one single-leg hop test (one hop test: n=3; two hop tests: n=2; three hop tests: n=3; four hop tests: n=4). Independent samples t-tests compared post-training results on the double-leg reaction test and single-leg reaction test (surgical side only) between groups. No significant group differences were found in correct touches (p=0.737) or errors (p=0.771) on the double leg reaction test or in surgical side hop time (p=0.073) or errors (p=0.237) on the single-leg reaction test (Table 6).
DISCUSSION
This study examined changes in performance on reaction tests (dual-task) and single-leg hop tests (single-task) following advanced neuromuscular training in patients with ACLR. The study hypothesis was supported. Performance improved from pre-training to post-training on both reaction tests and single-leg hop tests, but the effect sizes were generally lower for reaction tests than for single-leg hop tests. Additionally, the mean number of errors on the reaction tests did not significantly change. The findings indicate that advanced neuromuscular training improves motor task performance in patients with ACLR but does not prepare them as well for performing motor tasks that include a cognitive challenge (i.e, visuomotor reaction test).
Results of this study support the concept of neural compensation, specifically neurocognitive reliance, after ACLR.8 Neural cognitive reliance is demonstrated in the current study by improvement in motor performance on the reaction tests without a significant improvement in the number of errors. The highest number of errors in any patient on the single-leg reaction test was lower following training, and this indicates that individual results might differ from overall group results. Future work is needed to understand if neurocognitive reliance occurs in all, or only some, patients with ACLR and how advanced neuromuscular training should be augmented to reduce neurocognitive reliance.
The dual-task test used in this study was a lower extremity visuomotor reaction test. Study results add to a small body of literature on reaction tests in patients with ACLR and could be used as comparative data in future studies. The exploratory analysis found no significant difference in post-training reaction test performance based on clinical criteria for return-to-sport (i.e., ≥90% limb symmetry index on single-leg hop tests). The finding adds to knowledge that single-task motor performance and dual-task motor performance are not mirrored.22,23 It is yet unknown which dual-task testing methods provides meaningful insight into readiness for sport participation after ACLR. Visuomotor tests have been recommended, and a variety of reaction tests demonstrate good reliability8,24; however, interpretation of reaction test performance requires a benchmark. Alternatively, a motor task (e.g., single-leg hop tests) can be administered with and without a cognitive challenge so that a “dual-task cost” metric can be computed.9 For this method, the cognitive challenge requires thoughtful selection, and equipment may be needed to acquire an objective measure. As visuomotor tests are developed, it will be important to understand the association with return-to-sport outcomes to determine their contribution within a comprehensive testing battery.
It has previously been posited that neuromuscular training with a focus on biomechanical factors (i.e., movement control) might be inadequate to address neural compensation after ACLR.8 This is supported in the current study by the smaller effect size change in reaction test performance compared to single-leg hop test performance. The advanced neuromuscular training program incorporated some dual-tasks conditions, such as catching a ball while balancing on an unstable surface, to challenge postural stability and dynamic joint stability, but a greater volume of dual-task challenges appears to be needed. It is yet unclear what training methods might be most effective. Positive changes in dual-task performance been reported in uninjured athletes after visuomotor25 and cognitive training on a computer,26 suggesting different methodologies for providing neurocognitive tasks in rehabilitation may be effective in minimizing neurocognitive reliance.
Strengths and Limitations
The strengths of this study are the application of novel reaction tests in patients with ACLR before and after participation in an advanced neuromuscular training program. The results of this study provide insight into dual-task visuomotor performance after ACLR as well as the impact of advanced neuromuscular training. The single-leg hop tests in the testing protocol are commonly used in return-to-sport testing7 and provided a comparator to the reaction tests. The primary limitation of this study is the small sample size, which is partly due to the relatively large attrition from the initially included population. The attrition could contribute to bias in the study if patient characteristics were different between those who did or did not complete the study. Study bias may also be present because the advanced training program was cash-based, which means patients needed to be motivated and have financial means to participate. Another limitation is potential confounding from the dual-task challenges in the advanced neuromuscular training program that may have contributed to improved performance on the reaction tests. More of these dual-task challenges, or different challenges, may be needed for improving errors on the reaction tests. An additional limitation is the lack of a control group that would aid the understanding of performance changes that could be attributed to recovery over time. A final limitation is the lack of isokinetic quadriceps strength data. At the time of this study, the clinic did not own an isokinetic dynamometer. Knowledge of quadriceps strength would aid the interpretation of neural compensation as patients with lower quadriceps strength (i.e., better motor reserve) are expected to demonstrate greater neural compensation.9
CONCLUSION
Motor performance in patients with ACLR improved after advanced neuromuscular training but the effects on visuomotor reaction tests were less than those effects seen on single-leg hop tests. The results suggest the persistence of neurocognitive reliance after ACL and for more dual-task challenges in advanced neuromuscular training to minimize neurocognitive reliance that might increase the risk for re-injury when returning to sport.
Conflict of Interest
The authors declare that they have no conflict of interest.
_and_single-leg_(b)_reaction_tests.jpg)
_and_single-leg_(b)_reaction_tests.jpg)