INTRODUCTION
Upper extremity injuries are prevalent across all levels of baseball.1 Three quarters of adolescent baseball players report constant pain in their throwing arm, with injury incidence estimated at 0.86 and 1.39 per 10 ,000 athlete-exposures (AEs) respectively.2,3 Higher injury rates occur at collegiate level, with 1.85 to 5.75 upper limb injuries per 1000 AEs in game situations, with 25% requiring absence from play for 10 days.4 Major League Baseball (MLB) players are at greatest risk, with an average of 55 days of time loss due to shoulder injury5; this incurs substantial costs on MLB clubs, estimated at $400 million dollars each year.5
A commonly utilized metric in maintaining optimal performance in a baseball player’s dominant throwing shoulder, is to obtain passive range of motion (PROM) measurements of internal and external rotation (IR/ER). The traditional standard clinical assessment of shoulder rotation PROM involves placing the athlete in the supine position, lying completely flat on their back, with the lower extremities fully extended. A goniometer is then used to assess shoulder rotational PROM with the athlete’s test arm typically held in either 0° or 90° of humeral abduction during testing.6–8 Although this standard method is reliable, it does not reflect the global torsional complexity of throwing mechanics.
It is important to recognize that the standard method to assess the rotational PROM of the throwing shoulder is to place the shoulder in a position of maximal tension locally at the shoulder, in combined abduction and external rotation. These combined motions do acknowledge the tissue tension that is occurring locally at the glenohumeral joint but neglects the potential impact on shoulder PROM once the torsion of the throw moves the trunk into contralateral rotation. For example, throwing a baseball encompasses movement throughout the kinetic chain at the shoulder, trunk, pelvis, hip joints, and lower extremities, and includes five phases of movement - wind up, cocking, acceleration, deceleration, and follow through.9
The transition from the early to late cocking phase is central to developing the torsion needed for throwing performance, as this rotation occurs and tissue elongation maximizes the length and tension on the musculoskeletal system, referred to as “system tension”. This release of stored elastic system tension transmits potential to kinetic energy at the ball release phase of throwing.9–14
Musculoskeletal impairments at any point along the kinetic chain can have an impact on throwing performance and injury risk.9 Empirical data show that the recruitment of the scapulothoracic muscles during throwing is sensitive to changes in lower extremity and trunk position,15 and that the risk of shoulder and elbow injury is increased in athletes with reduced hip extension on the same side as the throwing shoulder16 or internal rotation of the thrower’s stride leg.17 Increasingly, studies appear to support that the throwing shoulder is affected by the global kinetic chain, yet the currently utilized standard supine testing position used to assess shoulder rotational PROM does not capture any aspect of the sport specific throwing motion outside the shoulder.
There is a precedent at the hip joint, for the idea that PROM assessments do not appear to reflect the task of the athlete that is being assessed. Sport specific testing positions have been developed for assessing lower limb hip PROM in the kicking athlete. Tak and Langhout developed a clinical test14 that recreates the system tension arc associated with kicking, using a combination of hip extension, abduction, adduction, and rotation, with contralateral rotation of the trunk and pelvis. The test has been reported to be reliable and can accurately differentiate asymmetries in kicking athletes with groin pain.18 As Tak, et al.19 observed, the standard traditional supine hip PROM testing position in soccer players lacks similar face validity, as does the standard traditional supine testing position of shoulder rotation PROM in baseball players. Neither of these traditional standard positions used to measure hip or shoulder PROM incorporate many of the key trunk and pelvic positions, and the accompanying torsional movements that occur during a maximal throw or kick.
Overhead throwing athletes should be assessed using a sports specific PROM test, which may better reflect the task specific global torsional positioning observed during throwing motion. This study proposes a novel clinical test to quantify shoulder rotational PROM in baseball players, which is underpinned by the global three-dimensional tension that is experienced during overhead throwing. The development of the FAST-SHDR test was built on the concept of interconnected muscle chains, connecting the lower to upper extremities via the trunk, which have been increasingly recognized in current literature.20,21
The key objectives were to determine the intra-rater reliability of the novel PROM test, and to establish reference values in throwing and non-throwing (control) populations. Construct and discriminant validity were also explored by comparing shoulder rotation PROM within (dominant vs non-dominant) and across populations (baseball vs control). It was hypothesized that the greatest variations to sport specific PROM would be seen in the dominant shoulders of baseball athletes.
METHODS
Participants
The study protocol was approved by the Institutional Review Board at High Point University (Protocol number 201508-387). Prior to any testing the potential risks of all experimental procedures were explained fully to all participants. Prior to participating in the study, all participants read and signed the informed consent form.
A sample of 31 collegiate male baseball players from the Division 1 baseball team were recruited during the preseason period of the 2018/19 playing season. The total number of roster players invited to participate was 33, and 33 total players volunteered (14 pitchers and 19 field players), but two were unable to participate on the day of testing secondary to pain from a previous weight room session (Figure 1).
The inclusion criteria in the study stated players must have been aged > 18years at the time of informed consent. The exclusion criteria included any current shoulder or elbow injury or shoulder or elbow injury in the previous 12 months, or pain reported during, or at the time of testing, that would not allow the participant to be assessed.
A convenience sample of 18 non-baseball research participants volunteered from a class of 66 physical therapy students from the same university (10 females and 8 males; age: 21.6 + 1.6). In an effort to allow the control participants to fully understand the aim of the study, all students were given a demonstration and thorough explanation of the procedure and why it was being performed, prior to giving their informed consent to participate in the study. Participant recruitment and testing was undertaken by three final year High Point University Doctor of Physical Therapy students (JMP, CLB, JAC), under the supervision of two experienced licensed physical therapists and clinical researchers (SLD, CMB).
Testing Procedures
FAST-SHDR PROM Testing
A novel sport specific test (FAST-SHDR) was developed to quantify shoulder internal and external rotation. The FAST-SHDR test is performed by having the athlete initially positioned in supine hook-lying, with the shoulder to be tested off the side of the plinth. While maintaining the supine hook lying position, the pelvis is passively rotated 90 degrees contralateral to the tested arm, which remains off the side of the plinth. Once the pelvis is rotated, the legs are secured by placing a strap around the knees, securing the legs to the plinth with a belt, while keeping the athlete flat on their back. The legs rest on the plinth when the strap is placed around the lower extremities, the strap serves to provide stability as the trunk is rotated and the arm is moved into horizontal abduction, thus, the strap does not force the legs to the table, rather, the strap holds the legs in position as tension is taken up more proximally (Figure 2).
Although the FAST-SHDR test could be performed by a single clinician, in this study the test was performed most efficiently by using two assessors. Assessor 1 positioned the test shoulder in 90 degrees of shoulder abduction, then into maximal passive horizontal abduction taking up spinal rotation slack as well, and then lastly rotated the shoulder to the passive end range testing direction (internal or external rotation). The end range of passive shoulder ROM was determined by soft tissue end-feels and all the available slack in the movement was taken up during the movement. Assessor 2 placed a bubble inclinometer on the distal styloid process of the ulna to determine shoulder angle. Assessor 1 was blinded to PROM angles for the duration of the testing process. The process was then repeated for the opposite shoulder with the testing order randomized (dominant vs non-dominant extremity) (Figure 3).
The standard testing position of shoulder rotation PROM began with the participants lying supine with the lower extremities in a fully extended and in a comfortable resting position. As participants were in the supine position the arm was brought passively into 90 degrees of shoulder abduction and 90 degrees of elbow flexion. A stabilizing hand was brought to the anterior shoulder with a slight posterior glide to maintain glenohumeral joint congruency. These steps were performed to fully replicate the current standard method of shoulder rotation PROM assessment used by the baseball athletic trainer at the university during pre-season screening (Figure 4). Reliability data were determined based on three repeated tests on both sides, during a single session, for each of the test conditions.
Statistical Analysis
FAST-SHDR reliability was initially determined through ICCs, using a two-way, mixed effect model (absolute agreement).22 Standard Error of Measurement (SEM) was then calculated using the formula: SEM = SD √1-r (SD = standard deviation of sample scores; r = reliability of scores) and Minimum Detectable Change (MDC) was calculated using the formula: MDC = 1.96 X √2 X SEM.23 MDC was expressed both in absolute terms, and as a percentage of the grand mean.
Between and within group differences were assessed using relevant t-tests, effect sizes (Hedges g) and absolute differences with 95% confidence intervals (CIs). Normality of data distribution was assessed visually using Q-Q, Box plots, and histograms. P values were set at 0.001 a priori due to the exploratory nature of the study, and all analyses were conducted in SPSS v21 (IBM, USA). ICCs were interpreted using the lower bound 95% confident interval of each estimate, as follows: <0.5 = poor, between 0.5 and 0.75 = moderate, between 0.75 and 0.9= good, and >0.90 =excellent reliability.22
3. RESULTS
On the day of testing, two baseballer players were unable to undergo the test procedure secondary to pain reported from a recent weight training session. Thus, 31 total baseball players completed the protocol on the day of testing. None of the 31 participants reported any pain or adverse effects because of the testing procedures.
Reliability
The participant demographics were (M/SD): age: 19.2+ 1.2 y; weight: 86.1+ 7.7 kg; height: 185.5+ 5.39 cm. Intra-rater reliability and key clinimetrics of the sport specific FAST-SHDR test are shown in Table 1. The test shows good to excellent reliability with ICCs ranging from 0.95 (0.89 to 0.98) to 0.96 (0.92-0.98). MDC for FAST- SHDR rotation ranged from 6.8° (IR) to 11.1° (ER), which represents 10.6% and 15.2% of mean scores respectively.
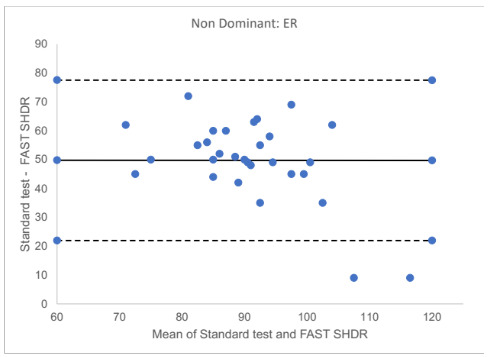
Bland and Altman plots were used to visually examine the level of agreement between PROM when measured in non-dominant (Figure 5) and dominant (Figure 6) arms and across populations (baseball and controls). In both Figures 5 and 6 the solid black line represents the mean difference between the tests, while the dashed lines indicate the 95% limits of agreement. The largest differences were recorded for ER, with mean differences of 49.7° (95% CI 44.5 to 55.1) and 50.7° (95% CI 44.7 to 56.7) at non-dominant (Figure 5) and dominant (Figure 6) shoulders respectively.
Sport Specific Rotation Testing (FAST-SHDR) vs Standard Rotation PROM Testing
Normative testing data for the Division 1 baseball players is summarized in Table 2. Shoulder rotation PROM was normally distributed with no evidence of floor or ceiling effects. Sport specific FAST-SHDR IR was significantly lower in the dominant shoulder vs non-dominant (p <0.0001), however this pattern was reversed for ER (p <.0001).
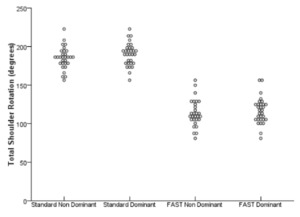
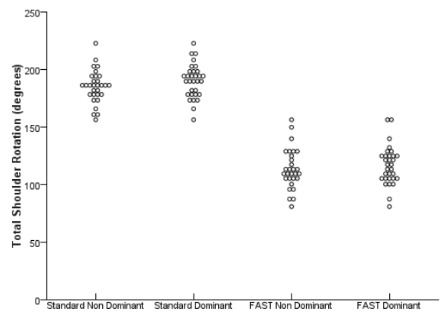
The correlation between sport specific and standard test scores were weak to moderate for ER scores, and strong for IR scores (Table 2). Total arc shoulder rotation (Figure 7) was also consistently lower with sport specific testing compared to standard, at both dominant (MD 74.0°; 95% CIs 66.9 to 81.1 degrees; p<0.001) and non-dominant shoulders (MD 71.4°; 95% CIs 64.8 to 78.0 degrees; p<0.0001) (Table 2).
4. DISCUSSION
The study introduces a novel sport specific test (FAST-SHDR) for assessing shoulder rotation PROM. The test was developed to acknowledge the multisegmented and torsional nature of throwing. The test demonstrated good to excellent intra-rater reliability, with MDC scores ranging from 6.8° to 11.1° for IR and ER respectively. These figures compare favorably to traditional standard method of assessment of shoulder IR / ER (based on full supine lying, 90° shoulder abduction and 90° of elbow flexion), where MDC is estimated at 5 - 10°.24,25 The hypothesis of this study, that the greatest restrictions to sport specific rotation PROM (FAST-SHDR) would be seen in the dominant shoulders of baseball athletes was confirmed.
A key difference between traditional shoulder rotation PROM testing methods, and the new sport specific assessment, is that the FAST-SHDR test places the patient in a position that produces a similar “tension arc” position of the trunk and pelvis during the terminal phase of an overhead throw. The sport specific PROM scores were consistently lower than standard assessment scores, in both isolated rotation and total arc of motion. The FAST-SHDR test is clearly measuring an independent construct compared to the standard testing methods. The authors suggest that shoulder PROM during sport specific testing is limited by a combination of local passive stabilizers (e.g. ligament and capsular tissue) and more global passive restraint from musculotendinous and fascial units across the shoulder, torso, and pelvic region (e.g. the anterior functional line, posterior functional line, and spiral line).14,20,26,27 The FAST-SHDR test specifically targets the anterior interconnected fascial muscle chain (pectoralis major, rectus abdominis, and adductor longus muscles) and the posterior fascial muscle chain (gluteus maximus, lumbodorsal fascia, and latissimus dorsi) which have both been reported via systematic review as having strong evidence to support their existence.20 In a 2018 consensus statement published in the British Journal of Sports Medicine, the authors stated that “improved assessment technology” would be needed to advance fascial system research.21 The FAST-SHDR assessment begins to contribute to this growing field of research targeting the interconnectedness of the musculoskeletal system and how it may inform future clinical practice.
In the traditional standard shoulder rotation PROM supine testing position, significantly more passive ER in the dominant throwing shoulder compared to the non-dominant shoulder is expected, which is what was observed in this study. By rotating the pelvis in the opposite direction from the dominant throwing shoulder (FAST-SHDR), the soft tissue slack through the musculoskeletal system is taken up and system tension is created. During the FAST-SHDR ER test the mean difference in passive shoulder ER was 50.7 less compared to the non-dominant shoulder. This large of a difference in ER rotation finding may have consequences on performance or possible injury risk of the throwing shoulder of baseball athletes.
The within subject changes (sport specific vs standard testing) were normally distributed, suggesting that in some athletes, shoulder PROM was minimally affected by test position. Biomechanical properties of soft tissues such as stiffness,28 elasticity and fascial tension can vary across subjects. It may be that the athletes whose shoulder PROM did not change across test position have lower levels of stiffness or elasticity in the tissues beyond the shoulder complex, somewhere else in the kinetic linkage. This may be another variable to consider within their throwing mechanics and could potentially contribute to overworking the local soft tissue of the shoulder complex. For example, a baseball player who has less elastic stiffness in their interconnected musculoskeletal system, may compensate through active muscle force to generate the same throwing velocity; a compensation that is less efficient and more metabolically challenging.29 The differences in IR PROM recorded between baseball players and controls provides some further evidence of test validity. These between group differences were large and exceeded the MDC, with the largest differences recorded in the dominant shoulder, based on mean differences of 26°. The reduction in IR during FAST-SHDR testing also suggests there is some three-dimensional interplay between the interconnected anterior and posterior muscle chains, and that the trunk and pelvis counterrotation potentially alters the body-wide tensegrity and muscle tension at the shoulder joint.
Throwing a baseball is a three dimensional task that requires the athlete to transfer ground reaction forces across the kinetic chain, until the moment the ball leaves the hand.9 It has been reported that more than half of the kinetic energy that is transferred to the hand during throwing is maximized from the muscles of the core and lower extremities.30 As the kinetic energy moves through the kinetic chain, the thoracolumbar fascia transfers forces from the gluteus maximus to the latissimus dorsi.26 Currently, the posterior chain mechanism is not a consideration in the standard testing model for shoulder rotational PROM. Much of this clinical measurement of shoulder rotation is traditionally assessed at 90° of humeral abduction,6 where the end range is dictated primarily by local (glenohumeral) ligament and capsular restraints, thus, three-dimensional torsion is not captured in the traditional assessment techniques. Since throwing involves movement excursions at the trunk, pelvis and shoulder, over multiple planes, the new testing position was developed to capture how global musculoskeletal tension affects shoulder PROM. The current findings also support earlier research reports where a sport specific ROM assessment was developed for the hip joint in an effort to more accurately reflect assessment measures that replicate task specific sporting movements (throwing and kicking).14
Limitations
The novel sport specific test procedure aims to recreate the tension arc position during the later phases of the overhead throw, and incorporate multiple kinetic links across the shoulder, torso, pelvis, and hip region. The authors acknowledge that the test position does not exactly replicate the mechanics of throwing, and it possibly captures a more task specific position related to external rotation, and that internal rotation maybe better suited with another novel test in the future. The FAST-SHDR test does acknowledge the value of the previous sport specific testing at the hip, which has provided useful clinical research. The test is also passive in nature and it may be that larger ranges of motion are achieved during an active and dynamic maximal throw, as tissue biomechanics are influenced by loading forces.9 Adopting a standing test position may be more specific, but it will be more difficult to stabilize the trunk during tests, and test reliability is likely to be reduced. Good to excellent intra-rater reliability was reported based on the collected data. Although two investigators were used in this study, the second assessor was only needed to hold the inclinometer since this device did not have a feature to “lock in the degree of inclination” before removing it from the subject. Had an inclinometer with this feature been used, the test could be performed by a single assessor, and reliability testing could be investigated with one assessor only in future studies. Further confirmatory research is required, and the findings cannot be extended to inter-observer agreement. There would be value in future testing to examine the FAST-SHDR for inter-rater reliability data. The test does have a level of subjectivity, particularly when passive horizontal abduction is performed, which was limited as much as possible with stabilizing straps at the lower extremities. This subjectivity and “end-feel” was also acknowledged in the hip specific functional assessment by Tak and Langhout,14 and there is potential to limit the subjectivity of the measure by using pressure sensitive technology. Integrating more technology into the assessment would potentially allow the examiners to exert the same amount of force on each subject during the testing procedure.
There was not an a priori sample size calculation. The data reported in Table 2 can inform future sample size estimations. The results of the current study suggest that the true ICC for the new test is likely to be high e.g. around 0.95; if we set a minimal ICC value (null) of 0.90 (which equates to the lowest CI margin reported in Table 2), then n=62 participants is recommended in future studies (assuming two testing points, a significance level of .05 and power of 80%).31 Of note, the sample size for the current study was 31 which is still above average for reliability studies in the sports science field.31
CONCLUSION
A new sport specific assessment has been developed to quantify passive shoulder rotation ROM (FAST-SHDR) in the baseball population. The test is reliable and has been designed to reflect the global torsional soft tissue connectivity of throwing biomechanics when compared to the traditional supine standard method of measuring passive shoulder rotation. Traditional measures of shoulder PROM (taken from 90º of abduction) were consistently higher than those achieved with the new sport specific test. The magnitude of these differences were large (eg. 50° of difference for passive shoulder ER) and should be of relevance to clinicians working with these populations. The new test also consistently differentiated between athletes and controls, suggesting initial evidence of its discriminant validity. The lower scores, which were consistently observed with the FAST-SHDR, support the hypothesis that adopting a sport-specific position engages relevant musculotendinous and fascial structures across the torso and pelvic region, influencing the available shoulder range of motion (ROM). Future research is needed to establish inter-rater reliability and to observe how these passive ROM limitations may affect performance and injury risk in baseball players.
Disclosure statement
The authors have no disclosures.