Introduction
Subacromial impingement syndrome (SIS), also called external impingement, is the most common diagnostic label for shoulder pain.1 Neer defined SIS as a mechanical compression or abrasion of the supraspinatus tendon, subacromial bursa or long head of the biceps tendon beneath the anterior undersurface of the acromion, coracoacromial ligament or acromioclavicular joint during elevation of the arm.2 Currently, this pathoanatomic model is controversial because recent evidence suggests that it does not fully explain the mechanisms related to SIS.3,4
Biomechanical factors such as alterations in glenohumeral and scapulohumeral kinematics and impairment of the rotator cuff and scapular muscles are commonly associated with SIS.5,6 Although there is no consensus in the systematic reviews of electromyographic studies examining the scapulohumeral musculature, the most significant findings were increased upper trapezius activity with reduced serratus anterior and inferior trapezius activity, associated with a delay in the activation time of the latter two muscles.7,8 Regarding the glenohumeral musculature, the activity and coactivation of the rotator cuff muscles, especially the subscapularis with the infraspinatus or supraspinatus, was found to be reduced during the first phase of arm elevation.9
Based on the above, weakness of the scapular and glenohumeral muscles is one of the main impairments in patients with SIS.10–13 Indeed, in these patients, the greatest impairment in muscle strength has been reported in the lateral rotator muscles of the shoulder (i.e., infraspinatus and teres minor, supraspinatus),11,12 leading to imbalance in the function of the rotator cuff muscles and alterations in the glenohumeral kinematics.11 Additionally, positive correlations between shoulder muscle strength, grip strength and upper limb function have been reported in previous studies.10,13 Due to the shoulder muscle imbalance that commonly exists in patients with SIS, the entire upper limb kinetic chain is affected, negatively impacting energy transfer through the upper limb as well as grip function.10 Therefore, shoulder rehabilitation programs should focus on the prescription of exercises to improve lateral rotation and handgrip strength deficits in these patients.
Although therapeutic exercise has been described as an important component for the treatment of SIS, no specific type of exercise has been described as a reference standard for the non-surgical treatment of SIS.14,15 Currently, musculoskeletal approaches focus on strengthening the shoulder joint complex and achieving dynamic stabilization.16 A novel therapeutic approach proposes adding lumbar stability training in individual athletes through the core musculature.16,17 Despite some controversies, it has been observed that this approach has general benefits in the functional recovery of the shoulder.16–18 These benefits include an increase in electromyographic activity of the middle trapezius and serratus anterior muscles, in addition to an increases in the power of throws and strength in the punches of athletes.17,19 Based on biomechanical foundation as energy transfer through kinetic chains, the authors hypothesized that, in addition to supervised physiotherapy, the use of core-focused exercises could be an effective approach for improving lateral rotator strength in the early stages of rehabilitation in patients with SIS.
To the authors’ knowledge, there are no published studies that have analyzed the effect of adding a core exercise program to supervised physiotherapy in order to improve lateral rotator strength in patients with SIS. Thus, the aim of this study was to assess the short-term effects of adding a core exercise program to supervised physiotherapy on improve lateral rotator strength and functional outcomes in patients with SIS. The authors hypothesized that, in addition to supervised physiotherapy, core-focused exercises could be an effective approach for improving lateral rotator and grip strength in the early stages of rehabilitation in patients with SIS.
Methods
Design/setting
A single-group pre- and post-test study was performed and reported according to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.20 The study was approved by the ethics committee of the Central Metropolitan Health Service of Chile on 7 October 2019 (ID: 048975). Between February 2020 and February 2021, a total of 47 patients with SIS were prospectively recruited. All patients signed an informed consent form approved by the ethics committee.
Participants
Participants were recruited from the Physical Therapy Department of Clinical Hospital San Borja Arriaran in Santiago, Chile. To be eligible for participation, patients with SIS had to meet the following conditions: age ≥ 18 years; pain located on the anterolateral side of the shoulder for ≥ 3 months; and three or more positive clinical signs of SIS, such as the Neer or Hawkins-Kennedy test, a painful arc, pain on resisted external rotation or the Empty Can test. The sensitivity and specificity of these combined clinical signs is >74% for a diagnosis of SIS.21 Exclusion criteria were a diagnosis of cervical radiculopathy, osteoarthritis in the acromioclavicular or glenohumeral joint, calcific tendinitis, adhesive capsulitis, glenohumeral instability or a partial or full-thickness rotator cuff tear; radiographs and magnetic resonance imaging were performed to confirm the absence of these pathologies. Other exclusion criteria were athlete’s subjects or participate in a structured sport, a clinical history of acute trauma, previous surgery, previous fracture in the affected shoulder or corticosteroid injection into the shoulder joint in the prior 12 months.
Supervised physiotherapy treatment
Physiotherapy treatment consisted of a five-week, twice a week, supervised, specific exercise program based on the clinical decision algorithm proposed by a panel of experts.22 In the initial stage, ‘scapular orientation’ was trained to improve proprioception and normalize the resting position of the scapula. Then, three scapular control exercises were performed: bilateral shoulder flexion up to 60°; a closed kinetic chain exercise (the ‘unilateral bench press’); and a scapular control exercise with bilateral shoulder retraction and extension in the prone position. The final stage included two glenohumeral control exercises to restore centralization and prevent superior translation of the humeral head: isometric lateral rotation performed with shoulder adduction; and isometric adduction of the shoulder in the scapular plane at 30° and 60° of elevation. The exercises were performed without or with minimal pain (< 3 cm on the Visual Analog Scale [VAS]), and a maximum of four exercises per session. The dose and progressions were related to the goal of each exercise: 8–10 repetitions of each exercise, with a 5–10-s duration and 30s to 1 min of rest between each repetition.23 (see Supplementary Table S1).
Core exercise program
The ‘core’ is a functional term that represents the trunk musculature (back, abdominal, pelvic floor, diaphragm, hip and gluteus) and connects the upper and lower extremities.18,24 Alongside conventional physiotherapy treatment, a Level 1 core exercise program (patient in a stationary position with static contraction) was performed; following the levels of as suggested by Jeffreys et al.25 Four core exercises were performed: ‘knee push-up’, ‘isometric forearm plank’, ‘gluteal bridge’ and ‘dead bugs’. Ten repetitions of each exercise with a 10–15-s duration and 1 min of rest between each repetition were performed (see Supplementary Table S2).
Outcome measures
Two physiotherapists external to the research team performed the assessments at baseline and at the end of the five-week treatment. Both physiotherapists assessed the same number of patients.
Primary outcome measures
The primary outcome measure was isometric lateral rotator strength and grip strength assessed using a dynamometer. Lateral rotator muscle isometric strength was measured using a handheld dynamometer (Hoggan MicroFET2; Scientific LLC, Salt Lake City, UT, USA). Participants completed 5-s maximal contractions. Participants were in the standing position with their feet approximately shoulder width apart, the arm and wrist in neutral position, and the elbow at 90° flexion.10 Three measurements were performed with the dynamometer against a wall for stability and to give resistance to counter the maximal contraction.10 The affected shoulder was tested, and verbal encouragement was used to ensure maximal contractions. Additionally, a physiotherapist observed whether the participant compensated for lateral rotation with shoulder abduction; if this occurred, the attempt was discarded and the assessment was repeated. A rest time of one minute between each contraction ensured sufficient recovery. The average value obtained from the three attempts was used for analysis.
A Jamar™ dynamometer (Model FS360, Performance health; Illinois, United States) was used to assess handgrip strength in the affected side. Participants completed 5-s maximal contractions. Participants were in the standing position with their feet approximately shoulder width apart, a wall behind them to add stability, prevent trunk rotation, and help maintain arm position. Three measurements were performed with the arm and wrist in neutral position and the elbow at 90° flexion. The affected side was tested, and verbal encouragement was used to ensure maximal contractions. A rest time of one minute between each contraction ensured sufficient recovery. An adjustment of 10% between the force of the dominant and non-dominant side was made. The average value obtained from the three attempts was used for analysis.
Secondary outcome measures
The main secondary outcome measure was muscular endurance, assessed using the Closed Kinetic Chain Upper Extremity Stability Test (CKCUEST).26 Participants assume a push-up position, with the spine and lower limbs aligned and feet separated shoulder-width apart. During the 15 s of testing, participants moved one hand to touch the dorsum of the opposite hand and then returned the moving hand back to the starting position. Subsequently, participants performed the same movement with the other hand. If one of the touches did not reach the required distance of the test, the testing continued but the attempt was not counted.26 The CKCUEST is considered easy for clinicians to apply, and also easy for patients to understand.26 Additionally, shoulder function was assessed with the Constant-Murley questionnaire.27 Scores range from 0 to 100 points, with lower scores indicating a worse condition.27 Finally, pain intensity during isometric strength testing of the lateral rotator muscles was assessed with the VAS. This is a valid scale, with scores ranging from 0 to 10 cm and higher scores indicating greater pain intensity.28
Statistical analysis
Descriptive statistics were used to describe the demographic and clinical characteristics of the patients. For continuous outcomes, data are presented as the mean and standard deviation (SD); for categorical outcomes, data are presented as the number and percentage (%). The normality distribution was evaluated using both statistical (Shapiro-Wilk test) and graphical (normal probability Q–Q plot) methods. To assess the differences between baseline and post-treatment, the paired t-test or Wilcoxon test was used. Additionally, the Cohen’s d (d) was reported to provide the effect size of adding the core exercise program to the supervised physiotherapy treatment, considering the effect as trivial (< 0.2), small (0.2–0.5), medium (0.5–0.8) or large (> 0.8).29 The significance level was set at p < 0.05 and the confidence interval (CI) at 95%. Data were analyzed using the Statistical Package for the Social Sciences (SPSS), Version 27 (SPSS Inc., Chicago, IL, USA).
Results
Thirty-four subjects with SIS were included in the study (43.9 +/-5.4 years; 34 male and 17 female). All baseline characteristics for the patients are presented in Table 1.At the end of the five week intervention period, there were no complications associated with the treatment received and no dropouts or withdrawals.
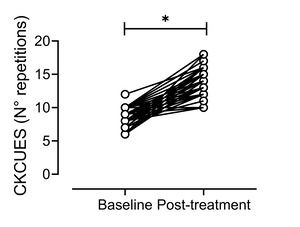
Table 2 shows the baseline, post-treatment and a comparison of results for all the functional outcomes. At the end of the five weeks, the isometric lateral rotator strength showed an increase of 9.2 kg (95% CI = 7.9–10.4; Cohen’s d = 2.1; p < 0.001) and grip strength showed an increase of 10.6 kg (95% CI = 9.3–11.9; Cohen’s d = 2.4; p < 0.001). For secondary outcomes, the CKCUEST showed an increase of 5.6 repetitions (95% CI = 5.1–6; Cohen’s d = 3.7; p < 0.001), the Constant-Murley questionnaire showed an increase of 30.3 points (95% CI = 28.5–32.1; Cohen’s d = 4.9; p < 0.001) and the VAS showed a decrease of 3.9 cm (95% CI = −3.7 to −4.1; Cohen’s d = 6; p < 0.001) (Figures 1-5). For all the outcomes assessed, the effect sizes were large (> 0.8) and the differences were statistically significant (p < 0.05).
Discussion
Weakness of the rotator cuff musculature has been reported in patients with SIS. A novel therapeutic approach adding exercises of core musculature for functional recovery in these patients was examined. The main findings were that this exercise program showed statistically and clinically significant differences for improving the isometric strength of shoulder lateral rotator muscles, grip strength, muscular endurance
While shoulder strength has been studied extensively in the rehabilitation, reintegration, and sports training of throwers and healthy population, there is a notable lack of research focusing on the recovery of lateral rotator muscle strength in adult non-athletes with SIS.18,30 This study is the first to report improvement in the isometric strength of the lateral rotator muscles and grip strength in the early stages of rehabilitation with a supervised physiotherapy treatment that included a core exercises program. Based on biomechanical foundations, all upper limb tasks are performed through the integration of multiple body segments and sequential activation of different muscle groups.31 In this sense, the greater proportion of kinetic energy and force in this sequencing is derived from the larger proximal body segments.31,32 For instance, 51% of the total kinetic energy and 54% of the total force generated in a tennis service are generated by the lower legs, hip and trunk.32
Supporting this notion, dysfunction within a motion sequence from the pelvis to the shoulder girdle may cause an alteration in energy transfer through kinetic chains, resulting in significantly greater shoulder distraction forces.33 On the other hand, previous studies have shown that the muscles of the anterolateral and posterolateral kinetic chain present greater myoelectric activation during the execution of core exercises.18,25 Thus, the increase in grip and shoulder lateral rotation strength observed in the current study could be a result of improvement in energy transfer from the trunk, shoulder complex and remaining links of the kinetic chain of the upper limb.17,19 Furthermore, participants with SIS showed an improvement in the CKCUEST performance, which may also be related to optimization of energy transfer along the links of the closed kinetic chain that occur in a plank position and because the xercise program is performed in this position.34 Therefore, the use of core-focused exercises seems to be an effective and safe approach, without the prescription of the dynamic exercises specifically targeting to lateral rotator cuff muscles, for improving shoulder muscle strength in patients with SIS in early stages of treatment.
Usually, core-strengthening exercises are recommended to improve muscle activity in athletes with musculoskeletal injuries.18,24 However, this recommendation lacks strong evidential support when the treatment is applied to non-athletes with SIS.16,17 In accordance with the current findings, some studies on throwing athletes and healthy non-athletes showed improvement of isometric rotator cuff strength.16,19,30 Indeed, it has been reported that isometric core exercises involving the upper limb can improve shoulder strength, while dynamic exercises improve the throwing speed.13,35 In addition, other studies showed that lumbopelvic stabilization exercises improve the activity of the shoulder muscles.16,30 However, additional studies are needed to analyze the effects of these exercises in the rehabilitation of non-athletes with shoulder injuries.
The current findings could be explained from different viewpoints. Some authors have shown a relationship between the scapular and shoulder muscles and the central stabilizer muscles of the spine during movement of the upper limbs.35,36 A proposed mechanism to explain this association is that core stabilization provides stability and support for load transfer to the limbs, suggesting that core muscles provide proximal stability for distal mobility.37 Despite this, there is still a lack of high-quality evidence showing the direct effects of central stabilization exercises on the strength of rotator cuff muscles. Supporting the current findings, some authors have reported a positive correlation between grip strength and rotator cuff muscle activity.10,12,38 One study found that a neutral grip task increased the electromyographic activity in supraspinatus and infraspinatus muscles.38 Another study showed that patients with SIS who participated in handgrip exercises had reduced pain intensity and improved shoulder function.12 Finally, a strong correlation has been demonstrated between handgrip strength and lateral rotator strength in healthy populations.10 These findings could be explained by neural inputs in the corticospinal pathways during handgrip strength exercises.12 This mechanism is mediated by a neural network in the cortical and subcortical areas of the brain that increases the motor variability of the rotator cuff muscles when performing a handgrip exercise.12,39,40
Limitations
The safety and clinical applicability of the core exercise program in conjunction with supervised physiotherapy treatment are the main strengths of this study. However, this study has several limitations as it is a pre–post single-group study without a control group, the clinical effectiveness of the core exercise program cannot be established in these patients. The lack of control of confounding factors inherent in observational studies may have caused overestimation of the treatment effects, although the effect sizes indicate strong effects of the intervention. Changes in the glenohumeral or scapular kinematics were not assessed so any kinematic reasons for improvements cannot be assumed. Self-reported questionnaires were used for assessment, which are prone to subjectivity and recall bias, which may have affected CM outcomes. Finally, the method used to assess lateral rotator strength is one of the most recommended for clinical use but is not the ‘gold standard’. These limitations should be considered when attempting to extrapolate the findings of this study to all patients with SIS.
Despite the limitations, the results of this study provide an important clinical implication for the physiotherapy treatment of patients with SIS. Although physiotherapy is considered a first-line treatment for SIS, the effectiveness of therapeutic interventions to improve lateral rotator strength in the early stages of rehabilitation is unclear. Therefore, this study’s results could guide physiotherapists to consider these exercises in patients with SIS. Further studies are needed to determine the specific stabilization exercises that are most effective in this clinical population.
Conclusion
In the short term, adding a core exercise program to supervised physiotherapy showed statistically and clinically significant differences improvements in isometric lateral rotator and grip strength, as well as improvements in functional outcomes in patients with SIS. However, these findings must be interpreted in the context of the studied population and further high-quality research is needed to further explore this approach.
Conflicts of interest
The authors report no conflicts of interest.
_strength.tiff)



_strength.tiff)



