Introduction
Musculoskeletal ultrasound (MSKUS) has become an essential tool for diagnosing and managing a wide range of musculoskeletal conditions. The Achilles tendon, which connects the gastrocnemius and soleus muscles to the calcaneus, is a critical structure that facilitates walking, running, and jumping. Given its high mechanical load, the tendon is vulnerable to acute injuries and chronic degenerative conditions, particularly in physically active individuals.1,2
MSKUS provides high-resolution, real-time imaging of the Achilles tendon, allowing for the evaluation of its structural integrity and viewing the surrounding tissues.3,4 Unlike MRI, MSKUS is dynamic, enabling functional assessment during movement, while being more accessible and cost-effective. This paper reviews the sonographic anatomy of the Achilles tendon, the appearance of common pathologies, and the role of MSKUS in clinical evaluation and rehabilitation.
Anatomy of the Achilles Tendon
The Achilles tendon, or tendo calcaneus, is the confluence of the gastrocnemius and soleus muscles, inserting onto the posterior aspect of the calcaneus. It spans approximately 15 cm and tapers distally, with its musculotendinous junction varying in height among individuals. The tendon is enveloped by a vascularized paratenon, which aids in reducing friction during movement.
On ultrasound, the normal Achilles tendon in the long axis (LAX) view demonstrates a fibrillar echotexture with parallel hyperechoic lines. In the short axis (SAX) view, the tendon exhibits a reniform (kidney-shaped) contour and a homogenous hyperechoic appearance. The paratenon appears as a thin, hypoechoic layer, and Kager’s fat pad, situated deep to the tendon, serves as a hypoechoic reference landmark. Krager’s fat pad is the triangular region made up of the Achilles tendon, the flexor hallucis tendon, and a wedge of fat adjacent to the calcaneus.
Common Pathologies of the Achilles Tendon
Achilles Tendinopathy
Achilles tendinopathy is a degenerative condition characterized by tendon thickening, hypoechoic areas, and disrupted fibrillar architecture on ultrasound.5–7 Doppler imaging often reveals neovascularization in chronic cases, particularly in the mid-portion of the tendon.8,9 Symptomatic tendons frequently measure >7 mm in thickness, compared to the normal range of 4–6 mm.10
Partial and Full-Thickness Tears
Tears typically occur in the hypovascular “watershed area” 2–6 cm proximal to the calcaneal insertion.4,8,11 Partial tears appear as focal hypoechoic defects with preserved tendon continuity, while full-thickness tears demonstrate complete fiber disruption, visible as a hypoechoic or anechoic gap. Retraction of tendon ends is commonly observed in complete ruptures. The Kuwada classification system grades tears based on severity, ranging from partial (Grade I) to complete ruptures with a gap >6 cm (Grade IV).
Insertional Tendinopathy
Insertional tendinopathy affects the distal 2 cm of the tendon. Sonographic findings include hypoechoic and thickened tendon fibers, calcifications or enthesophytes at the calcaneal insertion, and fluid-filled retrocalcaneal bursitis.8,12 Chronic cases may also show hypervascularity on Doppler imaging. It is important to note that the tendon should be kept in a relaxed state when using Doppler as tension may obliterate any new vessels.13
This bony prominence at the posterosuperior calcaneus causes mechanical irritation of the Achilles tendon. Ultrasound reveals a prominent osseous contour, thickened tendon fibers, and retrocalcaneal bursitis with fluid accumulation.
Tendinosis
Tendinosis reflects chronic degenerative changes without inflammation, appearing as hypoechoic regions with tendon thickening and disorganized fibrillar architecture.2,9 Chronic tendinosis may also exhibit calcifications or fatty degeneration.
Retrocalcaneal Bursitis
Retrocalcaneal bursitis is associated with overuse and manifests as anechoic or hypoechoic fluid distension of the bursa anterior to the Achilles tendon. This entity can co-exist with tendinopathy or inflammatory conditions.14 Chronic inflammation may cause synovial hypertrophy and calcifications.4,8
Advantages of MSK Ultrasound for Achilles Tendon Evaluation
There are several advantages in using MSK-US to evaluate the Achilles Tendon in patients with posterior ankle pain.
-
Dynamic Imaging: Allows visualization of the Achilles during active movement, aiding in the diagnosis of Achilles tendon abnormalities.3
-
Real-Time Guidance: Facilitates guided interventions such as injections or dry needling.12
-
Soft-Tissue Differentiation: Provides high-resolution imaging of tendons, muscles, and bursae.4,8
-
Cost-Effectiveness and Accessibility: Offers a less expensive and more readily available alternative to MRI.1,12
Diagnostic MDK Ultrasound Techniques for the Achilles Tendon
Proper imaging technique is vital for accurate diagnosis. The patient is positioned prone, with the foot hanging freely or supported by a bolster, allowing dynamic assessment. A high-frequency (10–15 MHz) linear transducer is used.
The scanning protocol for the Achilles tendon includes 2 planes of transducer placement.
-
Transverse Plane: The transducer is placed perpendicular to the Achilles to identify tendon abnormalities including thickening, partial tears or ruptures.
-
Longitudinal Plane: The transducer is aligned along the muscle fibers to assess the muscle and tendon continuity.
Dynamic maneuvers, such as passive dorsiflexion and plantarflexion, or gentle squeezing (Thompson test) assess tendon glide and continuity. Adjacent structures, including the retrocalcaneal bursa and Kager’s fat pad, are evaluated for associated pathology. During movements of plantar flexion, Krager’s fat pad extends into the retrocalcaneal bursa as far as the enthesis. While in neutral, Kager’s fat pad is retracted so that the tendon is against the bone, the superior tuberosity of the calcaneus.15 Common artifacts, such as anisotropy, are mitigated by adjusting the transducer angle.3,8
Clinical Applications
Guided Interventions
MSKUS enhances precision in dry needling, corticosteroid injections, and platelet-rich plasma (PRP) therapy by confirming the target site and avoiding inadvertent tendon injury.3,12
Monitoring Healing
Serial imaging tracks resolution of hypoechoic areas, restoration of fibrillar structure, and reduction of hypervascularity, guiding progression in rehabilitation.6
Optimizing Rehabilitation
Sonographic findings guide individualized treatment plans, such as eccentric loading exercises for tendinopathy or range-of-motion protocols for post-rupture recovery.1,2,7,16
Conclusion
MSKUS is an invaluable tool for diagnosing and managing Achilles tendon pathologies. Its dynamic capabilities, cost-effectiveness, and high-resolution imaging make it superior for assessing soft tissue conditions. By enabling accurate diagnosis and real-time intervention guidance, MSKUS enhances clinical outcomes and facilitates effective rehabilitation.1,2,7,16 Continued research and protocol standardization will further integrate MSKUS into routine musculoskeletal care.
Achilles Tendon
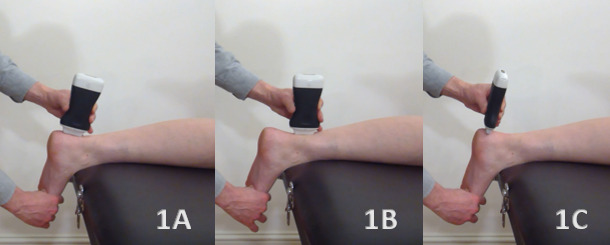
Patient Positioning
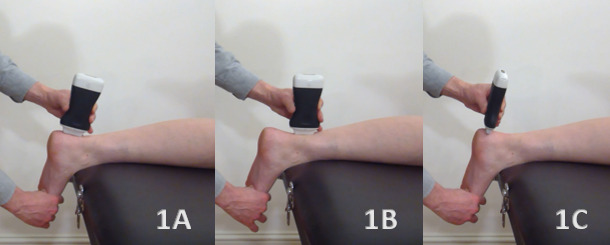
The patient should be positioned prone on the examination table, with the foot resting on a bolster or hanging over the edge of the table (shown in Figure 1A). This positioning facilitates dynamic assessment of the Achilles tendon by allowing it to be plantar flexed and dorsiflexed during the examination. Alternatively, the patient may be placed in a kneeling position in a stable armchair, providing support and allowing the transducer to be applied to the posterior aspect of the Achilles tendon. The examination typically begins with the foot in a dorsiflexed position to create tension across the Achilles tendon.
Figure 1A: Transducer Placement on Achilles Insertion in Long Axis View (LAX)
For the long axis view, the transducer is placed in a longitudinal (LAX) orientation, with the reference end positioned proximally on the Achilles tendon, directly over the calcaneal tuberosity at the Achilles insertion. The transducer should be angled slightly from posteromedial to anterolateral. A heel-to-toe rocking motion allows the examiner to scan the entire Achilles tendon at its insertion on the calcaneus, ensuring the tendon remains hyperechoic throughout the assessment.
Figure 1B: Transducer Placement on Achilles Tendon Mid-Portion in Long Axis View (LAX)
To visualize the entire Achilles tendon, maintain the transducer in the longitudinal (LAX) orientation and slide it proximally from the distal insertion toward the mid-portion of the tendon. Continue this approach up to the posterior knee to examine the gastrocnemius and soleus musculature. Scanning the tendon from medial to lateral enables a comprehensive evaluation of the tendon and associated musculature.
Figure 1C: Transducer Placement on Achilles Insertion in Short Axis View (SAX)
For the short axis view, position the transducer in a transverse (SAX) plane over the calcaneal tuberosity at the Achilles insertion. The transducer should be angled slightly from posteromedial to anterolateral. Using a heel-to-toe rocking motion, the examiner can scan the entire Achilles tendon at its insertion on the calcaneus, ensuring a hyperechoic appearance. To achieve a more thorough examination, slide the transducer proximally from the distal insertion toward the more proximal tissues.
.png)
NORMAL ACHILLES TENDON INSERTION IN LONG AXIS (LAX)
Figures 2A and 2B: LAX View
The objective of this image is to capture the tapering, arrow-like contour of the Achilles insertion onto the calcaneus. Refer to Figure 1A for the transducer position for this image. The retro-calcaneal bursa, visible as mixed echoes, separates the tendon from the calcaneus. The Kager’s fat pad, a triangular region located deep to the Achilles tendon and proximal to the calcaneus, appears as mixed echoes typical of fat on ultrasound. Abnormalities in the fat pad, often seen as ossification, are commonly associated with Achilles injuries. The Achilles insertion may appear hypoechoic due to anisotropy, which should not be mistaken for pathology. To ensure accurate visualization of all tendon fibers, employ a heel-to-toe toggling motion with the transducer to maintain a perpendicular orientation to the tendon as it curves at the insertion. Normative value for the Achilles tendon thickness is 4.94 + 1.24 mm.17
.png)
NORMAL ACHILLES TENDON MID-PORTION IN LONG AXIS (LAX)
Figures 3A and 3B: LAX View
When scanning proximally from the calcaneal insertion in a long axis (LAX) orientation, position the transducer approximately 5-7 cm (2-3 inches) from the insertion point. Refer to Figure 1B for the transducer position for this image. Dynamic evaluation of the Achilles integrity can be facilitated by plantarflexion and dorsiflexion of the foot. The height of the musculotendinous junction between the soleus muscle and the Achilles tendon varies among individuals, and in some cases, the plantaris tendon may also be visualized. As the transducer is moved proximally, no distinct bony landmarks will be encountered. The objective is to capture the bright, hyperechoic, intact fibrillar pattern of the most superficial fibers of the Achilles tendon.
.png)
NORMAL ACHILLES TENDON INSERTION IN SHORT AXIS (SAX)
Figures 4A and 4B: SAX View
Position the transducer slightly proximal to the true tendon insertion at the calcaneus to visualize the Achilles tendon in a transverse cross-sectional plane as it approaches the calcaneal insertion. Refer to Figure 1C for the transducer position for this image. This image does not include a bony reference point, and the objective is to capture the dense, “bristle-like” pattern characteristic of the Achilles tendon. In a normal short axis (SAX) view, the tendon exhibits a reniform or kidney-shaped contour. However, with advancing tendinosis and increased intra-tendinous pressure, the Achilles tendon often takes on a round or ball-like shape. The Achilles insertion may appear hypoechoic due to anisotropy, which should not be mistaken for pathology. Kager’s fat pad (KFP), situated deep to the Achilles tendon, should also be noted. Normative value for the Achilles tendon thickness in the SAX view are 14.43 + 4.07.16
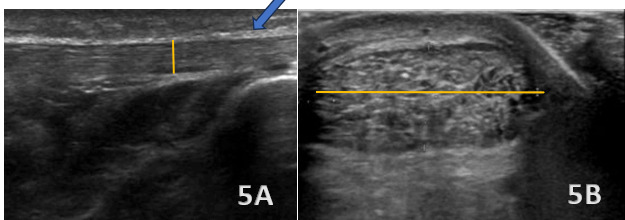
ACHILLES TENDINOPATHY
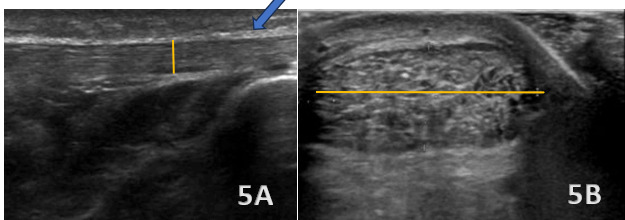
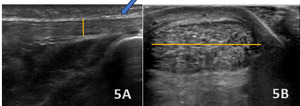
Figures 5A (LAX View) and 5B (SAX View)
In the LAX view, the Achilles tendon is significantly thickened (highlighted with blue arrow in figure 5A), measuring 10 mm in thickness (highlighted in figure 5A with yellow line) and 24 mm in width (highlighted in figure 5B with yellow line), with hypoechoic areas distributed throughout, indicating degenerative changes. This contrasts with the normal mean values for the Achilles tendon, which are typically 4.94 ± 1.24 mm. The SAX view shows an enlarged cross-sectional area with a rounded or irregular contour, heterogeneous echotexture, and hypoechoic regions, further highlighting the tendinopathic changes.
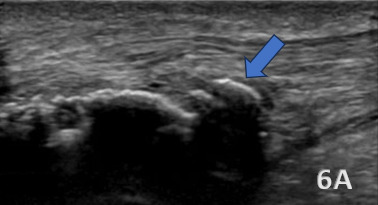
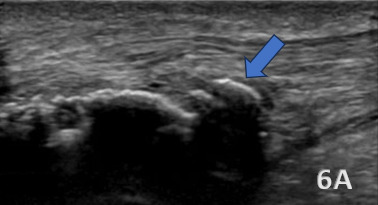
HAGLUND’S DEFORMITY
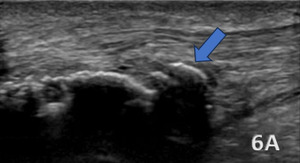
Figure 6A (LAX View):
A Haglund’s deformity is shown as cortical irregularities and a bony prominence on the posterior aspect of the calcaneus near the Achilles tendon insertion. The overlying soft tissues, including the retrocalcaneal bursa can show signs of inflammation, appearing hypoechoic or swollen. The Achilles tendon itself demonstrates thickening and increased echogenicity at its insertion due to chronic irritation. Additionally, there may be evidence of bursitis, with fluid accumulation seen as an anechoic or hypoechoic area within the retrocalcaneal bursa.
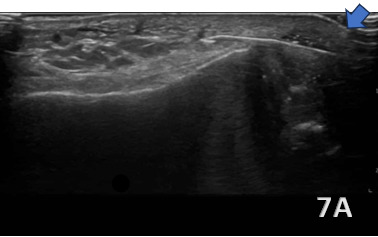
ACHILLES INSERTIONAL TENDINOPATHY
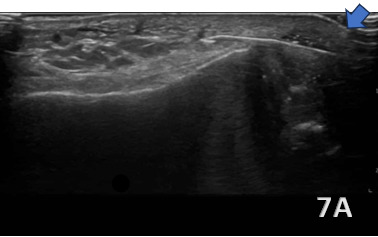
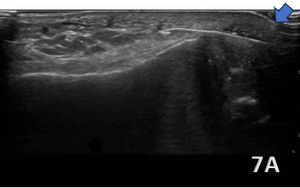
Figure 7A (LAX View):
Insertional Achilles tendinopathy (blue arrow highlighting) is characterized by pathological changes in the distal 2 cm of the Achilles tendon at its attachment to the calcaneus. On diagnostic ultrasound, hallmark findings include tendon thickening and hypoechoic areas indicative of collagen degeneration and disorganization. Calcifications or enthesophytes at the insertion site are common and appear as hyperechoic foci with posterior acoustic shadowing. Associated retrocalcaneal bursitis may be visualized as an anechoic or hypoechoic fluid collection between the anterior Achilles tendon and the calcaneus, with possible synovial hypertrophy in chronic cases. Power Doppler imaging may reveal hypervascularity at the tendon insertion, reflecting a chronic inflammatory response.
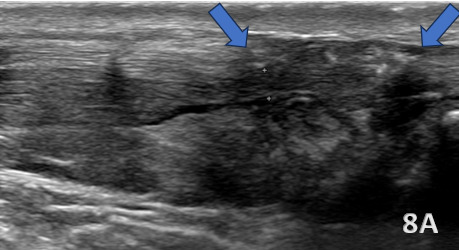
ACHILLES TENDON TEAR
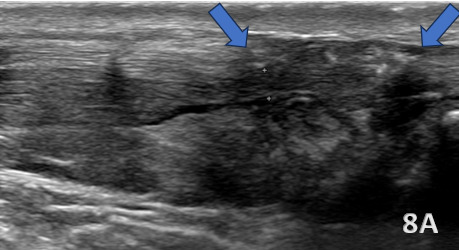
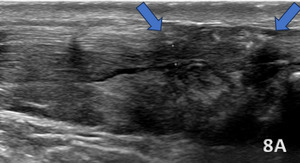
Figure 8A (LAX View):
Achilles tendon tears most commonly occur 2–6 cm proximal to the calcaneal insertion, a region of reduced vascularity. On diagnostic ultrasound, full-thickness tears (highlighted with the blue arrows) appear as discontinuities in tendon fibers with a hypoechoic or anechoic gap, while partial tears (<50% disruption) demonstrate focal hypoechoic areas with some intact fibers. Fluid and debris are often visible in Kager’s fat pad, accompanied by mild hyperemia on Doppler imaging. Bone fragments may be present near the insertion in cases of avulsion injuries, and portions of the tendon may remain intact even with significant disruption. The Kuwada classification system categorizes tears: Grade I (partial rupture, <50%), Grade II (complete rupture, gap <3 cm), Grade III (gap 3–6 cm), and Grade IV (gap >6 cm). Dynamic imaging during dorsiflexion and plantarflexion confirms tendon discontinuity and retraction, guiding diagnosis and management.
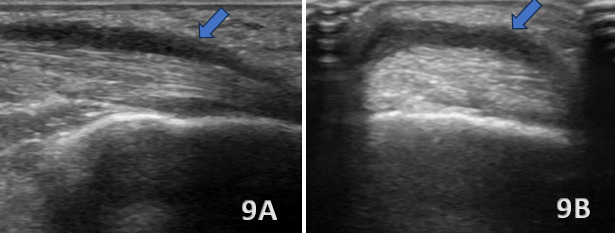
ACHILLES PERITENDONITIS
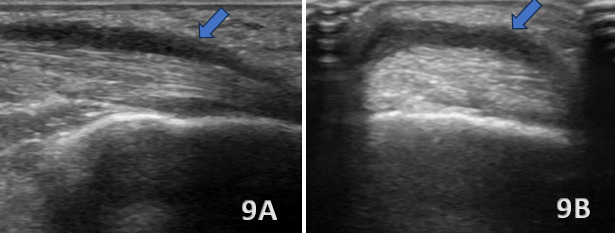
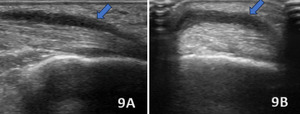
Figures 8A (LAX View) and 8B (SAX View):
Ultrasound findings of Achilles peritendonitis include a hypoechoic crescent (blue arrows) abutting the posterior surface of the distal Achilles tendon, with increased vascularity on Doppler imaging in the peritendinous region and Kager’s fat pad, without increased echogenicity. The Achilles tendon itself appears intact, with no signs of tendinosis. These findings differentiate peritendonitis, which affects the tissues surrounding the tendon, from tendonitis, which involves intrinsic changes within the tendon structure.

.png)
.png)
.png)
.png)
.png)
.png)