INTRODUCTION
Sports chiropractors are increasingly being consulted in the assessment, treatment, management and rehabilitation of amateur and professional athletes.1 Case reports and series can be invaluable types of research to document the clinical practices and outcomes of treatments of a profession.2
The throwing action of the javelin can be divided into four broad phases i) the approach/run up, ii) the delivery stride, iii) the delivery and iv) the recovery phase3–5 (Figure 1). The distance of the throw is directly related to the release speed, with 70% of the release speed created during the last 0.1 second of the throwing action in the delivery phase, which puts significant stress on the medial elbow and may predispose this area to injuries.4–6
Appropriate diagnosis and management of medial elbow injuries requires not only a thorough knowledge of the osseous, ligamentous, nervous, and musculotendinous structures but additionally a working understanding of the biomechanical aspects of the throwing action.7 The throwing action of javelin places significant stress on the elbow joint and may make this area susceptible to injuries.3,4,8 Medial elbow issues are not exclusive to the sport of javelin, but also seen in baseball, American football, volleyball, water polo, badminton, squash and tennis which require similar overhead actions.9,10
The biomechanics of the elbow joint can be divided into kinematics, force transmission and stabilization (passive and active).11 The stability of the elbow joint is due to a combination of both passive and active mechanics.12–14 Primary passive soft tissue stabilizers of the elbow joint resisting varus stress is from the lateral collateral ligament (LCL) and valgus stress from the medial collateral ligament (MCL).13,15 The medial ulnar collateral ligament (MUCL) or MCL is also referred to as ulnar collateral ligament (UCL); however, throughout this case report the term UCL will be used.16 The UCL is comprised of three bundles (anterior, posterior and transverse) that provide primary restraint to valgus stress.15 The anterior bundle is the most commonly injured structure of the UCL.17,18 The anterior bundle can then be further divided into the anterior and posterior bands, providing valgus restraint in overhead throwing actions from 30°-90⁰ (anterior), 90⁰-120° (posterior) and coprimary restraint between 60⁰-90⁰ of elbow flexion in motion.19
Active stabilization of the elbow joint occurs through four broad muscle groups that traverse the elbow joint; the wrist flexors, wrist extensors, elbow flexors, and elbow extensors and provide joint compressive forces and force transmission during functional movement.13,14,20 The flexor pronator group (Flexor carpi ulnaris [FCU], Flexor digitorum superficialis [FDS], Pronator teres [PT] and Brachioradialis) act as the primary active stabilizers of the elbow joint.21,22 The FCU is the predominant musculotendinous structure overlaying the UCL and primary dynamic stabilizer of the elbow at 120° of elbow flexion.23
Multiple medial elbow injuries are cited in literature amongst javelin athletes including medial epicondylitis/osis commonly termed golfers’ elbow), ulnar neuritis, UCL injury, osteochondritis dissecans (OCD), flexor-pronator muscle group injury, medial epicondyle apophysitis or avulsion, valgus extension overload syndrome (VEOS) (also known as posteromedial impingement syndrome or pitchers elbow), stress fractures, tendinopathies, and impingement injuries.8,24–30 The most common injuries seen in literature and within this case series will be expanded on in the discussion section.
A range of different treatment options for medial elbow injuries have been described in the literature, depending on the etiology and diagnosis. Common nonoperative treatment options for medial elbow injuries include stretching, rest, activity modification, and physical therapies.31,32 Additional treatment interventions include extracorporeal shockwave therapy (ESWT), platelet-rich plasma injections (PRP), prolotherapy, low level laser therapy (LLLT)/photobiomodulation (PBM), and ultrasound-guided percutaneous tenotomy.32–35 Surgical treatment options vary based on the diagnosis and pathophysiology; the most common of which is the “Tommy John surgery”, an ulnar collateral ligament reconstruction with a free tendon graft,36 discussion of this is outside the scope of this paper. There is limited research that describes chiropractic treatment and management of medial elbow injuries in javelin athletes. This case series aims to contribute to bridge the knowledge gap in this field, by presenting successful return to performance cases using conservative management approaches.
This case series presents the assessment, diagnostic work up and treatment protocols of both male and female javelin athletes at both amateur and elite levels. The purpose of this case series was to describe a multimodal chiropractic treatment approach to address medial elbow injuries in amateur/elite javelin throwers.
CASE DESCRIPTIONS
The athletes in this case series have competed at both national and international competitions which include world championships, Commonwealth and Olympic games. Their ages ranged between 15- 25 years and their years of training/competition ranged between 3-10 years. Both acute and chronic presentation of medial elbow injuries are discussed among these five athletes in this case series. Written informed consent was obtained from the subjects prior to publication. Written informed consent was obtained for the use of images prior to publication.
The cases in this series were managed by two practitioners. Practitioner one is a Titled Sports and Exercise Chiropractor, strength and conditioning practitioner and certified athletics coach with 17 years of clinical experience. Practitioner two is a Fellow of Sports and Exercise Chiropractic with 35 years as a clinician. The included athlete’s clinical and demographic information can be found in Table 1 and physical examination findings in table 2. All participants gave informed consent to participate in this research.
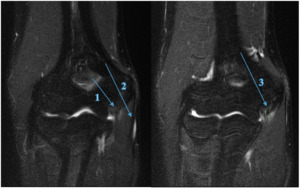
Athlete A
A 21-year-old elite male Javelin thrower (Australian representative) presented with right sided medial elbow pain, rating up to 8/10 (NRS), with a history of right medial elbow issues including medial epicondylitis and FCU tendinosis. The physical examination findings were primarily palpatory tenderness at the UCL over the joint line (oblique ligament location) and at the sublime tubercle attachment, positive orthopaedic tests for the shoulder and elbow, with changes in the elbow extension (160°), shoulder flexion (150°) and abduction (160°) and internal rotation (IR) (55°) (Table 2). The athlete only experienced pain in posterior medial elbow when throwing at high intensity or when in full elbow flexion during the catch phase of an Olympic clean exercise. Because the athlete was unable to compete at an elite level seven weeks post symptom onset, he was referred for a magnetic resonance imaging (MRI) scan of the right elbow, which revealed a high grade UCL tear with a small associated avulsion fracture with no ligament displacement (Figure 2). Subsequent consultation with an elbow orthopaedic specialist recommended surgery on the ligament however athlete, coach and chiropractor all agreed to attempt conservative therapy.
Athlete B
A 24-year-old elite female Javelin thrower (Australian representative) presented with a three-month gradual onset of sharp pinching pain at the right posteromedial elbow, six months prior to the 2020 Tokyo Olympic Games. She had a previous history of shoulder and elbow injuries intermittently throughout her throwing career, with a diagnosis of medial epicondylitis eight months prior to this presentation.
This presentation of medial elbow dysfunction was exacerbated by any throwing motion and had pain that she rated as a 4/10 - 8/10 (NRS), at worst when throwing. On postural examination, the elbow was flexed at 26° and on passive elbow extension 165° was observed. Additional physical examination findings are presented in Table 2. Based on the history, mechanism of injury, clinical findings and personal circumstances, the athlete was not referred for imaging.
Athlete C
An 18-year-old elite female Javelin thrower (Australian representative) complained of a constant dull ache at the medial elbow and GH joint. She described pain to the medial elbow as sharp and pinpoint immediately after throwing and a dull ache over her medial elbow occurred post training sessions. Athlete C reported 6/10 on the NRS with throwing, reducing to 2-3/10 post training for a few hours which developed to joint stiffness. Specific physical examination findings and associated symptoms to the elbow, shoulder and thoracic spine can be found in Table 2.
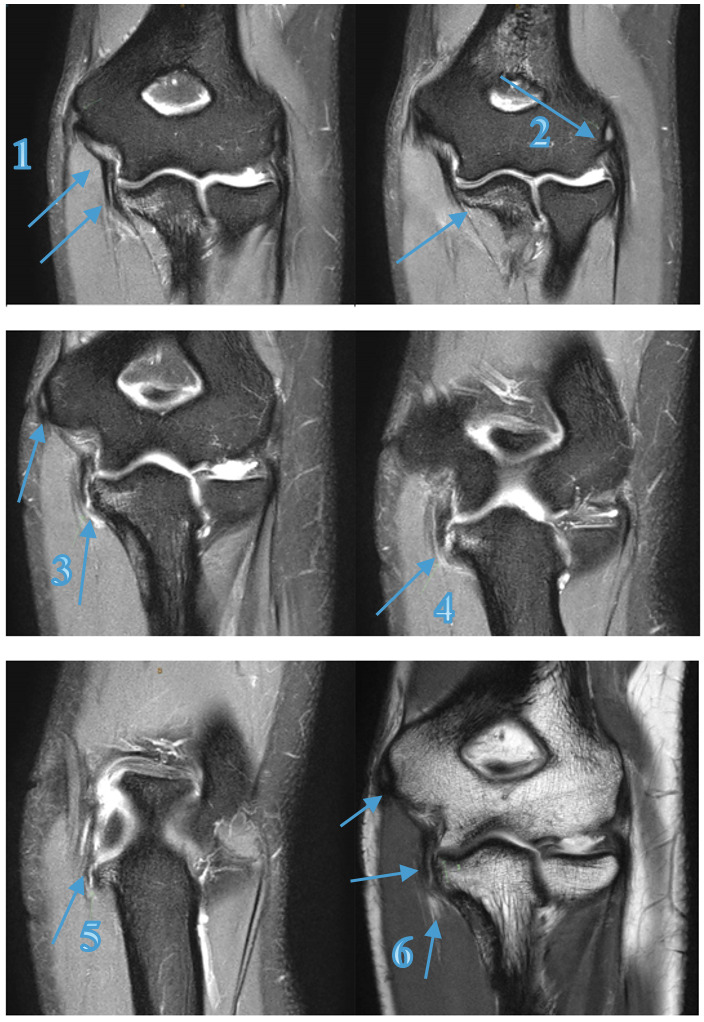
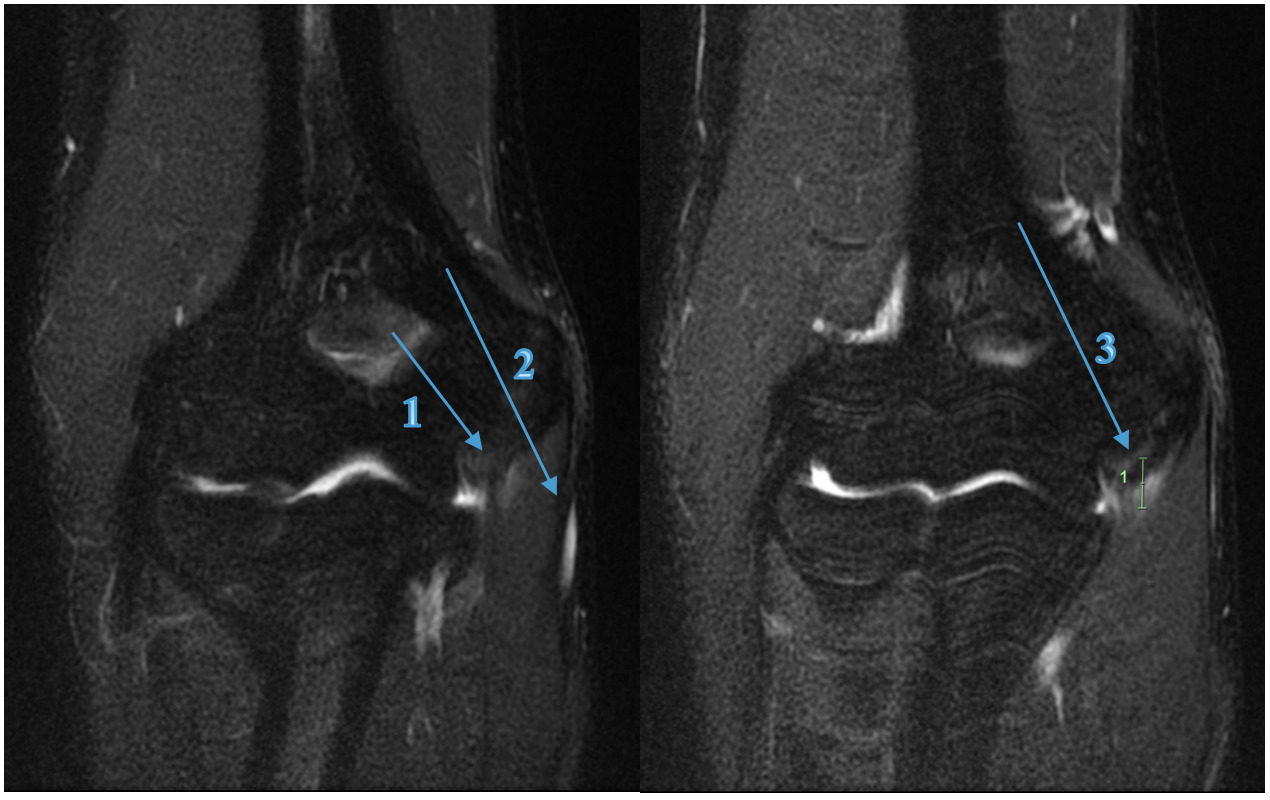
Athlete D
A 17-year-old amateur male Javelin thrower (State Representative) presented with right elbow pain which occurred during a competition 4 days prior. He described an audible pop and sharp pain experienced just before releasing the javelin. In the six weeks prior to the competition, the athlete experienced minor discomfort 3/10 (NRS) in the shoulder and medial elbow, which would ease at the completion of training and competition. As presented in Table 2 the physical examination findings, there was obvious swelling and palpatory tenderness over the medial elbow joint line (UCL/FCU & FDS tendons) and the medial epicondyle. The medial elbow dysfunction was exacerbated by any gripping or pronation motion reporting an 8/10 (NRS) at worst, reducing to 4/10 with the influence of ice, anti-inflammatories and analgesics as presented in Table 2 and 3. All activities ceased immediately until the pain and swelling was reduced. Due to the mechanism of injury and clinical findings, the practitioner referred him for MRI (Figure 3) which revealed a full thickness tear to the anterior bundle of the UCL with a low-grade partial tear of the FCU muscle, distal to the common flexor origin, which dictated the treatment choices and future modification to the training program.
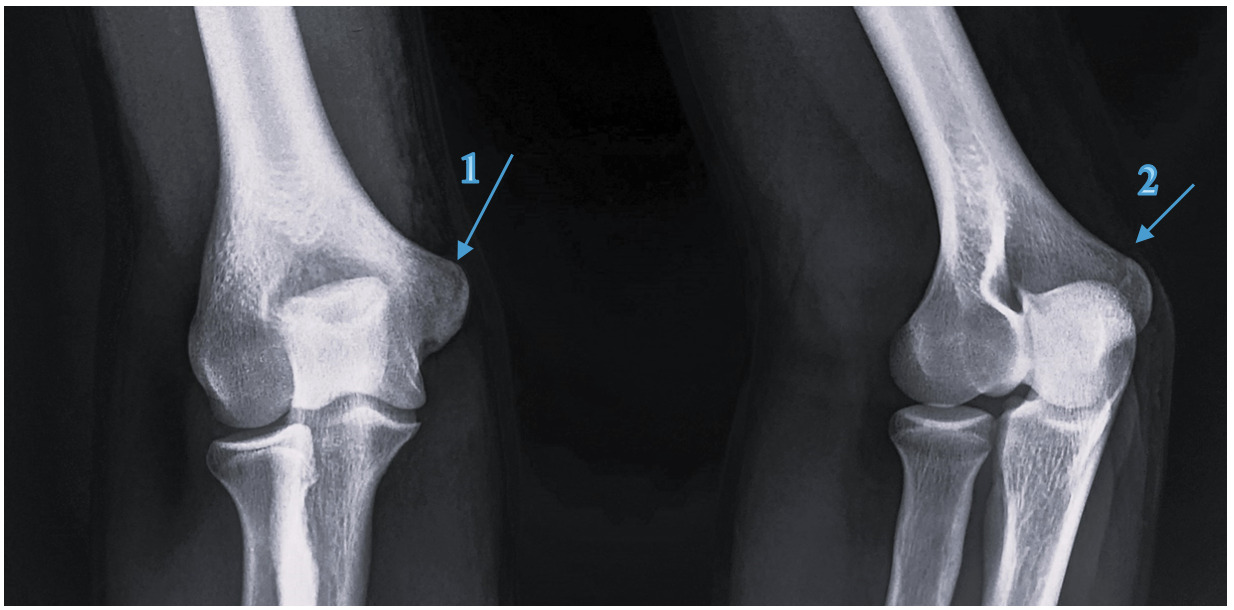
Athlete E
A 15-year-old amateur male Javelin thrower (State Representative) presented with a swollen and painful right elbow after throwing javelin in a competition three days prior to the appointment. The pain was felt immediately after releasing the javelin on his third throw of the competition with a 9/10 (NRS) pain and he was forced to withdraw. The pain remained 5/10 (NRS) for the following 7 days. Athlete E had been experiencing pain in the right elbow and forearm during the preceding month at training and competition, stating he had some discomfort after most training sessions. On physical examination, active full elbow flexion (45°) and extension (140°) was apprehensive and tuning fork vibration test over the medial epicondyle recorded a positive 7/10 pain (NRS) shown in Table 2, therefore referred for x-ray. The x-ray, Figure 4, revealed an avulsion fracture to the medial epicondyle with no displacement. Other clinical and associated findings uncovered during the physical examination were consistent with medial epicondylitis.
Interventions and Outcomes
Athlete A
The initial phase of Athlete A’s treatment and rehabilitation schedule was initiated with training modifications based on symptoms, with the goal of competing at week 6, as outlined in Appendix A and Appendix B. This was unsuccessful resulting in a complete remodel of the treatment and training program based off further investigation (MRI - Figure 2) and surgical opinion. After altering the treatment (Appendix A), rehabilitation, and training (Appendix B) over a 15-week period, the athlete rated “Excellent”37 Conway Scale (Table 3) and returned to high level competition at week 24 with a throw of 99.46% of previous personal best (PB) 76.34m (800g) and at week 27 a throw of 78.75m (800g) 3% greater than the previous PB.
The Conway scale was chosen as an outcome measure to assess the athletes return to play level.33,37
Athlete B
Athlete B initiated her treatment and rehabilitation schedule with strength training modifications, as she experienced symptoms during elbow flexion-compression based exercises such as the catch phase of the Olympic clean, and barbell pullover. Throwing exercises were omitted from her training program, as seen in Appendix B. The multimodal treatment schedule as presented in Appendix A, was implemented with a gradual return to throwing with unrestricted strength training. Athlete B was symptom free during the elbow orthopedic testing at 11 weeks of the treatment and rehabilitation schedule as seen in Appendix B. At week 20 post initial treatment date, she scored “excellent” on the Conway scale37 and was pain-free when performing high intensity throwing, returning to competition recording 61.42m (600g), a 1.8% improvement on her PB.
Athlete C
Athlete C required specific attention towards modifying the javelin technique through rehabilitation exercises, which was immediately included into her training program as seen in Appendix B. Post training symptoms were managed with ice and compression sleeve which provided relief in combination with other treatments as described in Appendix A. This included wrist and elbow mobility being incorporated into her daily training program, all training warm-ups and at home rehabilitation. Specific treatment protocol used for this athlete is presented in Appendix A. The athlete achieved an ‘Good’ on the Conway scale37 and returned to Javelin throwing after four weeks and ‘Excellent’ after 6 weeks, throwing 99.5% of her PB 52.81m (600g), and four weeks later improving her PB by 3.3% with a throw of 54.64m (600g).
Athlete D
Athlete D began treatment and rehabilitation with daily wrist and elbow mobility as outlined in Appendix A, commencing from the conclusion of initial diagnosis. The specific treatment protocol used for this athlete is described in Appendix A. The athlete achieved an ‘Excellent’ on the Conway scale37 and returned to Javelin competition at 27 weeks throwing 96.3% of PB 56.68m (700g).
Athlete E
The initial management for Athlete E was complete rest from training and competition, with chiropractic therapy, as presented in Appendix A. Conservative rehabilitation was initiated at 14 days which included wrist mobility and forearm flexibility exercises, as outlined in Appendix B. The athlete achieved an ‘Excellent’ on the Conway scale37 and returned to Javelin competition at 18 weeks throwing 98.2% of PB 54.12m (700g), with an improvement of 3.2% to 56m (700g) after 26 weeks.
DISCUSSION
Overall, this case series demonstrates positive outcomes from a multimodal chiropractic treatment and management plan for five javelin athletes with medial elbow injuries.
Historically, literature reporting medial elbow injuries has focused on athletes participating in baseball, hence the commonly accepted terms for medial elbow injuries such as, “pitcher’s elbow” or “Little League Elbow” or more recently “golfer’s elbow”, however, this injury can affect athletes participating in any overhead-throwing sports including softball, football, tennis and javelin.3
Javelin injuries affecting the medial elbow are usually chronic and progressive, with a gradual decline in throwing performance measured by velocity, accuracy and endurance.38 Due to the ballistic nature of the javelin throw when acute injuries occur it can result in an inflammatory response to the active stabilizers of the medial elbow and are often due to the excessive valgus forces with medial distraction of the ulnotrochlear joint.8 Repetitive high force throwing can lead to traumatic compression of the posteriomedial olecranon and trochlea resulting in osseus injuries including reactive bone formation, chondral damage, synovitis, loose bodies, VEOS.39
The risk of elbow injury increases with poor mechanics of the throwing technique.4,6,8 If scapular and GH mechanics are poor, due to limitations in joint mobility and/or muscular weakness, correct shoulder ‘cocking’ motion becomes limited, and the athlete will be unable to adequately move the shoulder through the throwing motion as seen in the delivery phase of Figure 5.
The shoulder position is set during the run up (transition & intermediate strides Figure 1) and delivery stride phases. If not set appropriately during these phases, it becomes difficult to correct the throwing arm which will result in a low carrying angle (below the shoulder), with greater elbow flexion, exposing the elbow to higher amounts of valgus strain.12,19 This was observed in Athletes D & E into the delivery phase, with Athletes A & C flexing the elbow during the delivery stride phase and Athletes A, D & E with lack of supination.
The introduction of the delivery phase, the cocking phase, will initiate upward rotation (posterior tilting) and retraction of the scapula, maximizing external GH rotation and providing a stable base for the humerus to effectively rotate at high velocities during the acceleration phase.3–5 This accelerative torque influences the amount of force the shoulder can produce resulting in the late cocking phases whipping action, creating maximal valgus tension through the elbow, as the elbow moves into flexion.6 Athletes A and C displayed early cocking phase mechanics but did not maximize scapular retraction and posterior tilting, resulting in 90° humeral abduction introducing a flexed ‘shortened’ right elbow to generate tension in a lower abducted humeral position. Athletes B, D, E exhibited little cocking action, resulting in between 60°-80° humeral abduction with between 50°-90° elbow flexion as seen in Table 2.
The acceleration phase is the most ballistic movement of the javelin throw, starting when the shoulder assumes the position of maximal external rotation, to javelin release.40 Valgus tension of the elbow is at its greatest as a result of the GH external rotation lag generated in this phase which is primarily restrained by the anterior bundle of the UCL.4 Athlete A, B, D experienced damage to the UCL, correlating with the literature and the faults they exhibited during acceleration phase of the throw, seen in Table 2. Athlete A rupturing half of posterior anterior bundle, matching the flexion about of approximately 80°.
The deceleration phase begins at javelin release, creating high eccentric tension on the posterior scapulo-humeral decelerators and follow through effects on the elbow, forearm and wrists. The elbow undergoes forceful flexion to extension with the completion of the ‘whipping action’, placing high stress on elbow joint osseous articulation (VEO diagnosis: Athlete B, C). Pronation of the wrist through rapid acceleration of the flexor pronator group influences medial epicondylitis (Athlete A, C) and osseous changes to the medial epicondyle (avulsion fracture medial epicondyle: Athlete E).
As previously mentioned, the athletes were managed by two practitioners with experience as athletics coaches, strength and conditioning practitioners, and sports chiropractors. Their assessment of the athletes involved a well-rounded approach assessing pain, function, ADL’s and sports specific capability. Functional ability and pain patient reported outcome measures (PROMs) were used to assess the athletes. Clinical functional ability was evaluated using shoulder, elbow and spinal ROM, ability to perform sport specific activities and orthopedic tests. The pain of the athletes was measured using an 11-point numeric rating scale (NRS) where the patient circles the most appropriate number to represent their level of pain, 0 signifies ‘‘no pain’’ and 10 represents ''worst possible pain".41–43
Physical Examination
A physical examination should include visual inspection, palpation, provocative maneuvers, orthopedic tests, neurological examination, and if clinically indicated diagnostic imaging.44 The evaluation of patients within this case series included medical history consultation, physical examination (postural, neurological and orthopedic/functional), kinetic chain evaluation and sport specific function.
Visual Presentation
On postural examination, the athletes shared a common observation with the elbow being held in flexion at approx. 20°-30°. The valgus carrying angle is defined by the angle that is formed between the long axis of the humerus and the long axis of the ulna.45 The average range is between 11° to 14° in males and 13° to 16° in females.11,46,47 Research amongst baseball players by Erickson et al., 2019, determined that an increase in the valgus carrying angle of the dominant elbow may be an adaptive change due to arrest of the lateral physis growth, prolonged medial elbow tension, wear and/or compression of articular cartilage or laxity of the medial structures.48 Shah et al., 2017, reported that an increase in valgus carrying angle of the throwing arm increased the likelihood of a shoulder/elbow injury in baseball pitchers. Whether javelin throwers are at the same risk of injury due to the increased carrying angle has been less clearly documented.
Pardiwala reports postural asymmetry in the overhead athlete’s scapulo-humeral and scapulo-thoracic rhythm is commonly due to the dominant use of the throwing arm and may be associated with injuries.9 Kibler et al. showed that individuals who have clinically significant UCL injuries had a higher prevalence of GIRD and scapular dyskinesis.44
Palpation
On physical examination of the athletes in this study tenderness was elicited over the medial elbow joint line, UCL and sublime tubercle attachment. In a study by Karbach et al, 2017, tenderness over the UCL has a sensitivity of 81%–94% and a specificity of 22% for an UCL tear.14 Additionally, patients reporting palpatory tenderness approximately 2 cm distal from the medial epicondyle has been shown to have good reliability when diagnosing UCL injuries.25 Rahman et al. agreed that point tenderness directly over the UCL or close to the insertion sites are suggestive of UCL injury.20 Additional palpatory pain associated with both the posterior and medial aspect of the elbow has high correlation of VEOS.8,15 Direct pain over the medial epicondyle with referral into flexor pronator musculature, are suggestive of medial epicondylitis or epicondylar injuries.24,26,28 The palpation findings and the diagnoses of these athletes are consistent with the literature.
Range of Movement
Although it could be assumed that ROM is affected in elbow injuries, Biz et al., 2019 and Sanchez-Sotelo & Morrey 2016, reported that medial joint swelling and point tenderness over the ligament without any limitation to the ROM are commonly seen in acute or subacute presentations of UCL injuries.34,49 Testing the athletes intra-articular movement (joint play) revealed an increase in ulnar glide or medial joint distraction; and decrease in radial glide or lateral joint compression, relative to the humerus, producing crepitus and grinding in the posterior/posterior-medial elbow and laxity in the medial elbow.
Orthopedic Tests – Specific to Medial Elbow Injury Diagnosis
Three orthopedic tests specific to this case series and commonly included in the physical examination of the medial elbow joint are the valgus stress test, milking maneuvers, moving valgus stress test.50 A diagnosis of elbow instability can be made using these specific tests in combination with the clinical presentation.14
On valgus stress test, Athlete A, B, D reported pain over the medial joint line, with medial joint laxity (opening) without a firm endpoint. Athletes C, E also experienced pain, superior to the medial joint line and didn’t exhibit joint laxity.
The Milking maneuver had positive findings for Athletes A, B, D which assisted to clinically diagnose the UCL tear. Athlete C had some discomfort to the medial elbow but no instability.
The moving Valgus stress test is highly sensitive and specific to diagnose a UCL tear, and necessary for any overhead throwing athlete due to positional similarities to the throw. Athletes A, B, D experienced positive findings of pain.
Imaging
MRI has typically been the gold standard imaging modality in identifying tendon and ligament pathology such as UCL injuries, particularly when full-thickness tears are present.10,51,52 Athlete A’s UCL injury was diagnosed by physical examination and confirmed by MRI (Figure 2), and Athlete D (Figure 3) also had diagnoses confirmed by MRI.
Medial elbow pain in throwing athletes will typically have normal findings on plain radiographs, although chronic or degenerative UCL’s may show evidence of calcifications.53
The sports chiropractors decided not to refer Athlete B for imaging, rather using their clinical experience, the athlete’s history and clinical presentation to make a working diagnosis of pathological findings and initial conservative management. Athlete E was referred for x-ray (Figure 4) 5 days post injury incident to confirm a fracture to the medial epicondyle (Little Leaguers Elbow), after clinical examination suggested its likeliness.
The treatment and management was not dictated solely on these imaging findings, but in conjunction with the physical examination and clinic history.
Medial elbow injuries
Differential diagnoses of medial elbow pain commonly discussed in literature include but are not limited to medial epicondylitis, avulsion fracture, occult fracture, UCL injury, synovitis, osteoarthritis and tendinopathies.22,33,54,55 The injuries within this case series include UCL injury, medial epicondylitis, avulsion fracture, tendinopathy and VEOS.
UCL injury was the most common diagnosis amongst the athletes in this series, with three out of five athletes experiencing this problem. Literature suggests that overall, most commonly UCL injuries did not require surgery and could be managed conservatively, which was the case for all five javelin throwers in this study.13,14,56–58
Medial epicondylosis/litis is seen in throwing athletes, often manifesting as pain during or after a period of throwing and is frequently associated with an increase in training volume or more intense throwing program.8,59 As presented in this paper, three of these athletes were diagnosed with UCL injuries and all five with medial epicondylitis.
Trauma resulting in valgus stress on the elbow, seen with athletes involved in throwing sports, are particularly susceptible to avulsion and stress fractures to the medial epicondyle or sublime tubercle due to the high load and forces during the acceleration and deceleration phase of the throwing action.53,60 Athlete A, was diagnosed a UCL tear/rupture and avulsion fracture of the sublime tubercle, confirmed on MRI. The tensile strength of the UCL is often overcome by the throwing force, especially in the elite athletes, where repetitive microtrauma can weaken and ultimately tear the ligament or cause avulsions fractures.61
Tendinopathies, Tendonitis, Tendinosis have evolving terminology but generally refer to persistent tendon pain and loss of function due to mechanical loading.13,60,62 Tendon tears, either partial or complete, refer to macroscopic discontinuity of load bearing tendons and can be common in throwers.63 All athletes in this study had specific tendon injuries of the flexor pronator tendons.
Valgus extension overload syndrome (VEOS) (posterior-medial impingement syndrome/pitcher’s elbow) is a common condition seen in overhead athletes characterized by impingement of the posteromedial tip of the olecranon process on the posteromedial wall of the olecranon fossa.64 Chronic medial elbow stress can create an adaptive reaction of scar tissue and osteophyte formation on the posteromedial aspect of the elbow and is commonly associated with UCL injuries (Athletes B, D). It is predominately caused by hyperextension and supination of the lower arm in the throwing action in the deceleration phase, which Athlete B, C and D exhibited.65
Influencing Factors to Elbow Injuries
Athletes with significant UCL injuries also exhibited shoulder pathology and scapular dyskinesia.4–6,9,44 Postural changes with throwing athletes can influence the fluidity of scapulothoracic and scapulohumeral rhythm, altering the throwing motion and upper limb mechanics.25,50 The presence of shoulder and scapular pathology increases the likeliness of elbow injuries occurring in overhead throwers.7 Thoracic, cervical spine, parascapular musculature and the ulnar nerve pathway were frequently examined and treated by the practitioners. All athletes presented with associated findings including wrist and shoulder pathology, poor scapulohumeral biomechanics, cervical, thoracic, and lumbar pathology as seen in Table 2. The sports chiropractors also examined the spine and upper limb orthopedically (Table 2) and provided appropriate treatment to the influencing structures to elbow injury (Appendix A), completing a holistic, multimodal treatment approach.
Multimodal Treatment and Management Approach
A multimodal treatment approach was utilized throughout this case series, consisting of sequential and progressive multiphase application of treatment and rehabilitation techniques with overlapping stages to optimize the clinical outcomes.
Manual soft tissue therapy, dry needling, low level laser therapy (LLLT)/Photobiomodulation (PBM), spinal and peripheral joint manipulation/mobilisation and upper extremity rehabilitation program are all described in literature for medial elbow injuries.8,10,32,34,39,50,66,67
Throwing/activity modification, modalities, physical therapy exercises including stretching and strengthening, nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroid injections/orthobiologics, and a gradual return to throwing program is the general consensus for treatment of medial elbow injuries.39,68,69
Soft Tissue Therapy
ART® is a soft tissue therapy which is a manual therapy and case-management system that allows a practitioner to create working diagnoses and treat soft-tissue injuries.50 The philosophies of the treating practitioners, was to use ART® to compliment manipulative/mobilisation techniques. The clinical relevance of the ART® interventions aimed to influence restoration of joint biomechanics, muscular and connective tissue integrity and reduce the incidence of scar tissue formation and fibrous adhesions to injured structures. The clinical findings of this case series showed gradual improvements in tissue quality and function, observed with improved ROM and strength, which allowed the athletes to progress their rehabilitation and training to more advanced levels, Appendix B.
Dry Needling
Research indicates that the definition of dry needling has been broadening to encompass the stimulation of neural, muscular, and connective tissues, not just trigger points.70,71 The results from a systematic review, involving 426 participants, suggested that dry needling of trigger points in the triceps muscle could have a positive impact on both muscle stiffness and functional outcomes.71 The clinical findings in this case series mirrored these findings, for an increase in function and decrease in muscle hypertonicity post dry needling treatment.
Low Level Laser therapy (LLLT)/Photobiomodulation (PBM)
The terms low-level laser therapy (LLLT), photobiomodulation (PBM) and light-emitting diode therapy (LEDT) are commonly used throughout literature.72 It is the use of near-infrared (NIR) or ultraviolet to red light applied to damaged tissue to stimulate, heal, regenerate, having photochemical and biophysical effects within the targeted tissue.72,73 A, C and D experienced two protocols using a Multi-radiance MR4 Activ at the 1-250hz and 1000hz settings. Applied for two cycles between 3-4 minutes as seen in Appendix A, reduction in inflammation during initial phases was noted as well as changes in the athletes’ subjective report of pain.
Joint Manipulation/Mobilization (Adjustments)
Spinal and peripheral joint manipulation/mobilization is an intervention commonly administered by manual therapy practitioners with the goal of restoring joint function.50,60 Joint manipulation/mobilization is performed by applying a high velocity, low amplitude thrust of specific magnitude in a controlled manner to a targeted joint which causes mechanical, neurological, and biological effects.50,74 The rate of improvement was more pronounced relating to joint restoration, ROM and strength, during the initial phases of treatment. Reductions to joint restriction and aberrant movement patterns were observed as a result of spinal and peripheral adjustments as seen in Appendix A. During the later stages, manipulation and mobilization therapies continued to reiterate improved joint biomechanics and posture, influencing the physical retraining administered during rehabilitation therapy.
Rehabilitation
The rehabilitation sequence used in this case series follows a progressive multi-phased approach, with an initial goal to relieve acute symptomatology, rehabilitate the pathologic tissues, and prevent future recurrence.22 Return to training and competition was guided by functional movement quality, absence of medial elbow symptoms during chiropractic and sport-specific assessments by the athlete’s clinicians. Returning the athlete to prior injury state was the first objective, then to increase their personal best ability. The examination and assessment of the elbow and shoulder enabled an appropriate and specific rehabilitation plan, targeting retraining and restoration of the proprioceptive (sensorimotor) systems using closed and open chained and plyometric exercise. Athletes A, B and C were only symptomatic in valgus tension of the elbow at moderate to high velocity throwing, allowing for immediate progressive rehabilitation of the injured tissues and those influencing (elbow & shoulder) continuing strength and conditioning training with exercises that avoided loading the injured structures. Athlete D and E followed a rehabilitation strategy appropriate to their experience, age and presentation. All rehabilitation phases are in conjunction with manual therapy modalities as seen in Appendix B.
Four progressions of rehabilitation were administered in this case series as presented in Appendix B, initiating immediately and being incorporated into normal training programs at the conclusion of their management. Phases I and II, followed a traditional rehabilitation approach with restoration strength, posture and stability through the elbow and shoulder progressing to the addition of proprioceptive and strength at range training. Phase III is where the additional knowledge of the sports chiropractors as elite coaches of strength training and the javelin throw enabled the reintroduction of specific movements which caused injury to occur, to be achieved under appropriate loads in segregated movements. This was executed in the form of throwing movements, banded and strength-based exercises, repetitively using strength training procedures. Phase IV progressed the technical remodeling with the javelin implement while applying progressive overload to specific rehabilitative strength exercises in Phase III. The progress of the Conway scale through the stages can be seen in Appendix B as well as each exercise and progression of the rehabilitation program.
Limitations
An inability to establish a causal relationship due to the lack of a control group, makes case series susceptible to bias and limiting the generalizability of the findings. A specific limitation of this case series is a lack of patient reported outcome measures to objectively measure change, throughout the cases. Additionally, being that the cases were all treated using a multimodal approach, there is no way to determine which, if any individual treatment may or may not have contributed to the perceived beneficial outcomes. Despite these limitations the clinical outcomes presented in this research could be useful to guide treatment and further research, particularly for allied health practitioners providing treatment to javelin athletes. Although all five athletes all showed positive benefits after a multimodal chiropractic treatment approach, the generalizability of these results is limited due to the case series methodology and improvements due to the passage of time cannot be ruled out.
CONCLUSION
The results of this case series demonstrate potential benefit of a multimodal chiropractic treatment and management approach in five javelin throwers with medial elbow injuries. All athletes scored an excellent on the Conway scale and were able to return to training and competition within 12-26 weeks of the initial injury presentation.
Each athlete returned to full functional capacity of the elbow and associated structures. Performance outcomes of javelin competition for all athletes were within 4% of throwing best or new PB on initial return to competition. Four of the five athletes would continue to throw PB performances within eight weeks of returning to competition.
Conflicts of interest
The authors report no conflicts of interest.
ACKNOWLEDGEMENTS
The authors would like to thank the patients whose cases were presented in this case series.
.png)


.jpg)
.png)
.jpg)