Introduction
Shoulder injuries are common in overhead athletes involved in sports such as volleyball, baseball, and handball. These athletes often subject their shoulders to repetitive, high velocity movements that place stress on both the active and passive structures within the joint.1,2 Much of the current research investigating shoulder injuries in overhead sports involves throwing athletes. In throwing athletes’ shoulders, during the cocking and deceleration phases of throwing, the glenohumeral joint (shoulder) must withstand distraction forces up to 120% of bodyweight,3 and shoulder internal rotation torques between 40-50 Newton-meters (Nm), respectively.4 Fleisig et al.,5 examined the torques placed on the throwing athlete’s shoulder and found high levels of internal rotation torque which is thought to contribute to the risk of overuse shoulder injuries. These high forces imparted on the shoulder also affect volleyball players during routine hitting maneuvers such as spiking and serving. Epidemiological evidence indicates that about 8-20% of injuries in volleyball occur at the shoulder.1,2,6–9 Volleyball players are typically afflicted with various shoulder pathologies, often resulting from overuse, including rotator cuff tendinopathy, suprascapular nerve impingement, and labral pathology.2 Despite this, shoulder injuries and pathologies in overhead athletes are understudied when compared to the lower extremities.
In particular, strength of the rotator cuff muscles’ is critical for overhead athletes to function at a high level as deficits in rotator cuff strength have been shown to be associated with elevated injury risk.7,9 There are various methods to assess rotator cuff strength including the gold-standard, stationary isokinetic dynamometer or the portable, cost-efficient, and widely available handheld dynamometer (HHD). As with all clinical testing, it is important to have valid and reliable methods for assessing strength. While the HHD is a clinically effective tool for measuring strength and it has been shown to have strong reliability and validity with stationary dynamometers, they can be subject to high variability due to patient set-up, HHD placement, and patient compliance.10,11
The majority of studies have performed rotator cuff strength testing in a neutral position, 0° of abduction.10,12 However, when evaluating overhead athletes, it is more common to also assess rotator cuff strength in more “sport specific” positions such as the 90°/90° position which involves 90° of abduction and elbow flexion.13–15 While measurements taken in the 90°/90° position are easily replicable and have high reliability and validity,13–15 a significant limitation is that it does not best capture the positional strength for overhead athletes who perform their sport in greater degrees of shoulder abduction. Volleyball players, for example, perform front row attacks, serves, and overhead hits between 116°-130° of shoulder abduction, and approximately 90° of shoulder external rotation (ER).4,16 Along with the range of motion demands, the shoulder undergoes high angular velocity of IR, reaching at times 2594°/sec, which generates exceedingly high ball spiking speeds around 15.5 m/s.4 Due to the high demand that volleyball players place on their shoulders, it is pertinent to develop strength testing methods to more accurately reflect the positioning of the upper extremity during sport performance. Establishing a more sport-specific testing position would also assist in identifying risk factors for shoulder injuries throughout a season and potentially assist in injury prevention programming.
Therefore, the purpose of this current study was to determine the inter- and intra-rater reliability of measuring shoulder internal rotation (IR) and external rotation (ER) strength at a novel testing position, 130° of abduction and compared to the 90°/90° position. A secondary aim was to assess concurrent validity between measurements taken with the Humac® Norm™ Isokinetic Dynamometer and Microfet® 2 hand-held dynamometer (HHD).
Methods
Participant Recruitment
After receiving approval from the Institutional Review Board at the medical institution, twenty-five (n=25) healthy, active participants were recruited from an outpatient sports medicine facility. A power analysis was conducted prior to data collection. A sample size of 25 subjects was considered to sufficiently power for the study.
All participants were recreationally active and between 18-50 years old. Participants were excluded if they had experienced shoulder pain in the prior three months, previous shoulder surgery, or contraindication to exercise as outlined by the ACSM guidelines.17 An electronic informed consent form was read, reviewed and signed prior to any performance testing. All data was blinded and stored on a secure database, REDCap® (Vanderbilt University, Nashville, TN) electronic data capture tools.18
Instrumentation
Testing equipment included the Humac® Norm™ (CSMi, Soughton, MA) isokinetic dynamometer (IKD) and the Microfet® 2 HHD (Hoggan Scientific LLC, Salt Lake City, UT).
Testing Procedure
On testing Day 1, participants performed a five-minute warmup on an upper body ergometer at a self-selected intensity and demographic data including height, weight and arm length, measured from the lateral epicondyle to the head of the 3rd metacarpal, was obtained.
Isometric Testing Using the Isokinetic Dynamometer
The participants were then tested on the IKD and randomly assigned to begin with the right or left shoulder. The participants were positioned by both Tester 1 and 2 together in a seated position on a foam pad, spine flat against a 24-inch plyo box, and legs supported by a foam roller and positioned close to the IKD arm so that their arm was in 90° of both elbow flexion and shoulder abduction while holding onto the handle attachment (Figure 1). These angles were verified by goniometric measurement by both testers. Testing began with one familiarization rep at approximately 75% maximal voluntary contraction (MVC), patient determined, for shoulder IR, prior to a 20 second rest period. The participant was instructed to maintain their scapulae flat on the box, hips on the ground and contralateral arm over the testing shoulder while performing the isometric contraction. This was then repeated for three maximal effort trials of three second contractions, followed by a 20 second rest period between reps. This process was again performed for shoulder ER, prior to the arm being elevated to 130° of abduction following the same testing procedure above, for shoulder ER and IR. The other shoulder was tested following the already described procedure. Consistent verbal encouragement was provided to the participant during the testing. The average peak torque of the three repetitions which was converted to Newtons via and was used for analysis to compare to the HHD, which outputs force in Newtons.
Isometric Testing Using the Microfet® 2 HHD
Following testing on the IKD, the subject was given five minutes of rest. They were randomly assigned to test with Tester 1 or 2 and randomly assigned which shoulder would be tested first. Each tester independently positioned the patient relative to the wall, in the same position described above see Figure 2a and b, provided stabilization to the box for support, and verified shoulder position with goniometric measurement. For testing IR, the HHD was placed in the palm of the subject’s hand. For testing ER, the dynamometer was secured to the back of the subject’s hand. The participant began by testing shoulder IR at the 90°/90° position with one familiarization repetition, followed by three maximal effort contractions for three seconds, followed by 20 seconds of rest in between repetitions. The patient was allowed to rest their arm down between repetitions to avoid fatigue effects. The patient was then tested for shoulder IR at 130° of abduction following the same process. This was then repeated for shoulder ER, before switching arms. Following testing of both arms, the participant was then tested by the other tester, following the same procedure as outlined above. Data were collected for the three maximal effort contractions and averaged to find the peak average force.
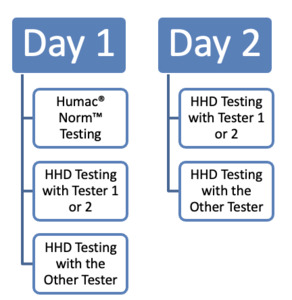
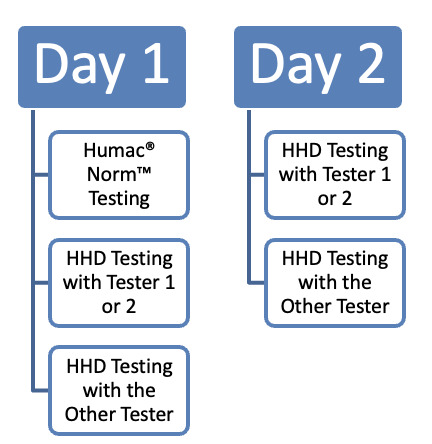
On testing Day 2, which occurred 7-14 days after the initial testing, the participant was instructed to warmup again on the upper body ergometer. Testing on the IKD was not performed on Day 2, rather only HHD was performed by each tester. The participant was again randomly assigned to a tester and which shoulder to be tested first. The testing procedure was the same as described in the prior paragraph. For further details regarding the testing protocol, consult with the Figure 3 flow diagram.
Statistical Analysis
Intraclass correlation coefficients (ICCs) were calculated to determine reliability and validity of isometric strength measurements from a novel, sport specific testing position between a stationary IKD and an HHD and between a novice and experienced physical therapists (one and five years of experience respectively) using only the HHD. The general guidelines for interpreting ICCs are as follows: values less than 0.5 indicate poor reliability, values between 0.5 and 0.75 indicated moderate reliability, values between 0.75 and 0.9 indicate good reliability, and values exceeding 0.9 indicate excellent reliability.19 In addition, the limits of agreement between measurements from the two testing devices were evaluated using Bland-Altman plots. Additional analyses involved quantifying responsiveness of testing strength in this novel position by calculating the minimal detectable change. Statistical analysis was performed using BlueSky Statistics version 7 (BlueSky Statistics LLC, Chicago, IL).
Results
Participant Demographics
Twenty-five participants completed the full testing battery. The average age of the participants was 27 years old (± 4.4 years) with 13 subjects being male and 12 being female. All participants were healthy without a history of shoulder surgery or contraindications to exercise as outlined in the inclusion criteria.
Reliability
Inter-rater reliability demonstrated a strong relationship and overall good to excellent agreement. This was true during both Day 1 and Day 2. The ICC values and standard deviations (SD) can be seen in Table 1. Intra-rater reliability was also strong between the experienced (Tester 1) and novice (Tester 2) clinicians with good to excellent agreement.
Concurrent Validity Between Testing Methods
There was moderate to poor agreement between the HHD and IKD for isometric strength testing in all testing positions and both limbs. The ICC values for shoulder ER at 90° was 0.296 and 0.449 on the right and left shoulders respectively. The ICC values for shoulder IR at 90° was 0.405 and 0.331 on the right and left shoulders respectively. The ICC values for shoulder ER at 130° was 0.192 and 0.321 on the right and left shoulders respectively. The ICC values for shoulder IR at 130° was 0.413 and 0.368 on the right and left shoulders respectively. This data is summarized in Table 1.
Bland-Altman plots were created as a method of qualitative analysis of the concurrent validity and agreement between testing methods.20 These plots for each testing position can be observed in Appendix 1. To summarize these plots, HHD measurements consistently reported greater strength measurements compared to the IKD. For shoulder ER strength at 90° of abduction, the HHD strength measurements were greater by between 11-20 newtons (N). For shoulder IR strength at 90° of abduction, the HHD strength measurements were greater by 36-37N. For shoulder ER strength at 130° of abduction, the HHD strength measurements were greater by between 15.6-19.4N. For shoulder IR strength at 130° of abduction, the HHD strength measurements were greater by between 34.7-39.7N. A summary of these average strength differences between devices can be observed in Table 2.
Responsiveness
In addition to reliability measures, responsiveness measures were calculated with minimal detectable change (MDC). These values for each shoulder position are listed in Table 1.
Discussion
The current study’s purpose was to determine the inter-rater and intra-rater reliability of using HHD measurements of rotator cuff strength at 90° and 130° of abduction as well as the concurrent validity of HHD compared to the IKD. The results indicate good to excellent agreement for intra- and inter-rater measurements. This demonstrates that hand-held dynamometry is a reliable measure between sessions and clinicians to measure shoulder RC strength at both 90° and 130° degrees of abduction. The results are consistent with the current body of research indicating that using HHD to quantify rotator cuff strength is reliable within and between raters.13,15 Two studies13,15 previously have assessed the 90° of abduction position and other common positions to measure shoulder strength. Based on the literature review, no study prior to this has assessed the ability to reliably measure rotator cuff strength at 130° of abduction. The results indicate that clinicians of multiple experience levels can reliably measure ER and IR strength in the 130 degrees of abduction position. This is consistent with a study performed by Roy et al.10 who found a high degree of reliability when testing shoulder flexion and extension strength at 140° of abduction as well as rotator cuff strength at 90°. In terms of responsiveness, this study establishes a minimal detectable change for shoulder rotator cuff strength in this testing position. However, these values for MDC may be larger in the normal population sample with large standard deviation between subjects, and different results may occur in an athletic population whose shoulder strength measures may be more similar to each other.
The agreement between the hand-held measurements and IKD was moderate to poor. The HHD consistently overestimated rotator cuff strength when compared to the stationary dynamometer. HHD and stationary dynamometers have been compared previously and show moderate to strong correlations when examined in the lower extremity. Hirano et al. compared knee extensor strength between devices and found ICC’s greater than 0.7521. Muff et al. also examined the ability to measure quadriceps and hamstrings strength between HHD and stationary dynamometers with the ICC’s ranging between 0.72-0.87.21 Additional studies have examined concurrent validity of shoulder ER and IR strength, and this has been previously reported to be 0.664-0.792),15 0.65-0.82,22and 0.45-0.8112 demonstrating moderate to strong agreement between devices at the 90°/90° and standard neutral positions.12,15,22 Although the present study demonstrated moderate to poor agreement between the devices, the Bland Altman plots display no inherent, systematic biases in the measurements. This implies that the devices should not be used interchangeably. The differences seen in measurement between devices may be related to patient comfort during testing, for example the arm being tested on the IKD was freely hanging, as compared to the HHD testing setup where the participant was able to brace their arm on the wall.
The positions of measurement for this testing protocol were chosen to be easily reproducible in a clinic setting. Previous studies assessing rotator cuff strength at 90° of abduction are often performed in the supine position,15,22 as well as in a standing position.12 Rotator cuff strength has also typically been assessed in the scapular plane of motion.10,12 The testing protocol in this current study was designed to avoid compensatory trunk involvement (i.e. trunk flexion for IR and trunk extension for ER) during shoulder force production, which may artificially inflate the force generated. The results demonstrate strength was reliably measured within and between raters. This indicates that this position can be considered when assessing shoulder ER and IR strength, potentially testing at both the 90°/90° position and the 130° of abduction position.
Limitations
There are several limitations to the study design. First, the participant sample was not a random selection, but a convenience sample. This sample included young to middle-aged, active individuals without a history of shoulder surgery or current shoulder pain. This limits the generalizability of these procedures when assessing patients with current shoulder pain or dysfunction.
The testing position selected for this study included the use of a 24-inch plyo box to stabilize the participant’s spine. Depending on the length of the individual’s torso, this may have affected the participant’s ability to produce force related to how much surface area of the participant’s torso was along the box.
There was also a risk for an order or learning effect as the participant performed testing on the IKD prior to the HHD. It is possible that as participants gained experience with the testing positions, they produced more force. Additionally, there is a possibility of a fatigue effect, with HHD measurements possibly being artificially lower due to always being tested second. However, previous research on learning effects on the Y-Balance Test has shown that results plateau after six repetitions.23 While this is a different testing procedure, it is reasonable to extrapolate given that each participant performed over 10 repetitions in each position for each shoulder in the study design, any learning effects are likely negated by the protocol. To combat fatigue, a 5-minute break was instituted between testing of the IKD and HHD. Rest time between repetitions was also instituted between repetitions, similar to previously published protocols.10,12
Another limitation is the use of a single familiarization trial with each testing medium and position. This was chosen to also combat the effects of fatigue and complete each testing session in a timely manner. However, with only a single familiarization trial, the possibility of a learning effect across a participant’s testing increases, as well as a higher variability in results as testing positions become more known. Future studies could remedy this by having a separate familiarization session so that all participants are exposed to the testing procedure prior to data collection.
There was also risk of bias as Tester 1 recorded the HHD data while Tester 2 performed testing and vice versa. In order to combat this, data were recorded on different REDCap® columns that were hidden from the recorder as soon as the data was recorded. Although the results were not hidden from the recorder before testing, with the amount of data collected, it is unlikely the testers could memorize the previously recorded data. Care was also taken to avoid this bias through randomization of which tester would conduct HHD first.
Future directions
Future research should focus on furthering the ability to reliably measure rotator cuff strength in these positions for overhead athletes, notably volleyball players. This current data also allows the ability to track strength changes throughout seasons for volleyball athletes and this should be considered. These measurements could also be applied across seasons and cohorts to determine correlations to injury occurrence and metrics of performance. Howard et al. measured torques at the shoulder to be 44 N-m due to internal rotation (IR) and 63 N-m for horizontal adduction during a volleyball spike.6 Due to these high torque values, exploring strength measurements across a season can give necessary information that would inform programming to prevent or reduce injury risk. Isometric strength has already been used in baseball populations to help track these metrics. Testing in more sport-specific positions, such as 130° of abduction for volleyball, can assist in more accurately identifying pertinent deficits.
Conclusion
The results of this current study demonstrate shoulder IR and ER isometric strength testing in 130° of abduction can be done with excellent inter and intra-rater reliability. The current testing protocol had fair, or poor to fair, agreement compared to the gold standard IKD. Therefore, results between the two measurement devices, although reliable, are not valid comparisons (should not be used interchangeably). More research is also needed to determine if clinicians can reliably measure strength in these positions in both injured and healthy overhead athletes.
Conflicts of Interest
The authors report no conflicts of interest.
Acknowledgements
This project was completed in partial fulfillment of capstone research requirements of the Mayo Clinic School of Health Sciences Sports Physical Therapy Residency for John Loepfe P.T., D.P.T., CSCS.