Introduction
Ankle injuries are among the most common musculoskeletal issues encountered in clinical practice, with the deltoid ligament involved in 10-15% of all ankle sprains. While deltoid ligament injuries are often associated with ankle fractures or high-energy trauma, isolated ligamentous damage can occur in sports and daily activities. Injuries to this ligament can significantly affect ankle stability, leading to chronic pain or dysfunction if not accurately diagnosed and managed. Traditional imaging modalities, such as MRI and radiography, provide valuable diagnostic information; however, constraints such as cost, accessibility, and time make it less practical in many rehabilitation settings. Diagnostic MSK ultrasound offers and readily accessible alternative for evaluating ligament integrity. This is important for those who need a time sensitive way to view the anatomy, for example when other diagnostic methods have a long waiting time to get in for assessment.1 It also offers another great benefit of obtaining dynamic testing of ankle stability, as displacement of the medial structures during an eversion stress test is diagnostic of a deltoid ligament injury.2,3 This article aims to provide a comprehensive guide for rehabilitation providers on the use of MSK ultrasound to evaluate the deltoid ligament, emphasizing its advantages, limitations, and clinical application. A recent narrative review of the use of ultrasound for ankle injuries suggests that systematic reviews and meta-analyses report that the pooled sensitivity and specificity of ultrasound are superior to those of the other imaging modalities such as MRI.4 The high sensitivity of ultrasonography in detecting normal deltoid ligament from an injured is 0.90 indicating it is an excellent modality for the medial ankle ligaments.5–7
Anatomy of the Deltoid Ligament
The deltoid ligament, also known as the medial collateral ligament. It is a strong, bi-layered triangular structure on the medial side of the ankle, extending from the medial malleolus to the distal bones of the foot.8 The ligament stabilizes the ankle joint against eversion forces and resists external rotation of the talus. The classic mechanism of injury to the deltoid ligament is forced eversion often in conjunction with lateral malleolar fractures. Another mechanism is due to inversion ankle sprains especially those with cases of chronic ligament ankle instability.4
Superficial Layer – provides a broad support against eversion forces
-
Tibiocalcaneal ligament: Connects the tibia to the calcaneus.
-
Tibionavicular ligament: Extends toward the navicular bone.
-
Posterior superficial tibiotalar ligament: Stabilizes the posterior aspect of the talus.
Deep Layer – primarily stabilizes the talus against medial translation and external rotation
- Anterior tibiotalar ligament and posterior deep tibiotalar ligament form the deep component and are critical for resisting excessive rotational forces.
Understanding the layered structure and function of the deltoid ligament is essential for accurate MSK ultrasound assessment and differentiation of injury severity.
The Role of MSK Ultrasound in Ligament Evaluation
Advantages
-
Real-Time Imaging: Allows dynamic evaluation of ligament integrity while the ankle is moved through its range of motion.
-
High-Resolution Visualization: Provides detailed images of soft tissue structures, including individual components of the deltoid ligament.
-
Accessibility and Cost-Effectiveness: MSK ultrasound is portable, widely available, and less expensive than MRI.
-
Dynamic Stress Testing: Enables direct visualization of ligament elongation or disruption during functional movements.
Limitations
-
Operator Dependency: Requires skill and experience for accurate interpretation of findings.
-
Depth Limitations: Visualization of deeper structures may be less effective compared to MRI.
-
Artifacts and Shadows: Bone and calcifications may create image artifacts, requiring adjustments in probe positioning and frequency.
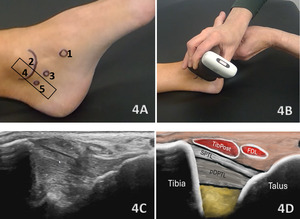
Sonographic Technique for Evaluating the Deltoid Ligament
Equipment Setup
-
Probe Type: A high-frequency linear transducer (7–15 MHz) is recommended for optimal resolution. The probe should be placed along the medial malleolus with adjustments in angulation to capture both superficial and deep ligament components, which includes both anterior and posterior portions of the ligament.
-
Patient Position: The patient is placed supine or lateral decubitus position with the ankle slightly plantarflexed to allow better visualization of medial structures.
-
Dynamic Assessment: Stress maneuvers, such as valgus stress or dorsiflexion, can be applied during MSK ultrasound to reveal ligament instability or disruption.
Examination Protocol
-
Superficial Layer Assessment
-
Begin imaging from the medial malleolus, moving caudally to visualize the tibiocalcaneal and tibionavicular ligaments.
-
Use power Doppler settings to detect hyperemia, indicating inflammation or acute injury.
-
-
Deep Layer Assessment
-
Deep ligaments are evaluated closer to the talus. A gradual examination shifting between static and dynamic imaging modes reveals partial tears or sprains.
-
Look for hypoechoic areas, indicative of edema, or disruptions in the ligament’s fibrillar structure.
-
-
Comparison with Contralateral Ankle
- Evaluate the healthy ankle for baseline comparison, particularly in suspected partial tears.
Normal Sonographic Appearance
The normal deltoid ligament appears as a hyperechoic, fibrillar structure with continuous and well-defined margins within the superficial layer, yet the deep fibers may appear hypoechoic due to their position.9 Additionally, the posterior deltoid appears more hypoechoic with the deeper tibiotalar fibers less well defined than the more superficial anterior deltoid ligaments.10 Dynamic assessment with stress maneuvers can confirm ligament integrity.
Pathologic Findings in Deltoid Ligament Injuries
Acute Sprains
-
Hypoechoic thickening due to edema
-
Disruption of fibrillar pattern
-
Partial or complete ligament tears with discontinuity or retraction
-
Associated joint effusion
Chronic Injury and Insufficiency
-
Ligamentous thinning and hypoechogenicity
-
Periligamentous fibrosis or calcification
-
Dynamic instability with stress maneuvers
Clinical Implications for Rehabilitation Providers
MSK ultrasound provides real-time feedback for rehabilitation professionals, facilitating early diagnosis and intervention. Key applications include:
-
Early Detection of Injury / Accurate Injury Grading: MSK ultrasound can quickly differentiate between a sprain and a more severe ligament tear to help guide treatment planning.
-
Dynamic Functional Testing: Rehabilitation professionals can use MSK ultrasound during physical therapy sessions to monitor recovery and assess ligament function dynamically. Serial MSK ultrasound imaging aids in assessing ligament remodeling and readiness for rehabilitation progression.
-
Guided Interventions: Ultrasound imaging assists in precision-guided injections, such as corticosteroids for inflammation or platelet-rich plasma (PRP) for ligament regeneration.
-
Patient Education: Real-time imaging serves as a visual aid to explain the nature of the injury and set realistic expectations for recovery.
Limitations and Challenges
Despite its advantages, MSK ultrasound cannot entirely replace MRI for complex cases, such as when associated injuries to bony structures or deep intra-articular pathology are suspected. Additionally, the expertise required for optimal imaging technique limits its immediate adoption across all rehabilitation settings.
Conclusion
Diagnostic MSK ultrasound is a valuable tool for the evaluation of the deltoid ligament of the ankle, offering fast, accurate, and cost-efficient imaging for rehabilitation professionals. Its ability to provide real-time, dynamic assessments makes it particularly suited for rehabilitation providers who can integrate the MSK ultrasound findings into clinical decision-making, optimizing treatment strategies and improving patient outcomes. However, practitioners must be adequately trained to maximize it’s diagnostic potential. By integrating MSK ultrasound into practice, rehabilitation providers can enhance patient care, improve outcomes, and reduce the burden of false diagnoses or delayed treatment.

.png)
_and_t.png)
.png)
_and_the_anterior_fibers_of_the_d.png)
_and_the_posterior_fibers.png)

.png)
_and_t.png)

.png)
_and_the_anterior_fibers_of_the_d.png)
_and_the_posterior_fibers.png)