INTRODUCTION
Hamstring strain injuries (HSIs) are the most common injury subtype in male football(soccer) players,1,2 accounting for 12-17% of all time-loss injuries, with incidence and burden increasing year by year.3 HSIs are associated with high financial consequences for clubs, significant time loss for players,4 and have the highest re-injury rate.5 In particular, when the distal musculotendinous T-Junction (DMTJ) is involved, management becomes more difficult and the re-injury rate rises substantially to 54%, as confirmed in previous investigations, due to the complex and variable anatomy of the region.6 Some of these types of injuries require surgical treatment for optimal recovery. The current literature shows high success and a lower re-injury rate.7,8
To date only one case report has been published on the management and return to sport of a professional football player after a hamstring surgery with a semimembranosus reconstruction,9 and there is no research detailing the management and return to sport after surgery on the musculotendinous junction of the biceps femoris, acknowledged as a problematic area for surgeons dealing with probably the most severe hamstring injuries.10 Therefore, the aim of this case report was to describe for the rehabilitation and return to play (RTP) process in a 24 year-old male professional football player with recurrent hamstring injury who was treated with DMTJ surgery and successfully returned to play at the same level of competition after 19 weeks.
CASE DESCRIPTION
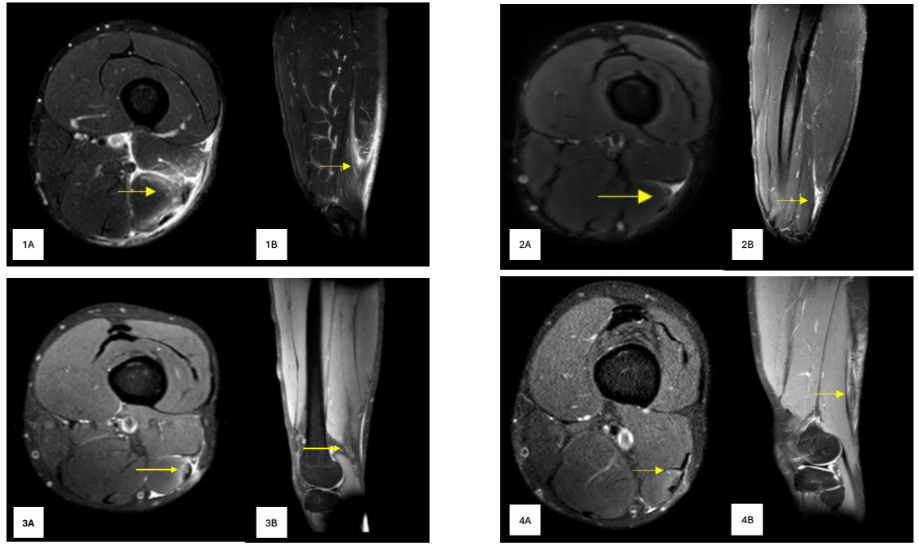
A 24-year-old male football player, playing in the Swiss first division, suffered an HSI during a friendly game while he was running at high speed with concomitant ipsilateral trunk rotation to press a defender waiting to receive the ball during the build-up phase (Supplemental Video 1). The first clinical decision was to undertake conservative treatment, which failed, and he suffered a re-injury in a match eight weeks after his first RTP. In this case, the subject did not report any acute mechanism of injury during the match. Twenty-four hours later the subject reported discomfort around the previous injury area. Following an MRI scan (magnetic resonance imaging, Figure 1) and an assessment by doctors, the orthopedic surgeon suggested a distal surgical repair. No ethics committee in place to provide ethical approval. An informed consent to publish signed by the patient was obtained. Patient confidentiality must be protected according to the U.S. Health Insurance Portability and Accountability Act (HIPPA).
INTERVENTIONS AND OUTCOMES
Decision-making Process and Surgery Description
After seeing the MRI, the surgeon recommended an operation for two main reasons: 1) chronic rupture, small seroma and gap identified at the biceps femoris (BF) T-Junction area with loss of tension of the musculotendinous structure; and 2) recurrent injury and failure of the conservative approach (Figure 1). In addition, given the player’s profile (fast and 1vs.1 player), this kind of injury probably would not have allowed him to perform at his pre-injury level, thus putting his professional career at risk.
General anesthesia was used for the procedure, and antibiotic prophylaxis was used. Through a vertical incision (at the injured area) the biceps femoris muscle was explored. The hamstring fascia was opened and as seen in the MRI, a chronic rupture, small seroma and gap was identified at the BF distal T-junction area. A BF fasciotomy was performed, and the muscle was released from adhesions. First the tendon structure was sutured with absorbable sutures and tendon continuity was restored. The BF T-junction area was reinforced with thin non-absorbable sutures. The tonus of the BF tendon/muscle looked good after the repair was completed, with no active bleeding. The subcutaneous tissue was closed using interrupted sutures, and the skin was closed with non-absorbable sutures. (Figure 2)
Hamstring Rehab Process: A football-centered Model
RTP times and re-injury rates after HSIs are influenced by many factors and the mode of rehabilitation.11 The authors strongly believe in the use of data to support decision-making during the RTP process. On this basis, the described program for rehabilitation and RTP is a football-centered model based on a range of clinical, functional/performance and psychological criteria to determine the player’s progression, with consensual decision-making involving a range of professionals (doctors, physiotherapists and performance coaches). The present model consists of four main phases: I) Regeneration, II) Functional (with several sub-phases), III) Return to Full Training and IV) Return to Play. (Figure 3)
Regeneration Phase
The first phase after the injury was characterized by passive treatments, therapies and mobility exercises, during which only isometric and light concentric contractions of the injured limb were permitted. The goals of this phase were to decrease pain levels, improve mobility, soften the surgery scar and guide the regeneration and remodeling phases through gentle contractions.
During the first two to three weeks the subject was not allowed full weight-bearing on the operated limb and walked using crutches. In this phase, the subject received passive treatments (e.g. manual therapy on the scar, Tecar therapy, electrostimulation) and performed upper body strength training in the gym. The operated limb was used only for submaximal isometric contractions following the surgeon’s recommendations, while the other leg continued with strength training. After the third week, the subject started to progressively increase the isometric hamstring strength training on the injured leg. The volume and intensity were regulated by time and subjective perception based on a percentage (%) of his maximal voluntary contraction (MVC) (e.g. 8 seconds at 50% MVC),12 using both pushing (PIMA) and holding isometric muscle actions (HIMA)13 with the goal of reaching MVC >80% to optimize the tissue regeneration process).14 During this phase, the main criterion for selecting the exercises and progression was pain. If the subject experienced symptoms during the first repetition of an exercise, that exercise was discontinued and was replaced with an alternative. Exercises were selected based on the targeted zone for tension application, beginning with those that focused more on the proximal region of the biceps femoris (BF). This approach allowed us to adjust the tension toward or away from the surgical site as desired, working at lower knee flexion angles or adding a box under the feet. Core and upper body were trained regularly, along with training on the uninjured leg,15 and conditioning/metabolic training. These conditioning sessions included activities such as boxing, battle ropes, air bike, versa climber, and upper body and core metabolic circuits.
From the fifth week, the subject began training in the pool to reduce ground reaction force on the limbs,16 performing mobility exercises, range of movement patterns and running drills aimed at restoring neuromuscular control and coordination in the running gait.17 At the end of this phase, tenderness on palpation, and pain response (measured using the numeric pain rating scale, NPRS) on concentric contraction (without external load) and stretching were minimal or absent (<2/10 NPRS). The interlimb asymmetry in passive (PKE) and active knee extension (AKE) was minimal (<10%) and based on the surgeon’s instructions the biological healing time required before starting strength training was complete (6 weeks)(Supplemental Video 2).
Functional Phase
This phase was split into three sub-phases:
1) Strength and conditioning (S&C) sub-phase: The subject started regular strength training on the back chain in the injured limb, combining isometric, concentric and eccentric exercises through progressive increases in loading and velocity. At this stage the subject was not allowed to run, and the metabolic training was performed using a variety of physical activities (bike, elliptic, air bike, versa climber, boxing, heat training or upper body High Intensity Interval Training (HIT). The strength training continued during the entire rehab and RTP process and when the player was already competing, as a part of his individual training routine for improving performance and minimizing the risk of injury.
The S&C subphase began in the sixth week and the subject progressed through fundamental exercises such as squat, split squat, lunges, hip thrust, Romanian deadlift (RD), and single-leg RD. These exercises were initially performed with a limited range of motion (ROM), using light loads, with a focus on execution, optimal movement control and neuromuscular adaptation. Pain-free execution was used as a criterion for progression and exercise selection. The subject progressively transitioned from hypertrophy-oriented training to maximum strength development using fundamental exercises. In the early stages, hip-dominant exercises that targeted the contractile elements of the proximal region of the biceps femoris long head (BFlh) were prioritized, minimizing recruitment and stress on the distal region of the biceps femoris and, consequently, the distal myotendinous junction (DMTJ).18,19 As training progressed the subject was gradually introduced to knee-dominant exercises, initially using light loads emphasizing slow and controlled eccentric contractions to guide scar remodeling (e.g., leg curl).20 After that, the eccentric overload and speed of execution during knee-dominant exercises progressively increased (e.g., flywheel leg curl, seated leg curl with conic-pulley, see Figure 4), alongside increasing the volume, speed of execution, and loads during the fundamental exercises.
Neuromuscular and lumbopelvic control exercises were performed at least twice a week, as the position of the trunk and the role of the pelvis have been shown to be crucial in the injury mechanism and, consequently, in hamstring injury prevention.21,22 Specific running drills and exercises to improve deceleration ability were also incorporated into the weekly planning. The player continued with upper body strength training twice a week, and three to four times a week a conditioning workout was included at the end of the training (Table 1)(Supplemental Video 3). After two months (at Week 9), a new MRI showed good scar healing, the subject had full mobility compared to the uninjured limb and no pain (<2 NPRS) in any of the exercises performed. Consequently, with the agreement of the surgeon and team doctor, the subject was cleared to start running progressively.
Isometric strength assessment was initially planned every two weeks using the 90 - 90 supine hamstrings test.9 However, due to the subject’s history of cartilage injuries in both knees which caused pain (particularly during resisted knee flexion), and after three tests with very low reliability (due to the pain), we decided not to monitor the subject regularly using this isometric test.
2) Return to Run and Soccer Drills: The subject continued with regular strength training and entered a sub-phase where he was allowed to run progressively at submaximal running speeds, not exceeding 70% of his pre-injury Maximal Sprinting Speed (MSS), also including specific training drills with the ball. External load was always monitored with GPS devices (WIMU, Real Track System S.L.; Calle Guinea, 2. 04009, Almeria, Spain).
This sub-phase was divided into three stages:
a. Return to Running: From continuous running to high intensity running interval training (HIT).
b. Return to Field (individual): Specific exercises with the ball. Progression from more generic drills to more complex tactical exercises. This stage started almost at the same time as the return to running stage
c. Return to Partial Team Training: The subject started to participate partially with the team (usually the first part of the training). The subject progressed from passing exercises to passing drills with shooting in small goals, evolving into combinations with passes, crosses and finishing actions. The progression in exercises with opponents evolved from simple to more complex rondos, rondos with transitions, and then progressed to ball possession games or positional games, participating as an internal floater at first, and then as a normal player.
When the player had successfully trained in stages 2a and 2b, the three stages were superimposed based on availability to participate in team training (this depended on daily approval from the head coach based on the on-field training content). For example: The player started with the team in the gym for 25 min strength training, then he performed the specific warm-up with the team on the field evolving to a passing exercise and then participated as an internal floater during a positional game (4vs4+3). After that, the player continued his individual training with technical-tactical exercises with the ball, combining it with HIT (i.e. 3 min, 10 s running / 10 s passive rest). All exercises were prescribed with the aim that the player should not exceed 60-70% of his MSS.
As an example of a training session within the *2a and 2b stages (*Return to run and return to field (individual)), the subject, after neuromuscular training for tissue preparation in the gym, started training with light jogging around the pitch, reporting good feelings and no pain. After that subject progressed to interval training, started at beginning of 2a stage with a 1:2 work-to-rest ratio, running straight lines at an average speed of 12 km/h. In the second and third week in this sub-phase, the subject tolerated HIT well, reaching an average speed of 20-25 km/h with a 1:1 work-to-rest ratio. At the same time, the subject performed specific exercises with the ball (2b stage). These exercises were aimed at conditioning, as well as working on technical and tactical aspects related to the player’s specific position.
At the beginning of week 12 the subject completed isokinetic tests (5 repetitions of concentric knee flexion/extension and five repetitions of eccentric knee extension at 60°/s) and a Countermovement Jump (CMJ) test on force plates.23,24 The isokinetic test results showed good Limb Symmetry index (%LSI: Injured Limb vs. Uninjured Limb) in eccentric strength (3.8% in mean peak torque and 5.6% in peak torque). There was a substantial %LSI in concentric strength (-19.2% on mean peak torque and -11.8% in total work) (Figure 5). However, due to the subject’s history of cartilage injuries, he reported discomfort/pain in the left knee during the concentric phase of the test, which could have influenced the test results. During the CMJ test, several metrics were analyzed including jump height (cm), concentric mean force (N), takeoff peak force (N), peak landing force (N), landing impulse (Ns) and force at zero velocity (N).9,25The data showed optimal results compared to the pre-injury values (Figure 6). After a positive evolution and progression based on data from player assessments, subjective player feedback, progression in analytic running (HIT) and his performance during the individual football specific drills, the subjectwas ready to start to participate partially with the team (stage 2c) during week 12. From this point the player participated with the team in drills for passes and as an internal floater during rondos. One week later (week 13) the subject began to integrate as a floater in ball possession games and subsequently progressed to becoming a standard player (Supplemental Video 4).
3) Return to High-Speed Running (HSR) & Sprint: The subject progressed within this sub-phase from doses of HSR in a more controlled way to HSR exposure with the ball in specific contexts, evolving to sprint actions (>70%MSS). During this period the player continued to train partially with the team, performing HSR and sprint training in addition to the team training (when he did not receive this training stimulus during his participation with the team). Table 2 shows an example of a weekly plan during this sub-phase of the rehab and return-to-play process. During the organization of the microcycle it was always a priority to achieve as much as involvement as possible with the team, in all activities in which the player would not be exposed to high-risk situations (such as a maximum sprint when the subject was not yet ready to attempt this). During sprint training within this sub-phase, the subject reached a peak speed of ~33 km/h, which was about 94% of his peak speed recorded during matches prior to the injury (Supplemental Video 5).
Return to Full team Training
In this phase the subjectwas allowed to return to on-field unrestricted training with the team.26
At the beginning of week 16 the subject completed another isokinetic test (5 repetitions of concentric knee flexion/extension and 5 repetitions of eccentric knee extension at 60°/s and at 180°/s)27 (Figure 5). The isokinetic testing showed optimal values in concentric and eccentric hamstring strength (mean torque, peak torque and total work), with a side-to-side difference <10% between the injured and uninjured legs. A new MRI was also performed during the week, showing a good healing process (Figure 1). The process to this point has resulted in: 1) good tissue healing; 2) no substantial asymmetries in eccentric hamstrings strength at different velocities; 3) exposures under specific contexts at speeds ~ 95% of MSS; and 4) optimal participation with the team in various football exercises including HSR and sprint activities, all without negative symptoms or discomfort. On the basis on these outcomes, at 16 weeks post-surgery the player was allowed to return to on-field unrestricted training with the team(Online supplemental video 6).
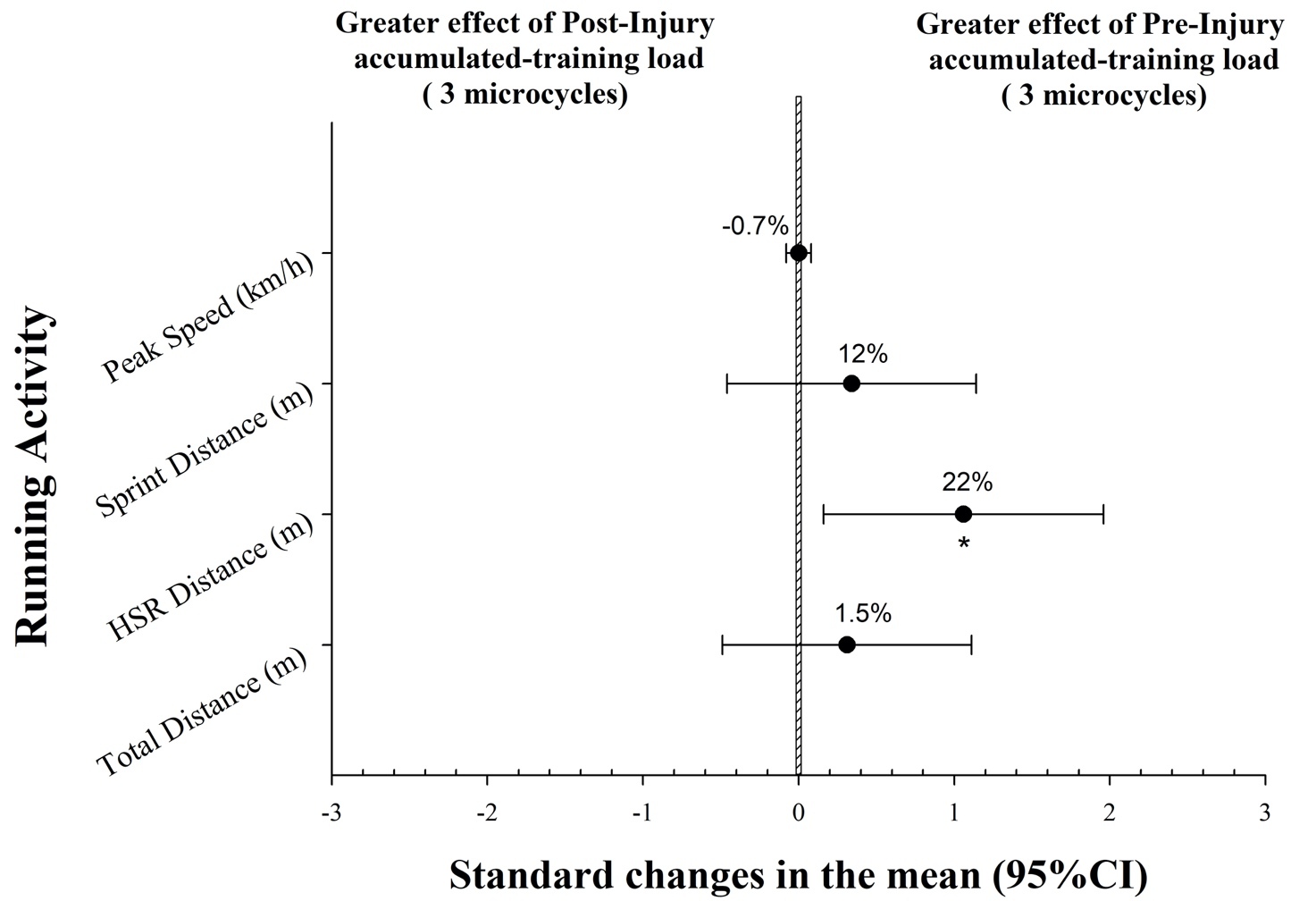
External loadings during three full microcycles were compared with three full microcycles preceding the injury. There were no differences in total distance covered, sprint distance covered (DC > 25 km/h) or peak speed between the accumulated external load during microcycles before and after the injury, while a small difference was detected in the HSR distance covered (DC between 20 – 25 km/h) (Figure 10). HSR and sprint distance covered within each microcycle are shown in Figure 9.
Return to Play
This phase started when the player was declared eligible by medical staff to participate in an official match, independently of whether he was performing at his desired performance level.29
At week 19, after evaluating and analyzing test data, GPS data, wellness data (sleep, muscle soreness and fatigue), RPE data and training videos from the three full team training weeks, a meeting was organized between team doctors, physiotherapists, performance and technical staff, to determine that the subject was ready to be available for an official match. In his first match, he entered as a substitute in the 85th minute, playing for nine minutes. In week 22, he played his first match as a starter and went on to play all 26 remaining matches of the season (totaling 1323 minutes), without experiencing any pain, discomfort, or symptoms at the injury site.
DISCUSSION
The aim of this case report was to describe the rehabilitation and RTP process (based on a football-centered model*)* of a male professional football player with recurrent hamstring injury treated with DMTJ surgery. This case report provides a detailed description of a real-life application and successful RTP journey for a professional football player, combining objective data in conjunction with clinical expertise and player feedback utilized for decision making on loading progressions. The journey through the process ranged from the moment at which the player suffered the injury, the subsequent decision to have surgery, and continued through the different phases of the rehab and RTP process up to the point at which the player participated in his first post-surgery match.
Comparing this report with similar clinical cases in the scientific literature is difficult, as there is no published research reporting the rehabilitation and RTP process for this type of injury in a professional soccer player. Furthermore, although criteria-based rehabilitation progressions have grown in popularity in recent years,30–35 there is no consensus in the literature on how RTP after HSI should be conducted, and RTP decision making after HSI lacks standardization and clear criteria.36 Despite recent interest, specific criteria for progressing through the stages of HSI rehabilitation have not been examined rigorously and a recent systematic review reported that RTP criteria for HSI have little evidence to support them.36 Some of these criteria-based rehabilitation progressions are based on closed criteria that allow the subject to advance from phase to phase.31 Although these protocols are of interest for understanding and helping practitioners during RTP management, relying exclusively on predetermined criteria to decide whether a subject can advance in the process could limit and slow down the RTP process. In addition, to date only one similar case report has been published describing the management and return to sport of a professional football player after hamstring surgery, although in this case following a semimembranosus reconstruction.9
The present study showed that after recurrent injury with a chronic rupture (small seroma and gap identified at the BF T-Junction area with loss of tension of the musculotendinous structure) a surgical repair was required (Figure 1). Taberner et al.9 reported in their study that after a high-grade semimembranosus proximal free tendon retracted tear in a professional soccer player, an orthopedic surgeon recommended an operative approach. In both cases, conservative treatment was dismissed due to the high risk of re-injury and negative consequences for an elite professional football player’s career.
The proposed rehabilitation program and RTP was a football-centered model based on a range of clinical, functional / performance and psychological criteria to determine the subjetc’s progression. The progression was divided into four main and differentiated phases: regeneration, functional with several sub-phases, return to full training, and return to play (Figure 3). The process was football- and player-centered, based on individual player characteristics, the player’s locomotor profile and specific position on the field and his tactical requirements. This meant that whenever possible the subject trained with the ball, performing what was allowed in terms of locomotive activity and high-intensity actions (i.e. kicking) based on the condition of the injured tissue. The main difference in our model is that the subject started training with the ball practically at the same time he started running. Previous research has shown that running <60-70% of MSS has a moderate-low impact and activation of BF, resulting in minimal stress, minimal overstretch, and consequently a low risk of re-injury.37,38There are many exercises in football that can be performed without exceeding 60-70% of MSS, especially when prescribed to a fast subject (MSS = ~ 36 km/h). Therefore, if the risk is controlled, incorporating soccer drills into rehab as early as possible could be a game-changer in the RTP process promoting specific neurocognitive readaptation and substantially increasing player motivation and attitude towards the proposed exercises, enhancing psychological well-being.
Strength assessments during the rehab and RTP process are commonly used to evaluate tissue condition and force levels.11 As previously mentioned, due to the subject’s history of cartilage injuries in both knees, which caused pain during isometric testing, the authors decided not to monitor the subject regularly using this test. Eccentric hamstring strength is believed to be an important criterion for determining when a player is ready for RTP after HSI.39 In this case it was decided that the best option was to unilaterally assess the eccentric hamstring strength using isokinetic testing at different velocities, as isokinetic testing is one of the most widely used tests in soccer40 and is extensively employed as a criterion for RTP in sport after HIS, comparing the injured vs the uninjured legs. Similarly, CMJ is the most common test of lower body muscular power in the scientific literature relating to football players.41 Similar to Taberner et al.,9 CMJ testing using force platforms was used to evaluate the lower body neuromuscular profile during the RTP process via several metrics proposed in previous research,25 with pre-injury levels as reference points (bilaterally and unilaterally).
External training load on the field was regularly monitored using GPS devices. HSR and sprinting distance covered have increased in recent years in professional football and are among the main causes of HSIs.42 Therefore, monitoring these metrics to objectively ensure that the player was progressively adapting to the demands of competition was a priority during the RTP process. Previous research suggests that HSIs often occur at high speeds but not necessarily at the absolute peak speed43; therefore it was a primary concern to expose the subject to a wide range of locomotor activities at high speeds in specific contexts that he would later experience during matches. Running activity during three microcycles prior to the injury was taken as a benchmark (from MD-4 to MD-1, both included) of weekly external load to prepare the player for the match, and compared to his post-injury external load data, to determine that the player was coping with the demands of training without fatigue and muscle soreness (wellness test).
CONCLUSION
The rehabilitation and RTP process based on a football-centered model of a male professional football player with recurrent hamstring injury treated with DMTJ surgery was described in the present study. This was based on a range of clinical, functional/performance and psychological criteria to determine the player’s progression, with consensual decision-making involving a range of professionals (doctors, physiotherapists and performance coaches). The subject gradually returned to team training after 12 weeks and successfully returned to play after 19 weeks. The player participated in 26 official matches throughout the season, accumulating 1.323 minutes of play without reporting any symptoms at the injury site.
Supplementary material
Supplemental videos about this article can be accessed online link
ACKNOWLEDGEMENTS
We would like to thank everyone involved in the day-to-day work of the RTP process: Fabio Soria Guerra, Borja Jover, Vittorio Bruni Prenestino, Tommaso Bosaglia and Marco Valcarenghi. Special thanks go to Marco Carletta for assistance with creating the figures and to Gianpaolo Ermolli for producing the videos. Finally, we would like to extend our gratitude to Luca Vergani and Aleksi Jokela for their valuable suggestions on the draft writing.
Corresponding author
Massimo Zanovello, Tel:+393496779209,
email: massimo.zanovello@fclugano.com; massimozanovello4@gmail.com
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data presented in this study are available on request from the corresponding author.






_tests_at_three_different_timepoints.png)

_and_sprint_distance_(dist.png)






_tests_at_three_different_timepoints.png)

_and_sprint_distance_(dist.png)