Introduction
The most common median nerve injury in the wrist is carpal tunnel syndrome (CTS).1,2 This entrapment neuropathy develops as the median nerve is contained within a relatively inflexible carpel tunnel. Increased compartmental pressures lead to local nerve ischemia, releasing inflammatory factors that cause edema, leading to further increased compression.3 Symptoms of CTS include nocturnal paresthesia involving the thumb, index, middle and radial half of the ring finger with sparing of the thenar eminence, progressing to daytime symptoms and eventual atrophy of the thenar eminence.4
Anatomy of the Median Nerve
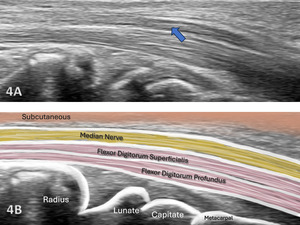
The median nerve begins as the extension of the medial and lateral cords of the brachial plexus in the axillary region. It descends in the arm lateral to the brachial artery until the insertion of the coracobrachialis, where it crosses in front, and in rare cases, behind the artery to move to the medial side of the arm near the anterior cubital fossa. At that location, it runs behind the lacertus fibrosus and is separated from the joint by the brachialis muscle. The median nerve received its name from the middle position at the end of the brachial plexus and the forearm.5 As it descends further in the forearm, it runs between the two heads of the pronator teres. From that point it runs beneath the flexor digitorum, laying on the flexor digitorum profundus more superficially as it passes underneath the transverse carpal ligament (flexor retinaculum) into the palm. At the hand, the median nerve gives motor branches to the thenar eminence, and second lumbrical muscles, as well as sensory branches to the radial half of the palm and the radial three and half digits.6 Its motor function is to the flexor aspect of the forearm, hand, and thumb to innervate the pronator teres, palmaris longus, flexor digitorum superficialis, flexor carpi radialis, and via the anterior interosseus nerve (AIN), the flexor pollicis longus, the flexor digitorum profundus, and the pronator quadratus.
Understanding the structure and innervation of the median nerve is essential for accurate MSK ultrasound assessment and differentiation of injury type and severity.
The Role of MSK Ultrasound in Nerve Evaluation
Advantages
-
Real-Time Imaging: Allows dynamic evaluation of median nerve integrity while the wrist and forearm are moved through available range of motion.
-
High-Resolution Visualization: Provides detailed images of soft tissue structures, including individual nerves in the forearm and wrist.
-
Accessibility and Cost-Effectiveness: MSK ultrasound is portable, widely available, and less expensive than MRI.
-
Dynamic Stress Testing: Enables direct visualization of nerve mobilization, thickening, or disruption during functional movements.
Limitations
-
Operator Dependency: Requires skill and experience for accurate interpretation of findings. The ability to sonograph peripheral nerves is to a large extend influenced by the operator and the availability and technical considerations of state-of-the-art equipment.7
-
Depth Limitations: Visualization of deeper structures may be less effective compared to MRI.
-
Artifacts and Shadows: Bone and calcifications may create image artifacts, requiring adjustments in probe positioning and frequency.
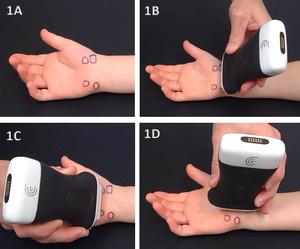
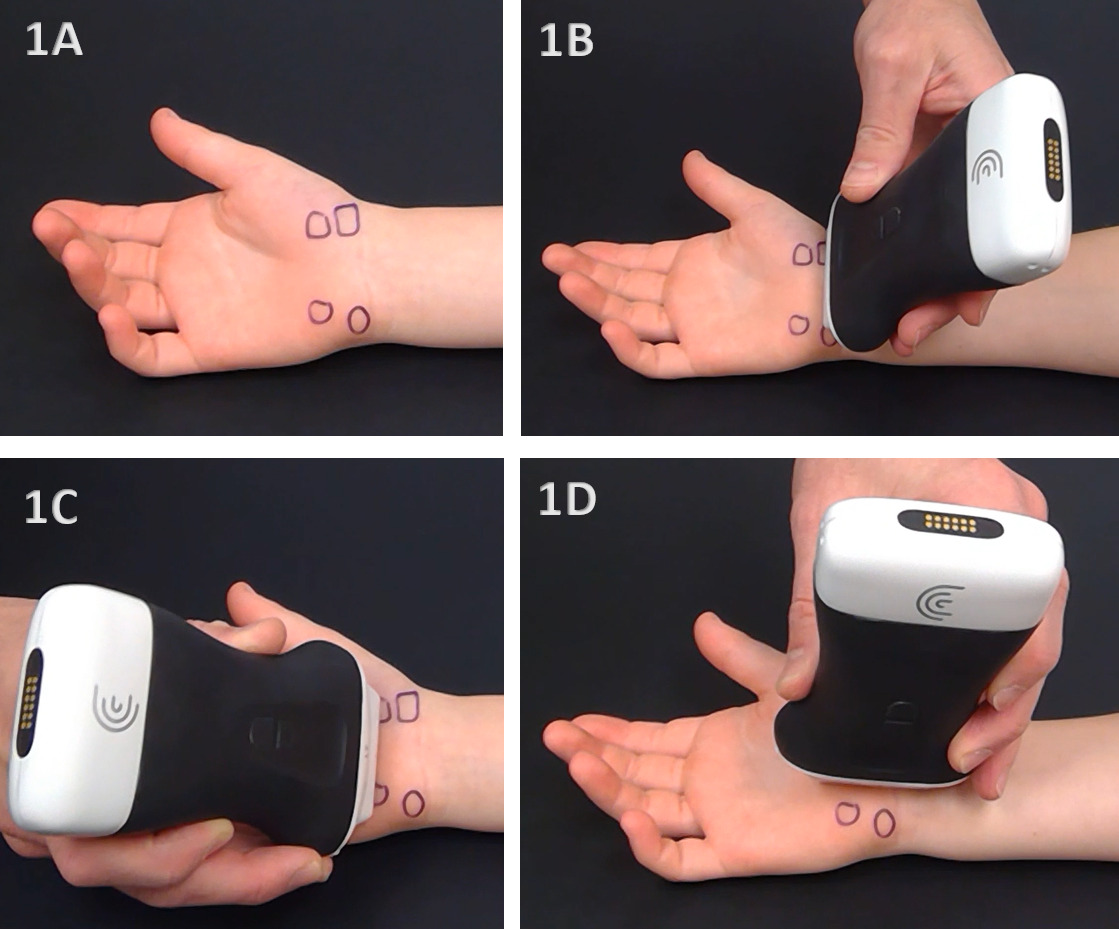
Sonographic Technique for Evaluating the Median Nerve
Equipment Setup
-
Probe Type: Because of the superficial nature of the median nerve at the wrist, a high-frequency, linear array transducer is normally used.8
-
Patient Position: The patient is seated on the opposite side of the table near the edge to be closer to the examiner. The hand is supinated and neutral with the wrist and fingers in minimal flexion. The probe is placed in either the transverse short axis (SAX) or longitudinal axis (LAX) near the crease of the palmar wrist.
-
Dynamic Assessment: Stress maneuvers, such as elbow and wrist flexion and extension, as well as forearm supination and pronation, can be applied during MSK ultrasound to reveal nerve instability, as well as hyper- or hypo-mobility.
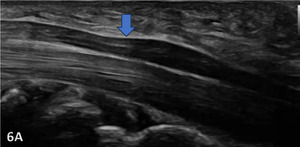
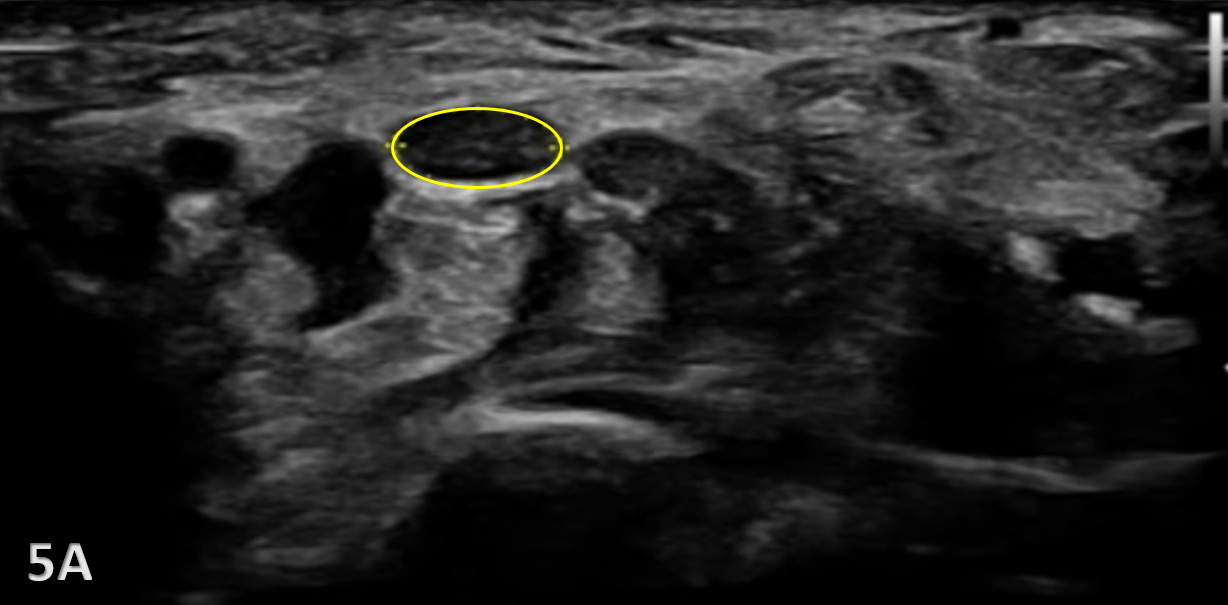
Normal Sonographic Appearance
The median nerve is clearly identifiable in SAX by a well circumscribed ovoid structure with hypoechoic fascicles in a honeycomb-like pattern deep to the roof of the carpal tunnel, the flexor retinaculum, and more superficial to the flexor digitorum superficialis and flexor digitorum profundus tendons. The median nerve is also very compressible and will alter its shape depending on the volume of the anatomical spaces with which it courses. The median nerve cross-sectional area (CSA) can be measured in four sites: 1) the proximal border of the pronator quadratus muscle, 2) proximal to the carpal tunnel inlet, 3) at the tunnel inlet, and 4) at the tunnel outlet.9
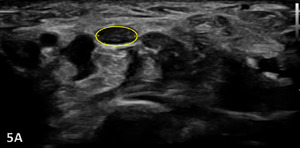
Pathological Findings in Median Nerve Pathology at Wrist
A maximal CSA of 12 mm2 or greater at any location is typically diagnostic for CTS.6 More recent evidence shows that CSA may vary based on subgroupings including age, sex, ethnicity, geographical location, and method of CSA assessment.10 An increase in size greater than 2 mm comparing proximal (at pronator quadratus) to distal (at wrist crease) can diagnose carpal tunnel syndrome with 99% accuracy.11
Carpal Tunnel Syndrome can be identified by the following images:
-
Hypoechoic thickening due to swelling and edema
-
Disruption of fibrillar pattern
-
Associated joint effusion
Clinical Implications for Rehabilitation Providers
MSK ultrasound provides real-time feedback for rehabilitation professionals, facilitating early diagnosis and intervention. Key applications include:
-
Early Detection of Injury / Accurate Injury Grading: MSK ultrasound can quickly differentiate between a sprain and a more severe ligament tear to help guide treatment planning.
-
Dynamic Functional Testing: Rehabilitation professionals can use MSK ultrasound during physical therapy sessions to monitor recovery and assess ligament function dynamically. Serial MSK ultrasound imaging aids in assessing ligament remodeling and readiness for rehabilitation progression.
-
Guided Interventions: Ultrasound imaging assists in precision-guided dry needling or injections, such as corticosteroids for inflammation.
-
Patient Education: Real-time imaging serves as a visual aid to explain the nature of the injury and set realistic expectations for recovery.
Limitations and Challenges
Despite its advantages, MSK ultrasound cannot entirely replace MRI and NCS for complex cases. Additionally, the expertise required for optimal imaging technique limits its immediate adoption across all rehabilitation settings.
Conclusion
Diagnostic MSK ultrasound is a valuable tool for the evaluation of the median nerve at the wrist, offering fast, accurate, and cost-efficient imaging for rehabilitation professionals. Its ability to provide real-time, dynamic assessments makes it particularly suited for rehabilitation providers who can integrate the MSK ultrasound findings into clinical decision-making, optimizing treatment strategies and improving patient outcomes. However, practitioners must be adequately trained to maximize its diagnostic potential. By integrating MSK ultrasound into practice, rehabilitation providers can enhance patient care, improve outcomes, and reduce the burden of false diagnoses or delayed treatment.