Introduction
Deceleration performance is an essential indicator of athletic talent and sport performance.1 Defined as a sporting action that precedes a change of direction2 or an action immediately following a sprint to reduce momentum,3 decelerations occur frequently during competition. High speed decelerations occur more frequently than accelerations, with soccer athletes performing 40-62 decelerations (5-7% of total player load) per match.4 Due to the high impact forces and loading rates that occur during a deceleration, it is a common mechanism for non-contact knee or anterior cruciate ligament (ACL) injury and also associated with elevated markers for muscle damage5,6 Because pressing or sudden decelerations performed close to an opponent have been identified as common injury mechanisms, it has been suggested that deceleration training may serve as a “vaccine”7 or “missing link”8 for reducing injury risk. Despite this, little is known about the relationship between quadriceps function and deceleration performance.
Deceleration places a high demand on the quadriceps with activation exceeding 161% of the maximum voluntary isometric contraction (MVIC) during a deceleration task.9 Angular velocities at the knee have been reported to be 493 ± 252°/s7,10 during decelerations, indicating that high levels of quadriceps activation and eccentric strength are required to safely control the knee joint. Specific to the athletic population, a single leg landing from a running stop results in a higher peak ACL force (1294 N) than any other open or closed chain task.11 Additionally, a higher rate of deceleration results in higher ACL loading.11,12 Functional testing batteries are often utilized to assess an athlete’s readiness to return to sport following ACL reconstruction, with a bulk of tests focusing on quadriceps strength, single leg squat performance, and horizontal hop testing. Recent evidence suggests that functional testing and horizontal/forward hop distance may over-estimate function, with patients achieving >90% limb symmetry indices (LSI) during hop testing despite having significant quadriceps deficits via isokinetic testing.13,14 As the quadriceps are under greatest demand during deceleration, the authors believe that examining deceleration performance may expose any underlying quadriceps deficit and serve as an appropriate surrogate when isokinetic or instrumented isometric testing is not available.
Current examples of deceleration testing heavily rely on technology (3-dimensional video analysis, force plates, etc.) and utilize a change of direction (COD) maneuver performed at shallow angles from 30-90°.5,15 Subjective scales such as the Cutting Movement Assessment Score (CMAS)15 have been utilized to examine COD performance and provide insight into technique, faulty patterns, and potential injury risk. The use of a deceleration index8 and deceleration deficit16 testing have also been suggested as assessment methods. Though promising, there is a lack of deceleration testing in athletic populations, especially at angles >90° where harder braking occurs, and vertical ground reaction forces rise. Therefore, the authors suggest two deceleration tests that can be performed without significant technology that may provide additional insight into quadriceps function: the deceleration task and the single leg retro hop.
The deceleration task involves a 10m sprint followed by a 135° COD and sprint to a cone 5m away (Figure 1). The patient is timed and subjective scales such as the CMAS can be utilized to provide insight into deceleration performance. The task is performed in both directions. The authors believe that this task places a high demand on the quadriceps and patients with large quadriceps deficits may likely compensate or demonstrate errors at the penultimate and/or final foot contacts. Biomechanical assessments of knee flexion angle, trunk flexion angle, and the presence of dynamic knee valgus can be performed.
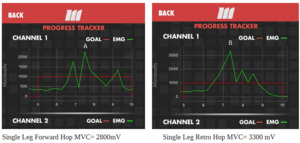
To perform the single leg retro hop, a marker is placed 24 inches in front of the athlete for the initial landing distance. [Of note, allometric scaling for placement of the marker is currently being explored by the authors]. The patient stands on the involved leg and jumps to the initial landing area. After landing, the patient immediately hops backwards with maximum effort, hopping as far as possible (Figure 2). The patient must “stick” the landing and hold it for three seconds. During the backwards hop, the goal is for the patient to achieve > 90° knee flexion if possible in order to ensure utilization of the quadriceps and eliminate compensatory strategies (stiff landings, over-reliance on hip or trunk landing strategies, etc.). The retro hop distance is measured from the initial landing position to the final landing position (heel to toe). Three trials are performed on each limb and averaged to identify the LSI . Surface electromyography (sEMG) may also be utilized during this task to quantify quadriceps muscle activity during the deceleration (Figure 3).
Figure 3 demonstrates an example of quadriceps sEMG activity during forward and retro hopping in an athlete nearing return to sport following ACL reconstruction. This patient demonstrated a peak sEMG of 3300 microvlts during retro hopping compared to 2800 microvolts with forward hopping. This indicates that retro hopping may require greater quadriceps sEMG activity than forward hopping. It is also noted that during the single leg forward hop the peak sEMG occurs upon landing (not take off), demonstrating that the quadriceps is more active during the deceleration (eccentric) phase. Further studies are needed to validate if retro hopping will correlate more closely with LSI quadriceps deficits versus traditional forward hopping tests.
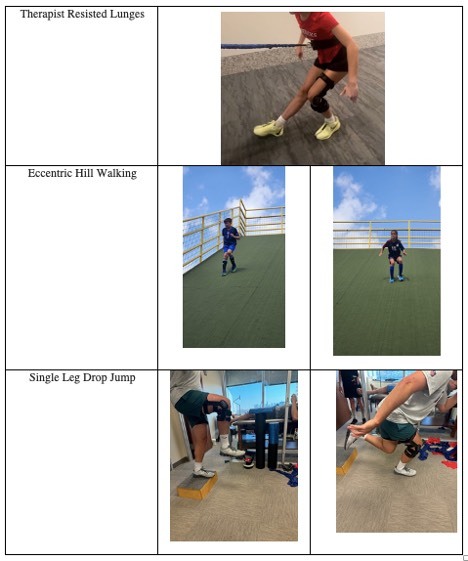
Both of these assessments may provide insight into quadriceps function during later stages of rehabilitation. Future validation and reliability studies are needed to ensure their clinical utility and identify their potential role in testing batteries. Eccentric exercises may help prepare athletes to handle the demands of deceleration when returning to sporting activities. Inclusion of deceleration activities during rehabilitation is helpful in preparing the injured athlete for sporting activities and testing. The following are examples of exercises that may be implemented during the rehabilitation process to induce eccentrics and deceleration: standing forward drop lunges, Sportcord retro walking, single leg drop jump, lateral/forward step downs, therapist resisted lunges activities (deceleration stops), hill walking eccentric descents and serpentines, and reverse lunges using sliders (multi-directional) (Figure 4).
Conclusion
Traditional functional testing often over-estimates quadriceps strength and does not expose athletes to the high eccentric quadriceps demands required for deceleration. The example described above demonstrated the increased quadriceps sEMG during a retro hop compared to forward hopping. Further studies are needed to determine if the retro hop and deceleration task performance correlate to or are predictive of quadriceps deficits in the involved extremity. Clinicians should consider the relationship between deceleration and quadriceps function when assessing athletes and leverage that relationship during the rehabilitation process to better prepare athletes to return to sport.
Corresponding Author
Steven Higbie, PT, DPT, SCS, CSCS, Memorial Hermann Rockets Sports Medicine Institute, Department of Sports Medicine & Rehabilitation, Houston, TX, 77030, USA; steven.higbie@memorialhermann.org
Conflicts of Interest
Dr. Higbie, Dr. Gallina, and Dr. Bailey report no conflicts of interest. Russ Paine has a financial relationship with MTrigger Biofeedback as a co-founder and clinical advisor, which is described within this manuscript.