Introduction
Elbow injuries are very common in athletics that require overhead motions.1 Although less commonly injured than its anterior counterpart, the biceps tendon, posterior distal triceps tendon injuries account for 1% of all tendon injuries in the upper extremity. These injuries usually affect males between 30 and 60 years old.2–4 Injuries to the triceps tendon include tendinopathy, partial tears, complete ruptures, and bony injury. High repetition, lower load activities usually lead to tendinopathy issues, while high-intensity trauma in contact sports such as football or in the active military population result in partial tears or rupture of the triceps tendon.5 Ruptures most commonly occur in the tendon insertion area compared to muscle-tendon junction or muscle belly6–9; the mechanism of injury is usually a fall on an extended elbow.
Although magnetic resonance imaging (MRI) is used due to its excellent soft tissue contrast, musculoskeletal ultrasound (MSK ultrasound) has been shown to be a very effective modality to examine tendon injury. Symptoms of triceps injury include pain, swelling, discoloration, and loss of active range of motion and strength. Partial thickness tears tend to selectively involve the superficial layer of the tendon, leaving the deeper layer intact.10 This can be misleading because a patient with a significant tendon tear may be able to generate elbow extension force during manual muscle testing.11 It is very important to detect the extent of the injury as patients with complete ruptures or partial ruptures of more than 50% are candidates for operative repair, whereas the others are treated with conservative care.12 Several case studies utilizing ultrasonography of triceps tendon injury are available in the literature.13–18
Anatomy of the Triceps Tendon
Understanding the structure and innervation of the triceps tendon is essential for accurate MSK ultrasound assessment and differentiation of injury type and severity. The triceps brachii forms a common tendon that inserts onto the olecranon. However, anatomical descriptions remain somewhat controversial whether two or three heads (medial, lateral and long heads) contribute to the common tendon.2,19–23 The long head origin is the infraglenoid tubercle of the scapula, the medial head originates on the posterior humerus proximal to the radial groove and lateral intermuscular septum, and the lateral head originates on the posterior humerus proximal to the radial groove and the lateral intermuscular septum. The three heads share a common insertion on the olecranon of the ulna along the radial surface. The action of the triceps is extension of the elbow, while the long head also extends and adducts the shoulder joint due to its origin on the infraglenoid tubercle of the scapula.
The Role of MSK ultrasound in Tendon Evaluation
Advantages
-
Real-Time Imaging: Allows dynamic evaluation of tendon and muscle integrity while the elbow can be moved through available range of motion.
-
High-Resolution Visualization: Provides detailed images of soft tissue structures, including the triceps muscle, tendon, and its enthesis at the olecranon process.
-
Accessibility and Cost-Effectiveness: MSK ultrasound is portable, widely available, and less expensive than MRI.
Limitations
-
Operator Dependency: Requires skill and experience for accurate interpretation of findings. The ability to sonograph tendons is influenced by the operator as well as the availability and technical considerations of state-of-the-art equipment.
-
Depth Limitations: Visualization of deeper structures may be less effective compared to MRI, particularly if the tendon is shielded by bone.
-
Artifacts and Shadows: Bone and calcifications may create image artifacts, requiring adjustments in probe positioning and frequency.
Sonographic Technique for Evaluating Triceps Tendon and Muscle
Equipment Setup
-
Transducer Type: Because of the superficial nature of the triceps tendon, a high-frequency, linear array transducer is normally used.
-
Patient Position: The patient can be seated upright or lying down supine. In the supine position, the patient’s shoulder is kept in a neutral position with the elbow flexed to approximately 90 degrees, and the forearm is pronated with the palm resting flat on the examination table. (See Figure 1)
-
Dynamic Assessment: Stress maneuvers, such as elbow and wrist flexion and extension, as well as forearm supination and pronation, can be applied during MSK ultrasound to reveal nerve instability, hyper- or hypomobility.
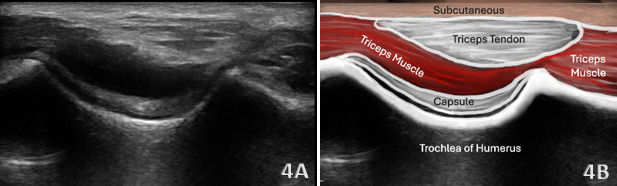
Normal Sonographic Appearance
Typically, the triceps tendon will be viewed in both the long axis (LAX) and the short axis (SAX). In the LAX view one should start distally to visualize the hyperechoic reflection of the humeral cortex. Proximal to the cortex one should visualize the hypoechoic medial triceps muscle, which is deep to the hyperechoic, fibrillar echotexture of the triceps tendon as it tapers toward the olecranon. In the SAX view, the image should be a non-uniform mixture of muscle, tendon and bone. In this view, the depression-like hyperechoic area is the olecranon process. The triceps muscle will be viewed as hypoechoic tissue, while the triceps tendon will be more hyperechoic in appearance. Maneuvering the transducer will help reduce anisotropy in this region.
Pathologic Findings in Triceps Tendon Injury
Triceps tendon pathology presents as most common tendinopathies do under ultrasound:
-
Hypoechoic thickening due to tendon swelling and edema
-
Disruption of fibrillar pattern in partial tears and ruptures
-
Associated joint effusion
-
Calcifications near the enthesis site
Clinical Implications for Rehabilitation Providers
MSK ultrasound provides real-time feedback for rehabilitation professionals, facilitating early diagnosis and intervention. Key applications include:
-
Early Detection of Injury / Accurate Injury Grading: MSK ultrasound can quickly differentiate between a strain and a more severe rupture to help guide treatment planning.
-
Dynamic Functional Testing: Rehabilitation professionals can use MSK ultrasound during physical therapy sessions to monitor recovery and assess tendon function dynamically. Serial ultrasound imaging aids in assessing tissue remodeling and readiness for rehabilitation progression.
-
Guided Interventions: Ultrasound imaging assists in dry needling and precision-guided injections, such as corticosteroids for inflammation.
-
Patient Education: Real-time imaging serves as a visual aid to explain the nature of the injury and set realistic expectations for recovery.
Limitations and Challenges
Despite its advantages, MSK ultrasound cannot entirely replace MRI for complex cases. Additionally, the expertise required for optimal imaging technique limits its immediate adoption across all rehabilitation settings.
CONCLUSION
Diagnostic MSK ultrasound is a valuable tool for the evaluation of the triceps tendon at the elbow, offering fast, accurate, and cost-efficient imaging for rehabilitation professionals. Its ability to provide real-time, dynamic assessments makes it particularly suited for rehabilitation providers who can integrate the MSK ultrasound findings into clinical decision-making, optimizing treatment strategies and improving patient outcomes. However, practitioners must be adequately trained to maximize its diagnostic potential. By integrating MSK ultrasound into practice, rehabilitation providers can enhance patient care, improve outcomes, and reduce the burden of false diagnoses or delayed treatment.
The patient can be seated upright on a stool or chair or lying down supine, as shown above in Figures 1A-1C. In the supine position, the patient’s shoulder is kept in a neutral position with the elbow flexed to approximately 90 degrees, and the forearm is pronated with the palm resting flat on the examination table. Ensure the arm is relaxed and supported to minimize muscle activation during imaging.
Figure 1A: Transducer Placement on Triceps Tendon Mid-Portion in Long Axis (LAX)
For the long axis view, place the transducer into a longitudinal orientation along the posterior aspect of the elbow, aligning it with the shaft of the humerus and the olecranon.
Figure 1B: Transducer Placement on Triceps Tendon Insertion in Long Axis (LAX)
As the transducer is moved distally, continue to follow the triceps tendon down to its insertion on the olecranon to obtain a clear view of the enthesis. Using a generous amount of gel or a standoff pad is helpful in this region to optimize acoustic contact and reduce near-field artifacts. Note how the transducer must be tilted. This angulation is essential to align with the distal tendon fibers and reduce anisotropy, which is common if the transducer is held too flat. Maintain light transducer pressure to avoid compressing superficial structures. Sweep medially to laterally across the tendon insertion to evaluate the full width of the enthesis.
Figure 1C: Transducer Placement on Triceps Tendon in Short Axis (SAX)
Position the transducer in a transverse plane over the posterior elbow, aligned perpendicular to the triceps tendon and muscle fiber orientation. Place the transducer just proximal to the olecranon process to visualize the triceps tendon in cross-section. Regularly toggle the transducer to maintain perpendicular insonation, which helps preserve the tendon’s hyperechoic appearance and reduces anisotropy.
Refer to Figure 1A for the transducer position for this image. Ensure the ultrasound depth is properly adjusted to visualize the deep structures of the posterior elbow. Begin with the transducer aligned parallel to the long axis of the humerus, centered over the distal posterior aspect of the elbow. Identify the hyperechoic cortical surface of the humerus, with the triceps muscle belly and its myotendinous junction visible more superficially. Scanning distally, a concavity in the bone will become apparent. This is the olecranon fossa, which houses the posterior fat pad. The fat pad appears hyperechoic and lies deep to the joint capsule, within the posterior joint recess. Appreciate the joint space between the olecranon and either the trochlea (medially) or the capitellum (laterally); this is the primary site where joint effusions will first accumulate. The olecranon process of the ulna is seen inserting into this fossa, with the distal triceps tendon inserting onto its posterior surface. The trochlea appears as a curved, hyperechoic contour, typically covered by a layer of anechoic or hypoechoic cartilage. Use small medial-to-lateral sweeps with the transducer to evaluate the full extent of the posterior joint recess. Carefully assess for signs of pathology, including joint effusion, synovial hypertrophy, cortical erosion, intra-articular loose bodies, or fracture. Suspected fractures may present as cortical irregularities, discontinuities, or step-off deformities. If a suspicious area is identified in long axis, rotate the transducer 90 degrees to confirm findings in SAX and improve diagnostic confidence.
Refer to Figure 1B for the transducer position for this image. Perform a slight distal LAX slide along the posterior elbow, curving around the bend of the joint to visualize the characteristic “bird’s beak” appearance of the distal triceps tendon as it inserts onto the olecranon process. Apply ample ultrasound gel and utilize a heel-to-toe maneuver to optimize contact with the skin surface. Tilting the transducer is essential to reduce anisotropy and enhance visualization of the fibrillar tendon structure. Perform small medial and lateral sweeps to assess the full width and insertional footprint of the distal triceps tendon. Carefully evaluate for sonographic signs of enthesopathy, including tendon thickening, hypoechoic changes, loss of fibrillar architecture, partial or full thickness tearing, and cortical irregularity or avulsion at the bony interface. Slightly extending the elbow can help relieve excessive tension on the tendon, which may otherwise obscure power doppler signals. The presence of power Doppler activity at the insertion may indicate active enthesitis or inflammatory changes at the enthesis.
Refer to Figure 1C for the transducer position for this image. Begin the transverse (short axis) assessment of the triceps tendon proximally at the mid to distal humerus. In this region, the triceps muscle belly is visible as a heterogeneous structure with mixed echogenicity, consistent with normal muscle architecture. As the scan progresses distally, observe how the muscle fibers converge into the triceps tendon, which appears as a hyperechoic, fibrillar structure inserting onto the posterior olecranon. The tendon becomes more compact and echogenic near its insertion. Anisotropy can assist in confirming tendon identity—subtle transducer tilting will cause the tendon to fade in and out of view, helping differentiate it from adjacent structures. Continuing the sweep distally, you will encounter the olecranon fossa, identifiable by its distinct U-shaped contour. This space normally houses a hyperechoic fat pad, which fills the fossa in the absence of pathology. In cases of joint effusion or synovitis, this fat pad may be elevated or displaced, and anechoic to hypoechoic fluid may become visible within the fossa. Further distal scanning reveals the olecranon process, deep to the tendon. The bony cortex of the olecranon should appear as a smooth, continuous hyperechoic line with posterior shadowing. A thin, anechoic layer of articular cartilage may also be appreciated lining the olecranon surface under normal conditions.
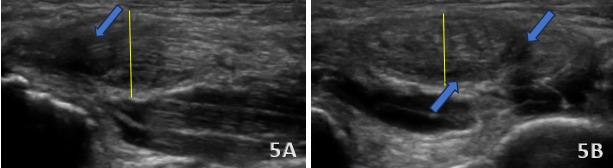
These two figures show a partial tear of the distal triceps brachii tendon (blue arrows). These tears typically present with a focal hypoechoic or anechoic area within the tendon, representing disrupted or absent tendon fibers. In a partial tear, some degree of fiber continuity remains, distinguishing it from a complete rupture. The long head may show localized fiber retraction or irregularity but with bridging fibers still visible across the tear site. In this case, shown above in Figures 5A and 5B, the tendon demonstrates diffuse thickening (yellow lines) and heterogeneous echotexture, consistent with chronic tendinosis. This often appears as hypoechoic areas interspersed with hyperechoic foci due to degenerative changes, mucoid degeneration, and possible calcifications. The tendon margins may appear poorly defined, and power Doppler imaging may reveal increased vascularity, indicating chronic inflammation or reactive hyperemia.
In the short axis view of the distal triceps tendon, synovitis (blue arrows) presents as hypoechoic or anechoic joint effusion surrounding the distal triceps tendon fibers within the posterior elbow recess. Observable synovial thickening appears irregular, hypoechoic tissue and increased doppler signal indicating active synovial inflammation. The triceps tendon appears mildly displaced or effaced by adjacent fluid but retains normal fibrillar architecture. Olecranon bursitis (yellow line) is identified as a fluid-filled distension of the olecranon bursa, located superficial to the distal triceps tendon and olecranon process. The bursa may appear anechoic in simple cases.

.png)





.png)