INTRODUCTION
Cervical intervertebral disc (IVD) hydration status changes under loaded and unloaded conditions resulting in normal IVD fluid fluctuations.1,2 The fluctuations lead to IVD height changes and occur with various positions and activities throughout the day.3–5 These IVD height changes are due to differences in osmotic and hydrostatic pressure that facilitate fluid and metabolites to flow either into or out of the IVD.6 As the IVD experiences external hydrostatic pressures forcing water out, IVD height decreases. Conversely, when hydrostatic pressure is removed the osmotic pressure gradient draws water in and IVD height increases.2,6 Hydration fluctuations of the IVD are required for homeostasis and contribute to overall spinal health.
Evidence supports that body movement, position, and other variables influence IVD height changes.7 Previous studies have used radiography, computer tomography (CT) and magnetic resonance imaging (MRI) to measure IVD height. However, valid and reliable measurement tools that can record cervical IVD height changes at point of care and in a variety of environments are lacking.8–10 Stadiometry has been used to measure overall spinal height changes, but is not able to measure segmental cervical spine height. Magnetic resonance imaging is noninvasive and represents the reference standard imaging that can be used to measure segmental spine height without ionizing radiation, but is limited due to cost and access.11 Reliability of MRI measures of cervical IVD height have been reported as good (ICC≥0.6) to excellent (ICC≥0.8), but is cost-prohibitive.12,13 While plain radiographs and computer tomography (CT) have been validated and determined reliable for measuring IVD height, they have isolated benefits to clinical researchers and are not preferable to vulnerable populations (e.g., metastasis, pre-pubescence, etc.) due to radiation exposure.8,14 Musculoskeletal ultrasound (MSU) is a safe and is increasingly available imaging modality. Musculoskeletal ultrasound allows researchers to control for certain variables that affect measurements such as timing and body position that are limited with MRI. Musculoskeletal ultrasound has displayed good reliability and validity for in vitro and in vivo IVD measurements in lumbar spine models, but literature related to the cervical spine is lacking.11,14–16 Harrison et al.11 found MSU promising for measuring spinal health in astronauts during long-term space flight, although it was poorly correlated to MRI in the cervical spine.12 The authors did not control for extraneous variables such as timing and positioning between MSU and MRI image acquisition. They concluded that cervical MSU protocol refinement was necessary for measuring cervical IVD height.
To date there are no reports of a reliable and valid MSU technique for measuring cervical IVD height. This study aimed to develop a foundational methodology to allow in situ MSU cervical spine assessment. The purpose of this investigation is to determine reliability and validity of musculoskeletal ultrasound (MSU) as a tool to measure cervical IVD height compared to magnetic resonance imaging (MRI) at C4-5, C5-6 and C6-7 spinal segments. A reliable and valid measurement of cervical disc height with MSU may provide clinicians a safe and convenient method to assess the efficacy of interventions such as cervical traction or to quantify disc height in patients with neck pain.
MATERIALS AND METHODS
Experimental Design
This was an exploratory study design to investigate reliability and validity of anterior cervical spine IVD height measurements using MSU compared to MRI. This study consisted of 3 consecutive phases. Phases 1 and 2 evaluated the reliability of researchers in their ability to quantify anterior cervical spine IVD with pre-existing MRIs and MSU measurements, respectively. The third phase compared concurrent MRI and MSU image measurements within the same subjects. See Figure 1 for study flow chart.
Franciscan Missionaries of Our Lady University’s Research Scholarship Committee and Institutional Review Board (IRB) approved the study (Study Number 2020-182). Subjects in Phase I of the study had preexisting MRIs in a deidentified database and waver of informed consent was approved by the IRB. Informed consent for all other subjects in Phases II and III of the study was obtained prior to participation.
Phase 1: MRI Reliability
The sample of de-identified MRI images was obtained from a local medical center via their Office of Research and included de-identified cervical T1 weighted MRI sagittal image series of subjects with non-acute musculoskeletal cervical conditions (e.g., cervicalgia, cervical radiculopathy, and without fractures) between the ages of 18-49 years. Subjects were from a sample of convenience taken in chronologic order from newest to oldest (December 2020 to January 2020) qualified images from the existing database and assessed in January 2021.
Subjects were excluded if there was poor MRI image quality (including movement artifact) that prohibited identification of specific anatomical structures, such as the transition between the cervical IVD endplate and the cortical bone of the vertebrae. If multiple MRI imaging episodes were present for the same subject, the initial imaging episode that met inclusion and exclusion criteria was selected. Subjects over 50 years old were excluded due to the increased prevalence of pathologies17 that are not the focus population of this study.
The investigators were both musculoskeletal-trained physical therapists with more than 25 years of experience. Each trained in a one-hour session with a medical center radiologist for the MRI image measurement. The investigators were blinded and performed measurements in a random order using Visage 7 Browser 1.1.05 (Visage Imaging Inc., San Diego, California, USA) radiologic software. Investigators selected and measured the clearest representation of cervical disc on mid-sagittal MRI. Three measurements of the anterior IVD height mid-sagittal images were recorded at each of the 3 segments (C4-5, C5-6, C6-7). Three measurement episodes were repeated on the same images randomly chosen by the investigators with at least a 24-hour timeframe between measurements. Landmarks identified for measurements consisted of the closest portion of both superior and inferior IVD cartilaginous endplate where they were relatively parallel and prior to transitioning to cortical bone of the vertebral body on the anterior portion of the image before turning to meet the vertically aligned portion of the anterior vertebral body. Figure 2 represents an example of MRI measurements.
Phase 2: MSU Reliability
A convenience sample of 10 volunteer healthy asymptomatic subjects aged 18-49 were recruited from students and employees at XXX university. Subjects were screened for inclusion and exclusion criteria. Subjects had full pain free active ROM and had the ability to lie supine for up to one hour with minimal movement.
Subjects were excluded if they presented with (1) known history of acquired or congenital cervical spine pathology, surgery, or cervical spine trauma requiring medical consult; (2) pregnancy by self-report; (3) Body Mass Index (BMI) greater than 29.9 (obese) due to ultrasound inability to obtain high-quality images in the presence of obesity18,19; and (4) inability for researchers to identify cervical vertebra on MSU due to morphologic variabilities or abnormalities.
Cervical spine MSU images were acquired with the subjects in the supine position. Subjects were placed in an interventional radiography head and neck stabilizer (ORFIT Industries America, Norfolk, Virginia, USA) (See Figure 3), which standardized subject position and limited movement between imaging modalities. Subjects underwent imaging in the morning time between 6:00 and 8:00 am and remained supine for at least 10 minutes for standardization of IVD hydration.3 Musculoskeletal ultrasound data were collected with a GE LOGIQ e (R7) unit (Milwaukee, WI) using a L4-12t linear array probe. Both investigators trained with an expert sonographer for developing technique for MSU image measurement.
Vertebral segment identification was from surface palpation of identifiable landmarks that corresponded to cervical vertebral level and placing a mark anteriorly over the structures on the skin while the subject lay supine. The transducer was oriented into the long axis and structures were identified and marked on the skin to assist in triangulation through palpation of the V notch on cranial thyroid cartilage for C4, the lateral mass of thyroid cartilage for C5, and first cricoid cartilage for C6.20 The MSU transducer position was placed in the long axis of the subject’s neck in order to obtain a parasagittal oblique view between the sternocleidomastoid muscle and trachea starting at C6-7 segment and then moving superiorly, segment by segment, to the C5-6 and C4-5 IVD levels. Right side neck imaging was attempted first and then a left-side approach was used in cases of poor imaging quality due to subject anatomical morphology variations. The principal investigator who trained for more than 10 hours with an expert sonographer for the MSU image acquisition collected six total acceptable MSU images, two at each IVD cervical segment (C4-5, C5-6, C6-7). All MSU images were collected, labeled for segmental level, and saved for future measurement.
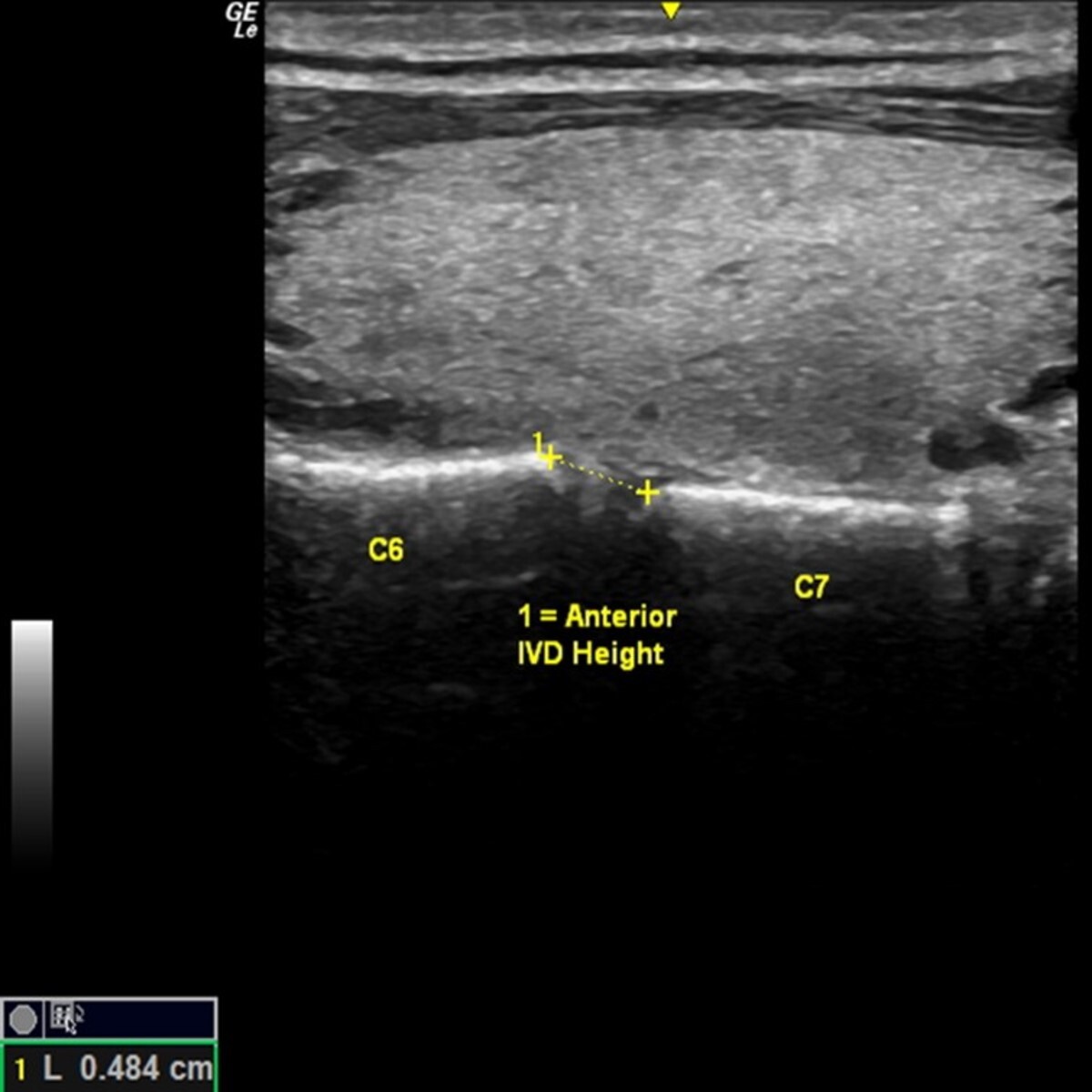
The deidentified MSU images were reviewed by investigators who agreed upon the clearest image to be measured for each segment. Investigators measured the anterior height of segmental IVD for each MSU image on non-consecutive days. The points for anterior IVD height measurement spanned from the anterior portion of the superior endplate of one vertebral body to the anterior portion of the inferior endplate of the above vertebral body. There was no blinding of the primary investigator while capturing the images but blinding of investigators occurred during all MSU image measurements. Figure 4 provides an example of the MSU measurement.
Phase 3: MSU/MRI reliability and validity
Volunteer subjects were recruited, screened, and consented as in Phase 2. Exclusion criteria was the same as Phase 2 with the addition of any contra-indications for MRI from the radiology department such as ferrous metal implants.
The MRI was a Siemens Magnetom Aera 1.5 Tesla unit and included use of the Tim 4G SlideConnect and DirectConnect coils along with the Tim Dockable Table (Siemens AG, Erlangen, Germany). The MRI protocol consisted of T1 weighted images sagittal series without contrast and without the use of the head and neck coil attachment in order to accommodate standardized positioning with the head and neck stabilizer. The MRI T1 settings protocol included 25, 3-millimeter-thick slices with a TR of 610 milliseconds and TE of 10 milliseconds.
Each subject underwent consecutive assessment in one visit between 6 and 8AM: MSU, then MRI, then repeat MSU image acquisition. The subjects were positioned supine on the MRI table quietly for 10 minutes with the head and neck placed in the ORFIT stabilizer to maintain patient position throughout the entire imaging acquisition process (MSU – MRI – MSU). The total time of image acquisitions was recorded by the investigator. The principal investigator collected MSU images at C4-5, C5-6, and C6-7 segments as described above, before and after the MRI. T1 weighted cervical spine sagittal imaging. Subjects remained supine in the head and neck stabilizer for all imaging modalities. MRI and MSU images were evaluated and measured using the methods described.
Statistical Analysis
A Microsoft Excel spreadsheet (Microsoft, Redmond, WA) and SPSS version 27 (IBM, Armonk, NY) were used to store, compile and analyze the data. Descriptive information included frequency counts, mean, standard deviation values for self-reported sex, age, subject anthropometric height and weight, and calculated body mass index (BMI) and mean values for C4-5, C5-6, and C6-7 anterior vertebral IVD height.
Inferential Analyses
For reliability, the mean of three measurements were used for both MSU and MRI analysis. Intraclass Correlation Coefficient – ICC2,3 (two-way, random effect, absolute agreement for the averages of three measurements) was used to determine inter-rater reliability for MRI and MSU anterior IVD height measurements with values of 0-0.59, ≥0.6, ≥0.75, ≥0.9 considered poor, moderate, good, and excellent reliability respectively.21 Each spinal segment’s standard error of measurement (SEM) [SEM = StdDev*√(1-ICC)]22 with 95% CI for MSU and MRI was calculated. For validity, a paired t-test was used to determine significant differences between MSU and MRI measurements, Bland-Altman plots were constructed to determine agreement between MSU and MRI measurements and a linear regression of the mean difference was used to assess for proportional bias at each anterior cervical IVD height (C4–5, C5-6, and C6-7). Alpha levels were set a priori at ≤ 0.05 and the limits of agreement for the mean bias were set at +1.96 times the standard deviation.
RESULTS
Phase 1 included four males and six females resulting in 180 IVD measurements. Subjects were 30.1+5.3 years of age with BMI of 28.4+10.3 kg/m2. Inter-rater reliability for MRI cervical spine IVD segments height (C4-5, C5-6, C6-7) measurements were between 0.91 and 0.97 (ICC2,3) for all measurements. The SEM were 0.13mm, 0.04mm, and 0.2mm for C4-5, C5-6, C6-7 segments, respectively (Table 1).
Phase 2 included 10 total subjects (7 females and 3 males) resulting in 180 IVD measurements. Subjects were 27.1+7.1 years of age, 169.3±11.0 cm. tall, weighed 67.24±13.1 kg, with BMI 23.21±2.9 kg/m2, and neck circumference of 35.84±3.7 cm. Inter-rater reliability for MSU cervical spine IVD segments height (C4-5, C5-6, C6-7) measurements were between 0.75 and 0.95 (ICC2,3) with SEM 0.33mm, 0.43mm, and 0.24mm for C4-5, C5-6, C6-7 segments, respectively (Table 2).
Eleven females and nine males completed Phase 3 resulting in 540 IVD measurements. Subjects were 24.5±2.8 years of age, 170.4±12.4 cm. tall, weighed 73.37±17.2 kg, with a BMI 24.93±3.2 kg/m2, and neck circumference of 36.02±3.8 cm. Mean total procedure time for subjects’ imaging was 23.4±3.7 minutes including the standard 10 minutes in supine prior to imaging. Total imaging time from the initial MSU to MRI to completion of the second MSU was 14.2±3.8 minutes.
Intra-rater reliability for MSU measurements for segments C4-5, C5-6, C6-7 were r= 0.875, 0.825, and .934 (p<0.01), respectively. The SEM values were 0.19, 0.19, and 0.12 for the respective segments. No significant differences were found in the mean difference between MSU and MRI measurements at any cervical IVD segments (p>0.05). Linear regression of the mean difference between MSU and MRI for each segment was not statistically significant (p≥0.129) for proportional bias (Table 3).
The construction of Bland-Altman plots for Phase 3 measurements assessed the mean difference between MSU and MRI measurements with 95% CI at each cervical level for each segment (Figures 5A-C). Visual observation of the Bland-Altman plots found no trends other than an average -0.10 mm or 2.2% (range=0.06 to 0.17 mm) underestimation for MSU measurements compared to MRI.
DISCUSSION
This study was the first to assess MSU against MRI reference standard for reliability and validity of anterior cervical height IVD measurements. This novel methodology found moderate to excellent reliability and validity values that support the use of MSU for anterior cervical IVD height measurements in further research and in clinical settings. The intra-rater reliability for Phase 3 between the two separate MSU images and measurements (pre- and post-MRI) resulted in excellent correlations at each IVD segmental level with inherent consistency with intra-rater reliability when compared to inter-rater variability. Small intra-rater reliability variations between IVD segments were seen. The highest intra-rater reliability values were at C6-C7 and lowest at the C5-C6 IVD segments. This may be due to difference in segment morphological and clarity of images acquired with MSU.
Measurement between MRI-MSU for validity were an improvement from the previous investigations on astronauts likely due to the ability to control of extraneous variables.11,16 These variables included standardization of subjects in a supine position prior to, during, and between imaging; time of day; the time between different imaging modalities; subject age; and past medical history. A previous study found that subjects in supine for less than 27 minutes resulted in observable IVD height changes.22 Thus, subjects’ standardized supine position with head and neck support to minimize movement, time of day, and timing between image acquisitions minimized movement and hydration changes. Total imaging time averaged 14.2±3.8 minutes to minimize changes in cervical IVD hydration and height. The use of the portable MRI docking table allowed subjects to remain supine without changing positions between MSU and MRI imaging. The underestimation of MSU compared to MRI measurements (≤3.9%) was smaller than the standard error of measurement (≤4.3%). This suggests that the observed underestimation falls within the range of expected measurement variability, indicating that it is statistically negligible.
Subjects in this study were young adults without a history of diagnosed cervical pathology or painful neck conditions. Previous authors found little correlation between MRI and MSU measurements in astronauts recorded on earth, likely influenced by the older age of subjects with aerospace occupations, as well as not controlling for subject cervical lordosis, time of day, and timing between imaging modalities.11 Those subjects’ demographics have been associated with increased prevalence of cervical pain and pathologies that resulted in image measurement difficulties.18,23
Previous MSU studies identified cervical segments by locating the vertebral artery as it enters the transverse foramen at C6.11,16 Anatomical variation of the vertebral artery entering different segmental levels has been found in at least 15.7% of subjects.24–26 These variations may contribute to the previously reported poor correlation between MSU and MRI.11 The current study used a different methodology to identify cervical segmental levels (C4-5, C5-6, C6-7) during MSU image acquisition. Cervical level was determined through surface palpation of structures corresponding to segmental level and then the MSU transducer was aligned accordingly to identify the cervical segmental level.20
Other validated measurement methods for spinal disc height and changes include stadiometry, MRI, CT, and radiography for measuring spinal height and changes; however, they lack the potential accessibility and utility of MSU.5,9–11 Radiographs, CT and MRI have drawbacks for researchers and clinicians. They are impractical to use due to the relatively fixed location of equipment, cost, unnecessary exposure to ionizing radiation, and inability to assess subjects in real-time during or immediately following interventions. Stadiometry avoids most previously mentioned pitfalls, but it is unable to directly measure individual IVD height. MSU is beneficial in both laboratory and clinical settings owing to portability and the ability to assess subjects in various conditions and in a wide variety of environments including aerospace microgravity. The impact this study’s findings on reliability and validity of MSU imaging of the anterior cervical spine IVD height is the foundation required for future studies and will allow for data collection that will foster better understanding of IVD behaviors in clinical settings.
Clinically, these findings may have implications in evaluating changes in disc height with sustained postures and occupational tasks. These measurements may provide information on the changes to disc height after interventions such as cervical traction or mobilization. Furthermore, these methods may be used to establish normative values to potentially identify patients at risk for degenerative conditions of the cervical discs.
This study’s limitations to external validity included the majority of subjects in Phases 2 and 3 were younger adults without a known history of cervical pathologies with BMI under 30.0, which may not be applicable to other populations. The majority of subjects presented with smaller neck sizes due to exclusion criteria and were easier to image with MSU; a larger and more muscular neck may be more difficult to capture high quality MSU images.
Internal threats to validity include different measurement location for MRI between Phase 1 and Phase 3 to include the entire endplate as it transitioned to cortical bone. In addition, the methodologies used in this study required considerable practice and control of extraneous variables that could limit application in certain clinical settings.
Future studies should investigate symptomatic populations with acute or chronic neck pathologies to determine MSU reliability and validity, as well as the effects of various positions and movements on cervical IVD height including longitudinal observations both in athletes and elderly population to seek programs that prevent IVD degeneration and stenosis associated with spinal shrinkage.
CONCLUSION
The results of this study indicate that musculoskeletal ultrasound is reliable and valid indirect measure of IVD hydration and health. This study design improved upon a previously described MSU protocol, finding that averaged good to excellent reliability and validity of measuring anterior cervical IVD height. The methodology of this study provides the foundation for future MSU studies investigating the effect of various positions, changes in positions, and movements on cervical IVD height and hydration.
Disclosures
There was no funding or conflicts of interests for this study.

_height_measurements_at.jpeg)






_height_measurements_at.jpeg)