Introduction
Foot pain is very common in both athletes and in a variety of vocations. One of the plantar fascia’s main roles is to provide passive support to the medial longitudinal arch on the sole of the foot. This support is compared to a tie-rod tension producer during weight bearing in the human foot.1,2 When loaded excessively during vocational or athletic activities, overuse in the form of plantar fasciitis can occur.3–6 This can be a very debilitating condition that can seriously impact physical activity, social function, and overall health.7,8 Several studies have indicated that plantar fasciitis affects up to 10% of the United States (US) population.9,10 It is also thought to be the most common cause of adult heel pain in the US accounting for greater than 1 million doctor visits per year.
Unfortunately, the etiology of plantar fasciopathy is complex and not totally understood11; mechanical overload with both intrinsic and extrinsic factors is thought to be responsible. Intrinsic risk factors such as increased body mass,10,12,13 and extrinsic factors such as increases in intensity, frequency, and duration of exercise may contribute to plantar fascia pain.
Anatomy of the Plantar Fascia
The plantar fascia is composed of dense fibrous connective tissue that forms a band running from the calcaneal tubercle distally to the toes. This connective tissue is composed of both superficial and deep fibers.14 The superficial fibers blend into the thick dermis on the plantar sole of the foot. The deeper fascia is connected to the medial calcaneal tubercle. In addition to the superficial and deep fibers, the plantar fascia attaches to 3 distinct portions of the forefoot. The plantar fascia forms 3 distinct bands and include the medial, central and lateral bands.11 The central band appears to have more importance as it is the key supporter of the longitudinal arch creating the windlass effect,15 and also assists subtalar supination during gait.16 This tissue is extremely thick, measuring from 2.0 to 2.5 mm in thickness and is very tough with the ability to resist elongation with tensile loads up to 180 lbs.17–19 It is important to note that there are conditions in which the plantar fascia may atrophy. Romero-Morales and colleagues found that the plantar fascia in those with lateral ankle sprains had statistically less cross-sectional areas of those that did not have ankle sprains.20
Patients will typically complain of constant foot pain on the plantar surface. The classic presentation is of sharp stabbing foot pain which is exponentially increased during the first steps after a long non weightbearing period. Typically, first thing in the morning or after sitting for a long time. The pain usually gradually reduces with continued gait; however, prolonged weight bearing may also exacerbate the condition.21
The Role of MSK Ultrasound in Plantar Fascia Evaluation
Advantages
-
Real-Time Imaging: Allows dynamic evaluation of plantar fascia integrity while the foot and ankle can be moved through available range of motion.
-
High-Resolution Visualization: Provides detailed images of soft tissue structures, including the plantar fascia and the enthesis at the calcaneal tubercle.
-
Accessibility and Cost-Effectiveness: MSK ultrasound is portable, widely available, and less expensive than magnetic resonance imaging (MRI).
Limitations
-
Operator Dependency: Requires skill and experience for accurate interpretation of findings. The ability to sonograph fascia is to a large extend influenced by the operator and the availability and technical considerations of state-of-the-art equipment. It has been shown that ultrasound measurements of plantar fascia thickness is reliable in both relative and absolute reliability.22
-
Depth Limitations: Because of the superficial location of the plantar fascia, visualization is very effective, and depth does not seem to be a limiting factor for its examination.
-
Artifacts and Shadows: Bone and calcifications may create image artifacts, requiring adjustments in probe positioning and frequency.
Sonographic Technique for Evaluating Plantar Fascia
Equipment Setup
-
Transducer Type: Because of the superficial nature of the plantar fascia, a high-frequency, linear array transducer is normally used.
-
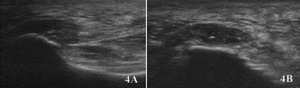
Patient Position: The patient is positioned prone on the table with the anterior ankle resting on a bolster or soft rolled towel, near the side of the examiner. The foot is relaxed as the transducer is placed in the longitudinal axis (LAX) with a slight medial obliquity along the thickest part of the plantar fascia near the calcaneus. In the SAX view, the transducer is oriented perpendicular to the long axis of the plantar fascia, typically placed just distal to the calcaneal insertion.
-
Dynamic Assessment: Stress maneuvers, such as passive dorsiflexion of the ankle and toes can be applied during MSK ultrasound to reveal fascial gapping that may indicate partial tears or functional limitations not visible at rest.
Normal Sonographic Appearance
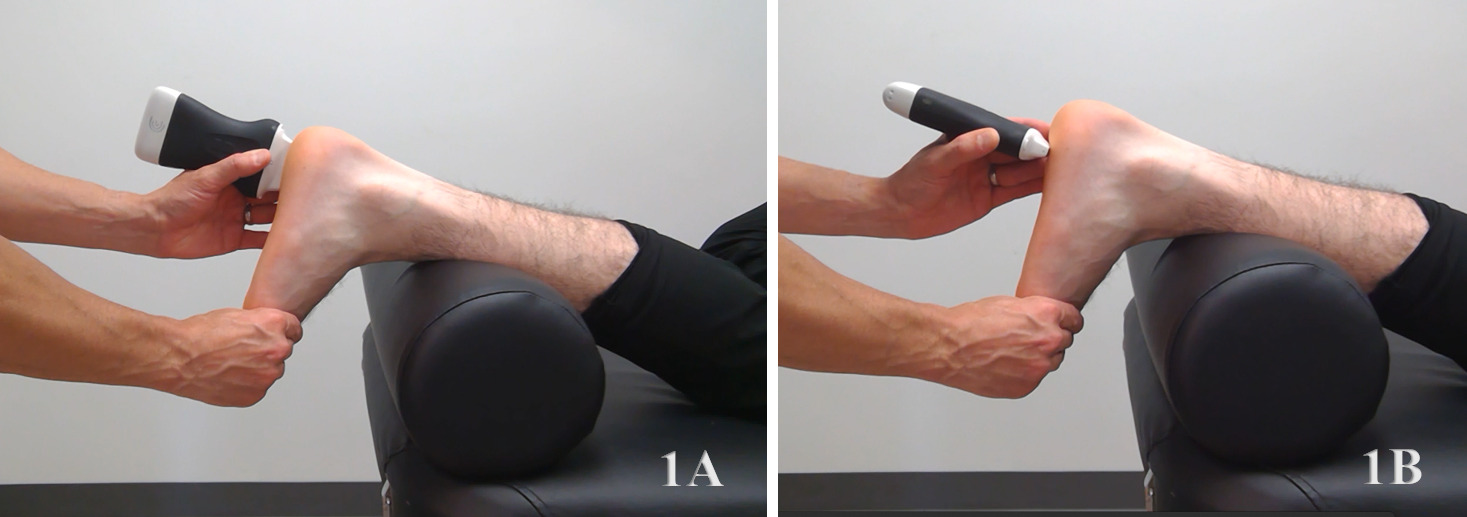
Typically, plantar fascia will be viewed in both the LAX and SAX views. In the LAX view one should start distally near the hyperechoic convexity of the medial calcaneal tubercle. It is at this location that the examiner will find the central band. The plantar fascia will appear as a hyperechoic fibrous tissue band extending from the medial tubercle to the phalanges. The lateral band can be seen by moving the transducer laterally toward the 5th metatarsal side of the foot.23 The hypoechoic tissue deep to the fascia is the interface of the deep plantar foot muscles.
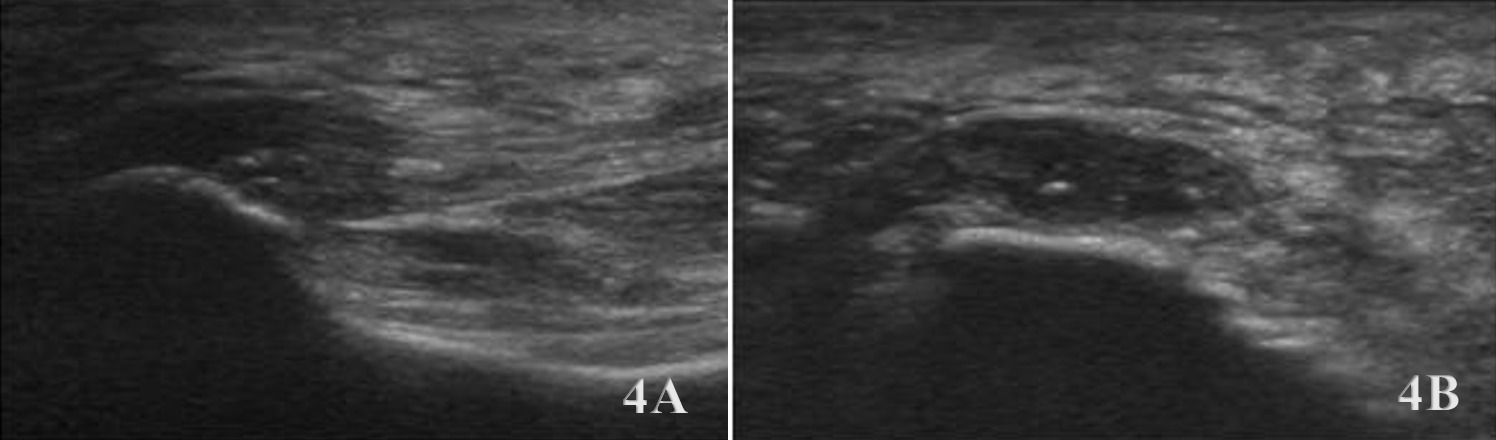
In the SAX view, the transducer is oriented perpendicular to the LAX of the plantar fascia, typically placed just distal to the calcaneal insertion. This view provides a cross-sectional image of the fascia and is particularly useful for assessing thickness and symmetry across the band. The plantar fascia in this view appears as an ovoid or slightly flattened hyperechoic structure, bordered superficially by subcutaneous tissue and deeply by the hypoechoic fat pad and intrinsic foot musculature. Normal fascia should appear homogenous with clear, well-defined borders. The SAX view is especially valuable for identifying focal thickening, hypoechoic changes, or disruptions in fiber continuity, which may indicate fasciopathy or partial tearing. This orientation also allows for comparison between the medial, central, and lateral fascial bands when sweeping across the foot.
Pathologic Findings in Plantar Fascia Pathology
-
Hypoechoic thickening due to swelling and edema
-
Disruption of fibrillar pattern in partial tears and ruptures
-
Associated joint effusion
-
Calcifications (heel spurs) are near the enthesis site
Clinical Implications for Rehabilitation Providers
MSK ultrasound provides real-time feedback for rehabilitation professionals, facilitating early diagnosis and intervention. Key applications include:
-
Early Detection of Injury / Accurate Injury Grading: MSK ultrasound can quickly differentiate between fascial thickening, bone spurs, or a more sever plantar fascia rupture to help guide treatment planning.
-
Dynamic Functional Testing: Rehabilitation professionals can use MSK ultrasound during physical therapy sessions to monitor recovery and assess ligament function dynamically. Serial MSK ultrasound imaging aids in assessing tissue remodeling, thickness and readiness for rehabilitation progression.
-
Guided Interventions: Ultrasound imaging assists in precision-guided injections, such as corticosteroids for inflammation.
-
Patient Education: Real-time imaging serves as a visual aid to explain the nature of the injury and set realistic expectations for recovery.
Limitations and Challenges
Despite its advantages, MSK ultrasound cannot entirely replace MRI for complex foot cases. Additionally, the expertise required for optimal imaging technique limits its immediate adoption across all rehabilitation settings.
Conclusion
Diagnostic MSK ultrasound is a valuable tool for the evaluation of the plantar fascia injuries at the foot, offering fast, accurate, and cost-efficient imaging for rehabilitation professionals. Its ability to provide real-time, dynamic assessments makes it particularly suited for rehabilitation providers who can integrate the MSK ultrasound findings into clinical decision-making, optimizing treatment strategies and improving patient outcomes. However, practitioners must be adequately trained to maximize its diagnostic potential. By integrating MSK ultrasound into practice, rehabilitation providers can enhance patient care, improve outcomes, and reduce the burden of false diagnoses or delayed treatment.
Patient Positioning
The patient is positioned prone or seated with the foot resting in a neutral or slightly dorsiflexed position to tension the fascia. Keep the great toe in a neutral or slightly dorsiflexed position as well. A towel or foam roll may be placed under the ankle for stability.