INTRODUCTION
Sports-related concussions (SRCs) are classified as mild traumatic brain injuries (mTBIs), characterized by a complex pathophysiological cascade triggered by biomechanical forces.1 In the United States alone, approximately 3.8 million SRCs occur annually.2 While epidemiological studies have detailed incidence rates for various contact and non-contact sports,3–5 data on SRC rates in figure skating remain scarce.6 A cross-sectional survey, presented via poster presentation, found 27% (n/N =24/88) of their figure skating sample had experienced at least one concussion. Notably, 42% did not seek medical attention. The most common mechanism of injury was a fall during on-ice activities.7
Typically, symptoms from SRCs are resolved within 7 to 10 days.8 However, following the implementation of the 11 “R’s”, including the Return to Learn (RTL) and Return to Sport (RTS) strategies in 2016,9 the duration for unrestricted RTS has increased fivefold.10 While the RTS strategy minimum duration is seven days, unrestricted RTS generally occurs within one month of injury.10 A systematic review encompassing 57 studies estimated a pooled mean RTS duration of 19.8 days.11,12
In 2023, the Concussion in Sport Group (CISG) published an updated consensus statement, including the revised RTS Strategy.10 This strategy, detailed in Table 1, provides a standardized framework for healthcare practitioners (HCPs) managing athletes with SRCs. Although adaptable across various sports and disciplines, it is not intended as a prescriptive guideline.10
SPORT OVERVIEW
Figure Skating is the oldest sport in the Winter Olympic Games.13 In the United States, figure skating is governed nationally by U.S. Figure Skating, which is recognized by both the United States Olympic and Paralympic Committee (USOPC) and the International Skating Union (ISU). International competitions are structured by skill levels, ranging from advanced novice to senior (elite). Disciplines that qualify for Olympic games include: women’s singles, men’s singles, pairs, and ice dance. While the synchronized skating discipline is not currently an Olympic sport, it is part of national and international specialty competitions.
Training and Performance Requirements
Needs Analysis
Figure skating is a multifaceted sport that places significant physiological, technical, and psychological demands on its athletes. An effective performance requires a complex interplay of energy systems, movement precision, artistic expression, and mental resilience.
Competitors of all disciplines (see Table 2) perform a short program (approximately 2 minutes and 40 seconds) and a long program (approximately 4 minutes and 10 seconds), with combined scores determining the final standings or ranking. Competitive levels are based on skill rather than age, however, with recent rule changes for Olympic qualification disciplines, skaters must be 17 years old for the 2024-2025 season and beyond.14
Physiological Demands
Figure skating routines demand both anaerobic and aerobic energy system engagement. Anaerobic power and capacity are critical for executing explosive elements such as jumps and spins, which require short bursts of maximal effort. Simultaneously, a well-developed aerobic base is essential for maintaining stamina and performance quality throughout the entire routine.
Strength, particularly in the lower body, underpins the athlete’s ability to generate height and rotational velocity during jumps. In pair skating, upper-body strength is equally vital for lifts and throws. Flexibility plays a crucial role in achieving the required range of motion for spins, spirals, and aesthetically pleasing movement lines. Balance and coordination are foundational to virtually all elements in figure skating—from edge work and intricate turns to stable landings. Core stability supports these movements by enhancing posture, control, and spin mechanics.
Technical Demands
Figure skating is highly technical, requiring mastery of a diverse set of skills. Jumps such as the Axel, Toe Loop, and Lutz demand precise timing, explosive leg power, and in-air control. Spins challenge an athlete’s balance, flexibility, and proprioception, while intricate footwork sequences test agility, speed, and edge precision. Artistic components are equally significant. Figure skaters must integrate choreography with musicality, demonstrating emotional expressiveness and interpretive depth—elements that are heavily weighted in scoring.
Psychological Demands
As a judged sport, figure skating places considerable psychological stress on athletes. Competitors must perform under pressure, often in front of large audiences and panels of judges. Mental focus is essential to execute routines with precision and consistency. Additionally, the sport demands resilience, as athletes must recover quickly from errors or falls and maintain composure throughout their performance.
Training Components
Elite athletes may devote up to 45 hours each week to their sport, with 15–30 hours spent on the ice, divided into multiple on-ice sessions, typically at 2-hour intervals. Sessions typically include an on-ice warm-up, technical elements practice (jumps, footwork), specialty drills (specific elements, combinations), program run-throughs (sequences, full/partial routines), skill refinement, and a cool down. Additionally, athletes may participate in off-ice conditioning for 5-15 hours each week, which commonly includes ballet and other complimentary strength and conditioning methods (i.e. Pilates, strength training, metabolic training).16,17 Annually, competitive demands span 7-8 months and invited touring ice show participation may span an additional two months during any calendar year.
ASSESSMENT
Concussion assessment continues to evolve in pursuit of a gold-standard. A comprehensive evaluation should include rink-side administration of the Sport Concussion Assessment Tool – 6th edition (SCAT6), a thorough examination of the cervical spine, a neurological assessment (i.e., cranial nerves, dermatomes, myotomes, and deep tendon reflexes),10 an oculomotor assessment (i.e., VOMS, King-Devick test)10 and greater dual-task testing.18 The presence and severity of symptoms should guide the need for advanced diagnostics; While emerging objective tools, including pupillometry19 and salivary biomarkers,20 are advancing in current research, they are not yet standard in clinical practice.
REHABILITATION
Healthcare team
The healthcare team commonly includes physicians, athletic trainers, physical therapists, neuropsychologists, and other healthcare professionals trained in SRC management. The healthcare team should identify a gatekeeper to oversee the athlete’s recovery and to promote interprofessional collaboration with all those involved in the care. Interprofessional collaboration should include consistent, coherent messaging to ensure the goals for clinical management are achieved. These goals commonly entail a holistic, multifaceted and individualized approach to concussion management and resolution.21,22
A local clinician should lead the athlete through the daily protocol, monitoring symptoms throughout their recovery, and evaluating their readiness to progress to the next step.23 Before unrestricted RTS, a HCP should provide documentation of readiness to RTS, as directed by local and state laws, federations such as National Federation of State High School Associations, and/or sport national governing bodies.10
Patient education
Patient education is essential to the athlete’s recovery. Specifically, patient education involving the prognosis and proposed recovery timeline is crucial for an athlete’s mental health. Literature has discovered a strong linear association between poor recovery expectations and poor recovery.24 While the CISG proposed RTS strategy suggests a minimum of seven days to unrestricted RTS, it is important to educate the athlete that unrestricted RTS in seven days is not the expectation. Supporting evidence may be shared: symptoms may resolve in seven days; however, it takes an average of 20-30 days until unrestricted RTS to allow for realistic expectations and to promote a state of mental well-being throughout the recovery process.
A qualitative study exploring patient expectations related to physical therapy outcomes found patients were interested in gaining a better understanding of, their symptoms, strategies for self-improvement, their prognosis and the clinician’s role in their recovery. Table 3 provides examples of biomedical patient education,25 to improve patient expectations.
Symptom-based classification
Concussion symptom-based classifications have been documented in the literature as: clinical profiles,26,27 clinical trajectories,28 and concussion sub-types.29 The literature predominantly describes five different symptom-based classifications: ocular-motor, headache/migraine, vestibular, anxiety/mood, cognitive/fatigue with two modifiers including: sleep and cervical/neck26,29; One study revealed the frequency of clinical profiles (N = 236): migraine (26%), motor anxiety/mood (24%), vestibular (19%), ocular (16%), cognitive/fatigue (11%).30 While some athletes may present with one classification or a clearly defined profile, many athletes will present with multiple clinical classifications or profiles.30 As with any symptom-based classification system, it is important to recognize and treat the impairments specific to the individual athlete. Table 4 provides symptom-based classification system examples.
Dual-task paradigm
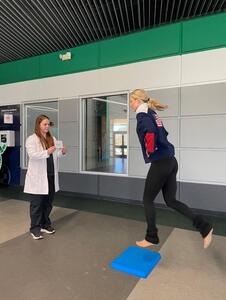
The dual-task paradigm has gained great attention over the past years and should not only be considered in the assessment but in the treatment or intervention as well. Dual-task assessment research shows athletes can demonstrate competence at singular tasks, but when performed simultaneously, their deficits become evident, including decreased gait velocity, increased medial-lateral displacement,31 decreased stride length, increased double-leg stance time,32,33 and greater cognitive errors.31 Dual-task assessment deficits should be addressed with dual-task training (DTT). Dual-task training has been shown to improve gait velocity and stride length both in single-task and dual-task environments in other neurological conditions.34,35 Tandem gait with subtraction equations or spelling words backward are examples of DTT that demonstrate strong dual-task effects.18
With the demanding necessities of the sport, such as undergoing elements at high speeds with the requirement for precise balance while cognitively preparing for the next steps in their complex choreography to be performed in time with the music, it is important to integrate cognitive and physical tasks simultaneously to prepare athletes for a safe return to sport. DTT can begin with Step 2. For example, if an athlete is in the ocular-motor symptom-based classification, the HCP can challenge the athlete with an eye tracking exercise while balancing concurrently. Progression can include a moving target, such as a Marsden ball. Figures 1-6 offer clinical examples of DTT. It is important that DTT progresses as the athlete progresses through the RTS Strategy Steps to truly replicate the necessities of the sport. For example, stroking – is a figure skating skill that incorporates gliding steps to move smoothly across the ice. Once could progress from stroking (Step 2B) to stroking while listening to their musical selection and vocalizing their choreography/sequence.
RECOVERY FACTORS
Return to play timelines have not been established for the figure skating population. Factors impacting recovery following SRC should be considered. Specifically, there is literature describing differing RTS timelines based on age,36 gender,37–40 acute clinical presentation/number of symptom-based classifications,41 premorbid/postmorbid factors,42–44 and psychosocial factors.45
Age
There is early evidence suggesting that younger age is associated with prolonged recovery times.36 However, one study comparing high school to collegiate athletes did not find age to be a clinically significant variable with SRC recovery.46 Recent literature suggests there is not a significant difference in recovery based on age.11 Further, RTL and RTS strategies can be implemented amongst different age groups with minimal differences in recovery patterns.11
Gender
In adolescent athletes, females were found to have a greater number of symptoms and symptom severity following a concussion.37 Similar reports were found in adolescent female rugby athletes.38 In a collegiate athletic setting, female athletes had symptoms for a longer duration, however, RTS timelines were similar.47 In elite European football, females were found to return to play in 20 days compared to their male counterparts, who returned in 10 days.39 A systematic review found females to be more susceptible to SRC secondary to biomechanical and hormonal differences.40 Another systematic review exploring the relationship between gender and recovery time and prolonged symptoms revealed mixed findings. Sex differences such as injury rates, differences in neck strength, injury biomechanics, and symptom reporting trends may contribute to the mixed findings.12 However, the consensus of the literature supports females having longer recovery times and having persistent symptoms.12 Conversely, a systematic review by Putukian et al11 found that all cohorts (i.e., age and gender) had similar recovery patterns. However, taking into consideration previous medical history, pre-existing factors, and postmorbid factors can modify recovery timelines.11
The total membership of U.S. Figure Skating for the 2023-24 season reached a milestone of 246,213 members, regardless of age. A detailed analysis revealed that the membership is composed of 69% females, 28% males, and 3% undeclared.48 While evidence is mixed, medical professionals working with figure skaters recovering from a concussion should consider gender as a potential factor impacting their prognosis.
Symptom-based classification
The number and severity of acute symptoms are a consistent predictor of a prolonged recovery.12 This inverse relationship has been further supported by evidence suggesting that symptom classification plays a significant role in recovery outcomes. For instance, a study involving 27 different sports within the PAC-12 found that the number of clinical profiles was positively associated with longer recovery times.41
Identifying the athlete’s symptom-based classification(s) will aid in the clinician’s application of the RTS strategy. For example, if an athlete is experiencing vestibular and ocular-motor type symptoms, the athlete may spend more time in Step 3. Classification will also enhance patient education by providing clearer insights into prognosis and the expected recovery timeline.
Premorbid/postmorbid factors
Pre-morbid factors, including concussion history,42 migraines,42 anxiety,43 learning disability,10 and mental health condition44 can impact RTS timelines. With the history of concussion being the greatest predictor of prolonged recovery.42 Post-morbid factors including increased time getting into a HCP and number of symptoms and symptom severity have a positive correlation with prolonged recovery times.10 With early symptoms being the most robust predictor.10 Specifically, light sensitivity, fatigue/low energy, balance problems, difficulty remembering, and difficulty concentrating were the symptoms with the greatest positive correlation to RTS timeframes.42 Initiating care and early physical activity play a pivotal role in an athlete’s recovery. Strict rest, cocoon therapy, and dark-room therapy are no longer considered effective treatments and have been found to impair recovery.49
Psychosocial factors
Psychosocial factors include contextual factors (i.e., loss of identity as an athlete, pressure from teammates, coaches, parents), emotional factors (i.e., depression, mental health, mood disturbance, anxiety, feelings of isolation), and fear (i.e., fear of another concussion, losing playing status).36
These factors need to be taken into consideration when managing the athlete’s recovery following a concussion. Clinicians should also be conscious of maladaptive behaviors and conditions such as Relative Energy Deficiency in Sport (RED-S).50 Subsequently, these factors should be considered when determining psychosocial readiness to RTS. One may consider utilizing the Injury Psychological Readiness to Return to Sport Scale, while not concussion specific, it is a validated instrument.51
Nutrition
Preliminary studies suggest creatine may be a beneficial supplement.52 However, weight gain is a potential side effect of creatine supplementation.53 Recent literature suggests that an acute supplementation of creatine did not affect fat mass.54 A study exploring short-term (3 weeks) creatine intake in swimmers did not impact body weight nor body composition.55
A systematic review exploring the role of nutrition identified six nutritional areas related to concussion management: omega-3 fatty acids, melatonin, Enzogenol®, MLC901, ketogenic diet, and phytocannabinoids to be beneficial.56 Some potential benefits include improvements in cognition, sleep, Sport Concussion Assessment Tool scores, systolic blood pressure volume, physical ability, and anxiety.56
While there is supporting evidence for some of these substances, HCPs working with elite athletes subjected to doping, need to ensure recommended supplements are compliant with the World Anti-Doping Agency (WADA) and the United States Anti-Doping Agency (USADA) in and out of competition. Further, HCPs making nutritional recommendations should understand which supplements are regulated. For instance, Melatonin is not a prohibited substance, but there is still an associated risk as it is not regulated by the United States Food and Drug Administration (FDA).57 One article reviewing the content of 31 melatonin supplements revealed a range of -83% to +478% of the labeled ingredients being present, far exceeding the 10% margin of the label claim. For example, one sample of a chewable tablet had 9 mg of melatonin, though the label claimed 1.5 mg of melatonin. Furthermore, contaminants such as 5-hydroxytryptamine (serotonin) were found in 26% of the supplements.58 Significant caution is recommended in the prescription or recommendations of medications or supplementation with elite level athletes as the risk of banned substances is high and the consequences of testing positive can be severe, potentially including suspension, disqualification, reputation damage, financial losses, psychological strain, and legal ramifications.59,60
RETURN TO SPORT STRATEGY
The RTS framework outlined by the CISG is a graduated stepwise strategy that involves six steps, and a minimum of 24 hours must occur between each step. Before activity, each athlete should denote their current symptoms and their symptom score on the Numeric Pain Rating Scale (NPRS). While in Steps 1-3, if an athlete has an exacerbation of symptoms, more than two points on the NPRS for more than one hour, the activity should be ceased, and the step should be attempted the next day. There should be a full resolution of symptoms, concussion-related clinical findings, and abnormalities in cognitive function, both at rest and with activity, before progressing to Step 4. If concussion-related symptoms arise during Steps 4-6, they should return to Step 3.10 Return to Learn and RTS strategies can occur in parallel; however, an athlete cannot progress to Step 4 if they are experiencing concussion-related symptoms in the classroom.
Twenty-four hours following a sport-related concussion, an athlete can begin Step 1 involving activities of daily living and walking. Step 2A & Step 2B introduce aerobic exercise at 55% maximum heart rate (HR) and 70% maximum HR, respectively. It is important to incorporate exertion testing to be able to appropriately prescribe aerobic exercise in Stage 2 and beyond. The Buffalo Concussion Bike Test61 or the Buffalo Concussion Treadmill Test62 will identify a safe heart rate zone for aerobic activity.
In Step 3, the athlete may begin sport-specific exercises, such as running and change of direction; at this step, elite competitive figure skaters may begin stroking, edge work, step sequences, and choreography (this does not include multi-rotation or high velocity rotation).
It is important to note that Step 3 should occur outside of the team setting (i.e., away from partnered elements) to minimize the risk of head impact. In figure skating, both skaters and coaches should evaluate the potential for self-injury when progressing and integrating skills, considering the likelihood of falls and the risk of secondary contact with the ice or uncontrolled coup/contrecoup mechanisms. Additionally, the risk of collisions with other skaters during on-ice sessions should be assessed, especially when interacting with athletes of lower skill levels or performing high-risk skills within the on-ice team environment. To progress beyond Step 3 the athlete must be asymptomatic, have cognitive function restored, and be free of any other clinical findings related to the current concussion.10
In Steps 4-6, instead of non-contact training drills and the progression to full-contact practice and games, it is advised to start with figure skating vertical elements. Progressing to rotation by revolution, then lastly, inversion, to mirror the development for the sport of figure skating. When initiating rotation, the onsite clinician should ensure a safe environment (i.e., spinner, pole harness, spotting); Figures 7-9 offer a progression of rotational elements from a neutral head position to cervical extension and inversion positioning.
In elite hockey, 4-5 full training sessions are warranted in Step 5, before competition readiness.63 In company dancers, there is a progressive loading into performance schedules, advancing from 2-3 pieces per night, to the full production.23 Similarly, figure skaters need to tolerate normal/customary training loads, which commonly include the completion of program elements according to their discipline and level and the integration of these elements during program run-throughs (i.e., jumps, spins, lifts, choreography). This may include the completion of multiple on-ice sessions within the same day, off-ice training within their daily training, and the completion of both short and long programs. Figure skaters will need to have several full days of training to establish physiological and psychological adaptation to obtain full clearance for unrestricted sport and build to return to competition readiness. Prior to final clearance HCPs should consider measures such as the Gapski-Goodman test64 and the Injury Psychological Readiness to Return to Sport Scale.51 A HCP should provide documentation, as directed by local and state laws, federations such as National Federation of State High School Associations, and/or sport national governing bodies, to allow unrestricted RTS.10
CONCLUSION
Sports-related concussion and mild traumatic brain injury research continues to evolve; however, the findings and return-to-sport guidelines remain scarce within the figure skating population. This clinical commentary shared an adapted RTS strategy for elite figure skaters following a concussion. As stated by the CISG, these recommendations and examples are not meant to be prescriptive guidelines but rather meant to aid the healthcare team in their clinical decision making. Amongst the multidisciplinary team, there should be a gatekeeper promoting interprofessional collaboration throughout the athlete’s recovery. A local member of the healthcare team should monitor the athlete daily and determine their ability to progress to the next step. Factors impacting SRC recovery timelines should be taken into consideration, including age, gender, acute symptom presentation, premorbid/postmorbid factors, psychosocial factors, and nutritional considerations. These recommendations were derived from current available evidence and sport specific clinical practice and will need to evolve as the research also evolves.
Acknowledgements
The authors would like to acknowledge Dr. Matthew Fazekas, MD (Medical Director of Pediatric Sports Medicine Program at Joe DiMaggio Children’s Hospital) for offering his clinical expertise and review of this manuscript, and Dr. Thomas P. Werner, PT, PhD (Assistant Dean, Faculty & Academic Affairs for Physical Therapy at University of St. Augustine for Health Sciences) for his review and edits to this manuscript. Additionally, Ashley Cain (2-time U.S. National Champion, 2022 Pairs Figure Skating Olympian; Elite Coach) and Darlene Cain (Elite Coach, Team USA, Olympic and World Level) for their review and figure skating expertise.



.png)
.png)





.png)
.png)
