INTRODUCTION
Many sports medicine professionals utilize the concept of Proprioceptive Neuromuscular Facilitation (PNF) in the rehabilitation and conditioning of their patients. PNF originated from the works of physiologist Charles Sherrington, Dr. Herman Kabat, and clinicians Margaret Knott and Dorothy Voss. Sherrington popularized a model of how the neuromuscular system operates coining the term "irradiation".1 Irradiation is defined as the spread of a response to a stimulus. This response can be seen as increased facilitation (contraction) or inhibition (relaxation) in the synergistic muscles and throughout patterns of movement.2,3 The term PNF originates from the technique developed by Dr. Herman Kabat as “proprioceptive facilitation,” with the addition of the term “neuromuscular” by Dorothy Voss in the 1950’s.2,3 The PNF techniques used today were developed as the result of work by Kabat, Knott, and Voss.2,3 Sherrington’s work provided the premise for Dr. Kabat, who began to examine natural patterns of muscle movement during treatment of polio patients. Dr. Kabat knew the myostatic stretch reflex caused an increase in muscle tension when muscle is lengthened too quickly, and the inverse stretch reflex, caused a muscle to relax when force was placed through the tendon.2,3 He believed that utilizing both of these neurophysiological principles with specific combinations of movement patterns would be more beneficial for muscle function than the standard, single joint, single plane movement. Their work combined analysis of functional movement with theories from motor development, motor control, motor learning, and neurophysiology.2–4 At inception, PNF focused on key concepts of using resistance, stretch reflexes, approximation, traction, and manual contacts to facilitate movement. The goal was to have the patient become more efficient with motor function during activities of daily living.2–4 By the late 1970s PNF strengthening techniques were incorporated into rehabilitation and strength and conditioning programs to facilitate neuromuscular control, strength, and restoration of fundamental movement patterns.4
PNF techniques use cutaneous, auditory, and proprioceptive input to address coordinated motor output which is an important component of the rehabilitation process. PNF is incorporated into rehabilitation and training programs with goals of increasing strength, flexibility, and coordination of the trunk and upper and lower extremities (LE). PNF can also help increase kinesthetic sense in response to stresses placed on the neuromuscular system,2–4 which can be beneficial for the overhead athlete in developing desired movement patterns. The PNF method is based upon promoting or hastening the response of the neuromuscular mechanism through the stimulation of the proprioceptors.2 Concentric, eccentric, and static muscle contractions are combined with gradual resistance and appropriate facilitatory procedures, adjusted to meet individual goals, typically applied during diagonal movements. PNF works by incorporating the neurophysiological principles of autogenic inhibition, reciprocal inhibition, and stress relaxation (constant applied pressure/tension to the muscles and tendons).5
This clinical commentary will present the most current evidence-based recommendations on the effectiveness of PNF for the shoulder and the scapula on upper extremity pathologies. When possible, the Strength of Recommendation (SOR) Taxonomy will be used to grade the strength of evidence that is based on quality, consistency, and patient-centeredness of the evidence (Table 1).
PNF TERMS AND DEFINITIONS
It is important to understand PNF related terms and their definitions when communicating with patients and other health care professionals. The following terms are commonly utilized in describing PNF technique and muscle contraction.
PNF is a therapeutic intervention that utilizes neurophysiological principles and provides the clinician a tool to utilize during rehabilitation and training of trunk, UE and LE neuromuscular and musculoskeletal impairments.2–4 Both structural and neuromuscular impairments affect the body’s ability to adopt and achieve optimal postures and motions, and perform coordinated and efficient movement which may lead to abnormal stresses on the neuromuscular and musculoskeletal system often resulting in pain. Proper use of PNF patterns facilitates development of desired motor patterns in patients (ie D2 pattern for UE incorporating coordinated movements of the trunk for overhead athlete).2–4,7
OVERALL PHILOSOPHY AND GOAL OF PNF
The philosophy of PNF relies upon the premise that it is an integrated approach with each intervention being directed at the whole patient, not just a particular problem or body segment, realizing that all of us have untapped existing potential.2,4
The International PNF Association defines the PNF philosophy under five subheadings: positive mental approach (full investment in the treatment), functional approach (integration of activities of daily living), mobilizing reserves (irradiation principle), treating the total person, and using motor learning and control principles. PNF is consistent with the ICF model in that it can address body structure/function impairments, enhance activities, promote participation, and can be adapted based on environmental and personal factors. Therefore, PNF is a functional and context-sensitive intervention strategy well-aligned with the biopsychosocial perspective of the ICF.4
The goal of PNF therapeutic intervention is to promote functional movement. PNF techniques use manually applied concentric, eccentric, and static muscle contractions. Desired muscle activations occur through a combination of properly graded resistance and appropriate muscle facilitation which are modified to meet the needs of each patient.2–4 The clinician adjusts the amount of resistance and type of muscle contraction to target the condition and needs of the patient, for example, muscle strength, coordination, muscle tone, pain, different body sizes, and the goal of the treatment.2–4
UNDERLYING PRINCIPLES OF PNF
The principles of PNF are based on neurophysiological and kinesiological principles and clinical experience.2–4 Each is an essential component of the approach and provides the basis for developing consistency throughout the examination and treatment process. Through applying these basic principles, the patient’s postural responses, movement patterns, strength, and endurance can be assessed and enhanced.
With the philosophy and goals of PNF in mind the following principles were developed.2–4
-
Always have a positive approach: The patient should experience little to no pain with the technique being utilized. Set the patient up for success by accomplishing prescribed tasks. Both direct and indirect treatment approaches can be utilized, and the treatment should start with a task that the patient can perform with strong muscle activation and neuromuscular control.
-
Work at the highest functional level (ICF; International Classification of Functioning, World Health Organization)8: The exercises performed should be individualized for the patient based on their functional goals and needs. The PNF techniques should emphasize both structural level and activity level exercises.
-
Mobilize potential by intensive training: It is important that the patient actively participates to the best of their ability with emphasis on motor learning and self-training.
-
Consider the total human being: PNF treatment is based on the whole person including environmental, personal, physical, and emotional factors (also consistent with the ICF model).
-
Use motor control and motor learning principles: Learning proper techniques through repetition in a different context is consistent with motor learning theory. The clinician should understand and follow stages of motor control and use varying resistance and techniques.
PNF TECHNIQUES GUIDELINES
PNF techniques are aimed at improving the overall functional ability of patients. When performing PNF exercise the following guidelines should be considered2–4,9–11:
-
Patient must be taught the PNF pattern of motion.
This will help the patient to visualize, experience the manual contacts, and understand the verbal cues for progression of the desired movement, which leads to a more effective outcome than not teaching the pattern before the treatment. PNF patterns most commonly utilize diagonal movement patterns (triplanar), that are very common in ADL’s, sports and exercise.3 It is theorized that using PNF patterns lowers the threshold for neuromuscular activation when compared to single plane pattens for initiating and completing movement.12
-
Patient should look at the moving limb.
Feedforward and feedback neural networks can influence contraction strength.13 Visual cues and feedback can help a patient control and correct body/limb position, movement patterns and elicit a stronger muscle activation.3
-
Verbal cues should coordinate with desired movements.
The verbal cues utilized by the clinician when demonstrating/performing the desired pattern or motion are crucial to having the patient complete the movement accurately. The verbal cue(s) is the driving force for achieving the accurate volitional response from the patient.2–4 Cues should be clear and concise (ie. push, pull, hold etc). It is also important to consider the timing of the command.3,14 It is important to have synchronization between the clinicians’ hand placement, resistance, and patients’ response. Verbal cueing initiates the movement while providing feedback to the patient on proper movement patterns and amount of resistance that should be utilized.2–4 It was also demonstrated that the volume of a command was correlated to the amount of muscle activation.15
-
Use manual contact with appropriate pressure to influence direction of movement.
One of the most important aspects of PNF is the use of manual contacts (hand placement) to the skin and deeper receptors that influence the desired neuromuscular response.2–4 Through the use of appropriate and specific manual contacts the clinician can influence and enhance the direction, strength, and coordination of a motor response. Appropriate manual contacts are applied to the skin and underlying muscles on the surface to which the movement or stabilizing contraction is desired. If improper hand placement is utilized, the sensory input is confusing which affects the desired motor response. It is recommended that a lumbrical grip be utilized when contacting the patient. (Figure 1) This grip allows the clinician to have better control of the diagonal motions required for each pattern.3
-
Proper mechanics and body positioning are essential.
This guideline is critical for accurate hand placement which allows the clinician to apply the desired amount of resistance throughout the pattern.2–4,12,14 The clinician must position their body in the same plane as the diagonal motion of the moving body part which helps create a stable base of support and improve neuromuscular response.2–4 Body position allows for efficient movement to occur throughout the entire PNF pattern for both clinician and patient. Total motion (body and extremities) of the clinician should regulate/meet the desired response of the body part being treated.14
-
Resistance should facilitate a maximal response.
Resistance is utilized for examination and treatment purposes. Initial and continued applied resistance enables the clinician to determine the appropriate amount of resistance needed to facilitate a coordinated, synchronized movement.2–4,12 Appropriately applied resistance can help patients reach their desired goal of increased neuromuscular control, stability, strength, relaxation, and or endurance. Efficient movement stems from the combination of isometric and isotonic muscle contractions.2–4,12 The use of resistance allows the clinician to determine the patient’s ability to efficiently perform the movement.
-
Rotational movement is critical.
The rotational component of the pattern is critical for effective resistance. Appropriately applied resistance to rotation will strengthen the entire pattern. Excessive resistance to rotation will cause undesired movement patterns to occur allowing compensatory movement patterns to detract from the targeted muscles and limiting the desired outcome of the treatment.2–4
-
Coordinated movements and normal timing of muscle contractions is desired.
Normal movement requires a coordinated progression of muscle activation that occurs through proper sequencing of muscle activation.2–4 The clinician should focus on proximal stability of the moving segment which leads to more efficient distal mobility.2,16 After proximal stability is obtained then normal timing occurs from distal to proximal with most movements.
-
Timing for emphasis is used for isotonic contractions.
Timing for emphasis utilizes appropriately applied resistance to enable a strong contraction that allows overflow (irradiation) to occur from stronger muscles to weaker muscles during a specific functional movement pattern.2–4 This principle involves altering the normal sequencing of resistance and motions to emphasize a particular muscle, action, or pattern.2–4
-
Joint receptors may be facilitated by approximation or traction.
Approximation produces compression of bony segments, which can be applied during the performance of a pattern to promote joint stability.2–4 Traction can be used to facilitate motion and decrease pain. Traction stimulates neural receptors that respond to stretch and enable motion. Application of approximation and traction can be added to the movement pattern to help facilitate the desired coordinated muscular response.2–4,12 Individual responses to traction and approximation vary.
-
Quick stretch of the muscle prior to contraction elicits a stronger contraction via the stretch reflex.
The quick stretch is incorporated into the PNF technique to facilitate contraction of associated synergistic muscles. This technique should be used with caution as it may be harmful to muscles, tendons, bones, or joints when recovering from an injury.2–4
PNF PATTERNS AND TECHNIQUES FOR THE UE AND SCAPULA
PNF patterns of motion are based on normal functional movement and use diagonal, gross movement patterns that reflect typical activity, aiming to elicit a normal neuromuscular response through synergistic muscle activation.
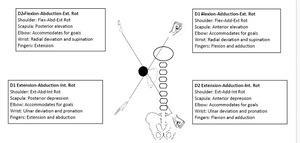
Each diagonal occurs in three planes of motion across multiple joints—Flex/Ext, Abd/Add, and Rotation—with rotation being the most important when replicating normal physiologic motion. (Figures 1 and 2) These rotational and diagonal components are in line with the orientation of biarticular muscles responsible for the movement.2,3,9–12
PNF patterns can be isolated into parts to address specific muscle weakness, inhibition, and/or joint stability. Manual resistance can be extremely beneficial in cases where the clinician wishes to increase or decrease resistance during a portion of the range of motion. Additionally, the control of the clinician is not just through resistance, but the grip (or touch) combined with their visual and verbal commands. Manual resistance allows the clinician to control range of motion, which should occur within a pain free, voluntary range of motion to minimize the risk of injury.
PNF Techniques2,3,9–12,17
Rhythmic Initiation (RI) is used to teach the desired movement pattern or movement to the patient. The goal of this technique is to elicit a response, improved coordination, speed, and function of the movement pattern starting with passive movement, progressing to active assistive, active, and finally with resistance.
Dynamic Reversals (DR) or Slow reversal (SR) incorporates an isotonic shortening contraction of the muscles utilized in the agonist pattern followed immediately by an isotonic contraction of the antagonist muscles of the movement pattern. This technique is best for increasing coordination, strength, and endurance.
Agonist Reversal technique (Combination of Isotonics)(CI)2–4,12 is used to facilitate functional movement throughout a pattern or task. Both concentric and eccentric contractions of the agonists are utilized. The focus of this technique is to promote functional stability in a smooth, controlled manner (controlled mobility). Other goals include increasing muscle strength and endurance, improving coordination, and eccentric control.
Slow reversal-hold (SRH) involves (1) an isotonic contraction of the agonist, (2) immediate isometric contraction of the agonist (hold) at end range of desired movement, (3) isotonic contraction of the antagonist, and (4) immediate isometric contraction of the antagonist (hold) at end range of desired movement. SR and SRH techniques can be implemented to increase strength, flexibility, and dynamic control. SRH can be utilized at any point in the rehabilitation process where strength training is indicated. The accommodating resistance is manually controlled by the clinician, so it can be minimal, moderate, or maximal resistance, meeting the needs of the patient. The frequency is determined by the clinician based on their evaluation of the patient’s injury status, strength, and endurance.
Rhythmic Stabilization (RS) is utilized to increase joint stability, decrease pain, and increase ROM using isometric contractions of the muscles surrounding the joint. The procedure for this technique is (1) isometric contraction of the agonist immediately followed by (2) isometric contraction of the antagonist. When RS is first initiated the joint should be placed in a stable position, and as the patient progresses the joint can be placed in less stable positions (i.e., when increasing shoulder stability, the shoulder should be placed at or below 90 degrees of flexion, and as the patient progress the shoulder can be moved to positions of flexion and abduction above the head while performing this technique). If using RS to decrease pain and/or increase ROM, go to the point of tightness and/or pain, apply the RS technique, then move into the increased pain free range.
PNF UE Patterns
PNF UE patterns are based on tri-planar functional movements that incorporate the entire upper extremity and scapula. There are four separate pivots described in UE PNF. The foundation pivot (scapula), proximal pivot (shoulder), intermediate pivot (elbow), and distal pivot (wrist and hand). PNF patterns can focus on all pivot areas as a whole or broken down into components to emphasize the area in which the patient needs improvement in stability, strength, coordination and/or ROM.
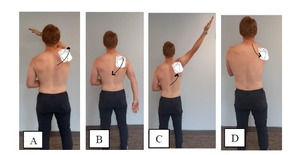
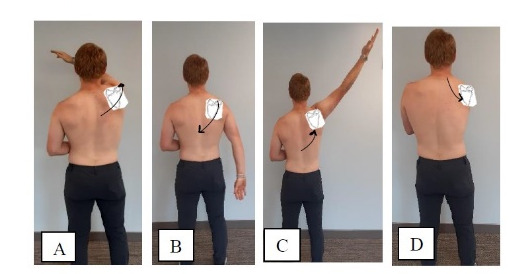
UE PNF patterns are described in Figure 1. Please see supplementary, 1, 2, 3, 4, 5, and 6 for demonstrations.
PNF Scapular patterns
There are two diagonal scapular patterns: anterior elevation/posterior depression and anterior depression/posterior elevation. (Figure 2). Scapular anterior elevation/posterior depression occurs with PNF pattern D1 (flexion-adduction pattern). The scapula moves up and forward (anterior elevation) in D1 flexion while the scapula moves down and back (posterior depression) in D1 extension. Scapular posterior elevation/anterior depression occurs in PNF pattern D2 (flexion-abduction pattern) with the scapula moving up and back (posterior elevation) in the D2 flexion, and down and forward (anterior depression) in D2 extension. Please see supplementary videos, 7, 8, and 9 for demonstrations.
EVIDENCE FOR THE USE OF PNF
Evidence for the use of PNF is grounded in the theory that a muscles’ response to a cortical stimulus increases when the muscle undergoes resistance.18 The tension from a muscle contraction has a proprioceptive facilitatory effect on that muscle and neighboring muscles and the amount of facilitation is directly proportional to the amount of resistance applied.18 It has been shown that proprioceptive facilitation from working muscles increases the response of synergistic muscles surrounding the joint and synergist muscles at neighboring joints.19 PNF was initially developed for use in patients with neurological pathology**,** however has become widely utilized as a therapeutic rehabilitation tool treating, rotator cuff pathology, subacromial pain syndrome (SAPS), scapular instability, arthritis, and lumbar and cervical pathology.12,20–27 PNF techniques have been demonstrated to help patients with scapulohumeral periarthritis to relieve pain, improve shoulder function, and strengthen daily living ability**.27 SORT A**
Functional movement is multiplanar incorporating rotational components. PNF characteristics are compatible with this concept due to the rotation that occurs during the diagonal patterns.2–4,12 PNF strengthening patterns utilize elements of motor control and biomechanical theories that embody the concept of “kinetic chain” rehabilitation.28 PNF techniques are commonly used in the treatment of many orthopedic conditions such as lumbar29 and cervical pathology,30 SAPS,31–36 shoulder impingement,31,34,36–38 rotator cuff39–41 and scapular38,42–45 pathology. PNF has been shown improve lumbar ROM, lumbar muscle spasm, pain perception, and function when used in treating chronic low back patients.14,29 Furthermore, traditional strength training and functional training were compared to PNF strengthening, in the geriatric population, for improvement in the sit to stand Timed Up and Go, and functional reach test and PNF and functional training showed the most improvement in these tests.46 Based on this evidence the implementation of a PNF centered rehabilitation program focusing on neuromuscular control, strengthening, and restoring synergistic movement patterns is beneficial for rotator cuff pathology, SAPS, scapular instability, arthritis, lumbar and cervical pathology and proprioceptive deficits. SORT A
Recent evidence supports the inclusion of scapular muscle strengthening exercises in the management of shoulder pain, particularly for individuals with (SAPS) or scapular dyskinesis.27,31–36,38,43–48 Melo et al.48 reported significant improvements in shoulder function following scapular therapeutic exercises, especially when performed for at least six weeks, with approximately 30 repetitions per session. Although these exercises were equally effective as other interventions in reducing pain, they did not demonstrate superior pain outcomes alone.48 Similarly, scapular stabilization exercises have been shown to effectively reduce pain and functional disability in patients with SAPS22,23,40,42,43,48,49 More recently, individualized scapular stabilization exercises targeting specific scapular dyskinesis types have yielded superior improvements in shoulder function and activity-related pain compared to standard exercise protocols.38,43,44 It has been demonstrated that individualizing scapular-focused interventions to the specific type of scapular dyskinesis yielded greater improvements in shoulder function and pain during activity compared to standard exercise protocols. When incorporated into conventional therapy, scapular muscle strengthening can further improve clinical outcomes.38,43,44 Exercises such as serratus anterior punches and lower trapezius strengthening should be prescribed based on individual presentation, with evidence suggesting that programs lasting at least six weeks with controlled repetitions are most effective.48 These findings support the inclusion of scapular-focused interventions (including PNF and others) as complementary components of comprehensive rehabilitation programs and that scapular stabilization exercises offers effectiveness in reducing pain and disability among people with subacromial impingement syndrome.38,43,44,48 SORT B
PNF techniques have been utilized for treating SAPS, rotator cuff pathology, and post-surgical shoulder conditions.50–55 Recent research supports the effectiveness of PNF techniques in managing shoulder and scapular pathologies, including adhesive capsulitis (frozen shoulder), subacromial impingement syndrome, and scapular dyskinesis. PNF exercises have been shown to improve pain, range of motion (ROM), and functional outcomes.54,55 Scapular PNF techniques specifically target neuromuscular control deficits, improve range of motion, reduce pain, and restore normal scapular kinematics and scapulohumeral rhythm compromised by glenohumeral dysfunction.38,43,44,50,52,53,56,57 Abnormal scapular mechanics, consistently linked to dysfunctional shoulder biomechanics and increased risk of pathology, underscore the critical role of dynamic scapular stabilization in rehabilitation.38,43,44,50,52,53,56,57 Addressing scapular muscle weakness and mechanical deficits is critical for enabling a return to pain-free physical activity.57 When combined with upper extremity movement patterns, scapular PNF techniques facilitate more coordinated and synchronized motor control.3,12,38,43,44,48,56–58 SORT A
Witt et al.59 demonstrated that PNF arm patterns, especially when combined with elastic bands or weights, significantly increased periscapular muscle activation compared to traditional maximal voluntary contraction exercises. D2 flexion patterns increase activation of the upper, middle, lower trapezius, and serratus anterior, whereas D2 extension preferentially activated the serratus anterior and lower trapezius while minimizing upper trapezius activity. D1 flexion with resistance bands also increased serratus anterior activation while minimizing trapezius activation.60,61 Although it may not specifically be labeled a PNF exercise, most scapular stabilization exercises incorporate part of a PNF pattern such as the “Y” exercise with creates a posterior tilt and upward rotation of the scapular very similar to the PNF D2 pattern. SORT B
Electromyographic (EMG) studies further support the integration of targeted neuromuscular training for periscapular muscles. Patients with SAPS frequently exhibit decreased rotator cuff activation, increased upper trapezius activation, and diminished activity in the middle and lower trapezius and serratus anterior.21,48,58,60–62 Scapular strengthening exercises, such as prone horizontal abduction, are theorized to enhance glenohumeral stability by providing a strengthening stimulus for rotator cuff muscles.21,58 Additionally, studies report greater improvements in scapular position and motion when verbal and tactile feedback accompany scapular strengthening protocols compared to exercise alone, further validating PNF-based frameworks.60,61 SORT B
For upper extremity rehabilitation, PNF strengthening patterns emphasize neuromuscular control, synergistic muscle activation, and multiplanar functional movements, integrating rotational components inherent in daily activities.3,12,28,59 PNF techniques have proven effective in reducing shoulder pain, enhancing range of motion, and improving shoulder function across various shoulder pathologies, including myofascial pain syndrome, secondary impingement, and supraspinatus tears.31,41,42,45,63 A systematic review by Reijneveld et al.45 identified moderate evidence supporting PNF strengthening techniques in treating shoulder impingement, highlighting the approach’s clinical utility.45 SORT B
A consensus report from the “Scapular Summit” emphasized that appropriate scapular positioning can improve subacromial space and supraspinatus muscle performance.50 PNF applications have been shown to improve range of motion, reduce pain, and enhance functional outcomes and quality of life in patients with rotator cuff disorders.48 Voight and Thompson64 also reported that rotator cuff muscles perform more efficiently when scapular mechanics and force couples are properly restored. Moreover, PNF movement patterns appear to effectively “groove” optimal motor control for scapular function, reinforcing their inclusion in comprehensive rehabilitation plans.40,53,56,64,65 SORT B
TREATMENT PARAMETER RECOMMENDATIONS
The guidelines for exercise and rehabilitation parameters are not well established in the literature but the following can be utilized as guiding principles for impletementing UE PNF techinques. Rhythmic initiation is often a starting point, as it teaches the motion, helps the patient to relax, improves coordination, and normalizes the motion. The repeated contractions technique can be used to increase active range of motion and strength and to facilitate altering the patient’s motion towards the desired motion.2–4,12,48
Stabilization Goal23,45,48,58,59,65–68 SORT C
For each step utilize the following parameters: Hold each position for 1-2 seconds, repeat until musclular fatigue or improper (submpotimal) movement occurs. Complete 2-4 sets at least 2-3 x/week. Each pattern/step can be broken down into component movements depending on the areas that need to be addressed.
-
Scapular rhythmic stabilization progressing from most stable position to least stable position with verbal cueing and tactile feedback.
-
Scapular rhythmic stabilization progressing from most stable position to least stable position without verbal cueing. Holding each position for 1-2 seconds.
-
UE rhythmic stabilization progressing from most stable position to least stable position with verbal cueing
-
UE rhythmic stabilization progressing from most stable position to least stable position without verbal cueing
-
Add perturbation to exercises (ie perturbation of the arm with the shoulder in a Y position with resistance from a cable or band).
Functional Movement Patterns23,45,48,58,59,65–68 SORT B
A combination of neuromuscular control and strengthening exercises have been shown to be the most effective for SAPS, rotator cuff pathology, scapular dyskinesis, adhesive capsulitis, and glenohumeral instability. It has been demonstrated that using elastic bands or weights (cable or free) while performing D2 flexion generated high activation of the upper trapezius, middle trapezius, lower trapezius and serratus anterior muscles. D2 extension with elastic bands increased activity in the serratus anterior and lower trapezius while minimizing activity in the upper trapezius. D1 flexion with resistiance bands increased serratus anterior activity with minmal trapezius (all parts) activity.59
The optimal number of sets, repetitions, and days per week have not been standardized but it appears that higher number of repetitions (10-20 with a max of 30 per exercise are more effective, when performed a minimum of 3x/week with increasing intensity over a 6-12 week.66 This protocol showed66the most promising results. Each pattern/step can be broken down into component movements depending on the areas that need to be addressed.
-
Scapular pattern rhythmic initiation promoting desired movement pattern with tactile stimulation of appropriate muscles.
-
Scapular pattern dynamic reversals and combination of isotonics with tactile stimulation of appropriate muscles.
-
UE rhythmic initiation promoting desired movement pattern with desired scapular movement pattern.
-
UE dynamic reversals and combination of isotonics (concentric and eccentric) with desired scapular movement pattern.
-
UE dynamic reversals and combination of isotonics with desired scapular movement pattern with resistance bands, pulleys, or weights.
-
Weighted UE movement patterns in desired positions (positions that reflect desired activity)
-
UE movement patterns with increasing velocity of movement
Conclusion
Research supports the use of PNF techniques as part of a comprehensive rehabilitation program for the shoulder complex. The clinician should be familiar with and follow PNF principles and procedures to obtain best results. PNF techniques appear to have a positive effect for shoulder and scapular muscle strength, pain, neuromuscular control, and ROM when UE and scapular patterns are used in combination, but the evidence is inconclusive on pain reduction, scapular positioning, and overall shoulder function when used separately. It is important to incorporate PNF upper extremity patterns of motion (for both the shoulder and scapula) when preparing a patient or athlete to return to daily living or sport as the patterns of motion are related to the movements performed daily.
SUGGESTIONS FOR FUTURE RESEARCH
The use of PNF for UE pathology and scapular positioning and mechanics requires further investigation because there are few well-designed randomized controlled studies. Research that investigates the effects of type (active versus passive), volume, and frequency of UE and scapular intervention is necessary, to determine if symptom relief can be achieved and maintained. There is also a need for larger, high-quality RCTs and clinical investigations to determine which scapular and or UE impairment may benefit from the use of scapular and or UE -focused treatment. Further research should be completed to investigate which UE and scapular directed PNF is beneficial in the reduction of shoulder complex pain and improving UE movement patterns.