INTRODUCTION
Shoulder instability disproportionately affects the young, athletic population with incidence rates up to 20 times that of the general United States (US) population.1–3 Most traumatic dislocations occur in the anterior direction,4 and many are managed surgically, due to the demonstrated higher rates of return to sport (RTS) and lower rates of recurrent injury with surgical compared to conservative management in this population.5,6 The optimal operative approach for managing primary anterior shoulder instability is up for debate and varies based on the surgeon and athlete involved.7 Although non-operative management after shoulder dislocation has shown some success in short-term RTS efficiency,5 long-term outcomes have shown high rates of recurrent instability, and many patients require surgical stabilization over longer-term follow-up.8 As such, current evidence recommends early stabilization to improve long term outcomes and prevent future instability for the younger athletic population with ambition to return to high levels of activity. Shoulder stabilization procedures broadly fall into the categories of arthroscopic or open soft tissue stabilization and bony augmentation (most often with coracoid process transfer). A recent study9 described 10-year trends in surgical stabilization in the US and found the most frequently performed shoulder stabilization procedure in the United States, accounting for over 90% of stabilizations in 2018, is the arthroscopic Bankart repair. The authors of that systematic review found a significant rise (250% increase) in the popularity of the open Latarjet procedure, while that of the open Bankart has steadily declined (65% decrease) over the same period. Future modeling trends predicted these patterns to continue through 2030.9
Regardless of the chosen procedure, the goal and expectation for patients is to be able to return to their prior levels of function without recurrent instability after shoulder stabilization.10 Unfortunately, evidence suggests that while many athletes are able to RTS at a lower level than preinjury, many less return to sport at their preinjury levels of competition and performance (RTSP),11,12 and recurrent instability rates remain high. However, many studies are confounded by including recreational or retiring athletes who may place less emphasis on RTSP than those planning to return to competitive sport. For the purposes of this scoping review, the acronym RTS (return to sport) will be utilized mostly in reference to clearance for unrestricted participation in sport and clearance timeframes, while RTSP describes the outcome of returning to preinjury levels of sport.
The purpose of this review is to 1) describe the current state of RTSP and recurrence rates for competitive athletes undergoing the most frequently performed anterior shoulder stabilization procedures and the factors potentially associated with these outcomes and to 2) describe RTS clearance timeframes and how RTS clearance decisions were made in the included studies. Describing these will highlight gaps in current knowledge and provide avenues for future research to improve clinical RTS decision-making and, ultimately, outcomes for competitive athletes returning from anterior shoulder stabilization procedures. It was anticipated that RTSP (65-75%) and recurrence rates (10-20%) would be similar to those reported in current literature.
METHODS
Search Strategy
To summarize the evidence on the outcome of RTSP rates after anterior shoulder stabilization procedures, a literature search was conducted for relevant articles using the MEDLINE (PubMed), EMBASE, and OVID databases. Search terms were (‘return to sport’ AND ‘shoulder stabilization procedures’). The reference lists of relevant systematic reviews were also reviewed for pertinent publications.
Article Selection
Articles in English and published after December 31, 2013, were included if they 1) reported on the outcome of RTSP, 2) involved surgical procedures addressing anterior shoulder instability, 3) included only competitive athletes in the study sample, and 4) had at least two years of mean or median follow-up. Articles which did not report specifics about competition levels the athletic population participated in were not included.
Analysis
Summary statistics including totals and percentages are used to answer the primary questions related to RTSP and recurrent instability rates for all athletes and separated by surgery type. Gender statistics are reported as the number of athletes in each study. RTSP and recurrence rates are reported in and summarized in number of shoulders relative to the original sample size for consistency. This method was chosen to avoid confusion because some articles reported rates of RTSP for only those that attempted to RTS. Data related to RTS timeframes and criteria for clearance decisions are presented according to their presentation in the included articles.
Quality of the included articles was assessed utilizing the validated Methodological Index for Non-randomized Studies (MINORS) scale.13 The MINORS scale consists of 12 items in the case of comparative studies (i.e. case-control studies, non-randomized cohort studies), and 8 for reviewing non-comparative studies (i.e. case series without comparison group). Each item is scored as 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate). Thus, the ideal score on the MINORS scale for a non-comparative study is 16, and 24 for a comparative study.13
RESULTS
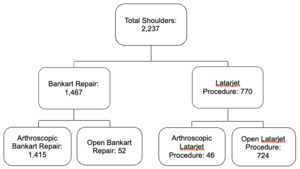
A PRISMA flow diagram14 depicting the article selection process is shown in Figure 1. Twenty-nine articles met criteria for inclusion and are summarized in Table 1. Included articles represent evidence levels III (28%) and IV (72%).15 Most articles (93%) were retrospective and represented Bankart repair alone (52%), Latarjet alone (24%), both as separate groups (20%), or as combined procedures (4%). The distribution of surgery types among the included shoulders is presented in Figure 2.
One article30 analyzed athletes who had undergone a Bristow procedure along with Bankart repair and was included with the ‘Latarjet’ category for simplicity because both procedures, though somewhat different, incorporate a transfer of the coracoid process to the anterior glenoid. Another study44 also reported on athlete outcomes after a combined procedure and was categorized with the outcomes after the Latarjet procedure. One study30 (n=152) did not report on the gender composition of the sample. Male athletes comprised 93.4% of the remaining sample. Regarding specific procedures, 89% of Bankart repairs and 96% of Latarjet procedures were performed on male athletes.
Study Quality
The MINORS13 scores for the included studies are presented in Table 2. The majority (19/29, 65.5%) of articles were non-comparative, and the remaining were comparative. The mean score for the non-comparative studies was 8.58 ± 1.35 (range 5-12, ideal score=16). The mean score for comparative studies was 14.00 ± 1.56 (range 11-16, ideal score=24). These scores indicate an overall low-level of methodological quality of the included studies.
Return to Sport at Prior Levels and Recurrent Instability Rates
Reported RTSP and recurrent instability rates are presented in Table 3. A total of 2,187 athletes (2,237 shoulders) were included. A Bankart repair was performed on 1,467 shoulders (66%), and 96% (1,408) of these were arthroscopic surgery. The Latarjet procedure was performed on 770 shoulders (34%) and 94% (724) of these were open procedures. The overall rate of RTSP was 82.3% (range 40-100%).
One study (n=51)32 did not specifically report on rates of recurrent instability and was excluded from the calculation of recurrent instability rates. Of the 2,186 remaining shoulders, 154 (7%) had recurrent instability captured during follow-up.
Bankart Repair
Bankart repair was performed on 1467 of the included shoulders. The RTSP rate after Bankart repair was 79.7% (range 40-100%). The recurrent instability rate after Bankart repair was 9.2% (range 0-20%).
Latarjet
The Latarjet procedure was performed on 770 of the included shoulders. The RTSP rate after the Latarjet procedure was 87.4% (range 78.4-100%). The recurrent instability rate after Latarjet was 3.1% (range 0-8.7%).
Return to Sport Criteria and Timeframes
Reported RTS criteria and the mean or median time for RTS clearance are presented in Table 4. Reported mean or median time to RTS clearance ranged from 11 weeks25 to 8.4 months.32 Five articles20,26,31,42,43 did not specify mean or median RTS clearance timeframes but provided general timeframes ranging from four to six months. Twenty (69.0%) articles reported RTS clearance timeframes of at least five months. Two of the included articles27,28 reported differentiated timeframes for return to play, competition, and ‘complete’ return. As no other articles specified this, it is assumed that the provided timeframes were the time of clearance for unrestricted participation in sport activities, but not necessarily to preinjury levels of performance.
Ten unique RTS clearance criteria were noted in the included articles (Table 4). If benchmark goals or cutoff scores were presented in the articles for the criteria, they are noted in the table. If a criterion was mentioned without specific goals/cutoffs, the cell was shaded grey but left blank. Strength and range-of-motion (ROM) were the most common criteria, each included in 13 of the 29 (44.8%) studies. The criteria of endurance, psychological readiness, and kinetic chain considerations were each noted by only one study.25 Of the 13 articles which analyzed outcomes after Latarjet, six (46.2%) incorporated imaging techniques to assess graft healing. As can be seen in the table, specific cutoffs or benchmarks were absent or widely variable for many of the noted criteria. Strength benchmarks for example, vary from specific percentages compared to the uninjured limb or preinjury levels to vague phrasing such as ‘full’ or ‘complete.’ Specific tests or measures utilized were not reported by any of the included articles except for the requirement of a negative apprehension test by one article.19
DISCUSSION
RTSP and Recurrent Instability
The primary findings of this review are that competitive athletes RTSP at a rate of 82% after common shoulder stabilization procedures and 7% suffered recurrent instability within a minimum two-year mean or median follow-up. These rates suggest that competitive athletes may RTSP successfully at a higher rate than reported for samples that also include recreational athletes. A recent systematic review found pooled rates of RTSP and recurrence in athletes of all competition levels to be 65% and 17%, respectively, after arthroscopic shoulder stabilization.45 Similar results were seen in an analysis of young recreational and competitive collision athletes who underwent an open Bankart repair, in which 62% RTSP and the recurrent instability rate was 25% (13% had true redislocation).46 Regarding specific procedures, those who underwent a Latarjet (87.4%) had a slightly higher RTSP rate than those who underwent Bankart (79.7%). However, the ranges of values found crossed over significantly, corresponding with findings in another recent systematic review47 which found no differences in RTSP among athletes undergoing arthroscopic Bankart repair versus Latarjet procedures in most studies included.
The higher overall rate of RTSP seen in this review stands in contrast to other evidence from individual studies which suggest that competition levels are not associated with differences in return rates.48,49 A number of the individual studies included in this review of only competitive athletes demonstrated a RTSP rate at or near 100%, including athletes ranging from high school26 to professional,23,24 while others reported rates below 50%.32 The varying RTSP rates seen in this review could be explained by the heterogeneity in the types of sport participation analyzed. There are, of course, differing demands placed on an athlete’s shoulder when participating in baseball as opposed to soccer, for example, and these different demands may contribute to disparate outcomes. Even within the same sport, the position played or the involvement of the dominant or non-dominant arm may influence RTSP. For example, some have found differences in RTSP depending on both position and dominant arm involvement in elite baseball players after Bankart repair.32 Players with non-dominant arm involvement were able to RTSP at a much higher rate (94%) compared to those with dominant arm involvement (60%). Pitchers were able to RTSP at a rate of only 57% in this study compared to 90% of infielders.32 Another study included in this review27 found similar results when they analyzed competitive teenage athletes after dominant shoulder Bankart repair. These authors found that only 59% of those who participated in overhead sports were able to RTSP while 100% of those in noncontact and non-overhead sports were able to do so.
The vast majority (93.4%) of athletes included in this review were male. This is consistent with other evidence that suggests shoulder instability is more commonly managed surgically in males than females.50 A recent systematic review and meta-analysis51 found no differences in sex-specific RTS outcomes or apprehension. They did, however, find that males were more likely to have recurrent instability.
Return to Sport Decision-Making
Regardless of the specific procedure chosen to manage an athlete’s anterior shoulder instability, the RTS decision is a complex and multifaceted process. It requires input from multiple healthcare providers, the athlete, and their coaches and trainers. The 2016 consensus statement on return to sport from the First World Congress in Sports Physical Therapy echoed this and states that a RTS decision should be made according to results of a battery of physical tests assessing an athlete’s ability to perform both open-environment and closed-environment skills that mimic the demands of their sport, and an assessment of their psychological readiness to return to their preinjury levels of sport.52 The evidence for the usefulness of these combinations is most well established in the evidence for athletes returning after anterior cruciate ligament reconstruction (ACLR) but is emerging in the management of anterior shoulder stabilization as well. Thus, it is of interest to discuss what has been done in this regard and the gaps in knowledge that remain, and to discuss what is known regarding how RTS decisions are being made by providers at this time.
Criteria-Based Return to Sport After Anterior Shoulder Stabilization
This review found that the use of specific tests and measures in the RTS decision-making process of the included studies were sparsely reported. However, many individual measures of physical function and sport-specific function have been developed and validated to some extent for assessing the surgically stabilized shoulder and athletes’ functional abilities. Many self-reported measures of function also exist and the Shoulder Instability-Return to Sport after Injury (SI-RSI) has been developed based on a similar measure developed in the ACLR literature to assess an athlete’s psychological readiness to RTS.53 It has also been suggested in the ACLR literature that a combination of at least two functional tests, psychological readiness, strength, and a minimum post-operative timeframe of eight months should occur prior to an athlete attempting to RTS.54 Many validated functional tests and methods to assess an athlete’s overall and shoulder-specific ability exist. However, none of these tests or measures has demonstrated the individual ability to predict successful RTS at prior levels. It is evident from clinical and research experts,55,56 and similar processes in the ACLR literature that some combination of both subjective and objective assessments should be used to aid the sports medicine clinician in these decisions. Some works have suggested cutoff scores for psychological readiness using the SI-RSI questionnaire,57 but this is just one component of an informed and comprehensive RTS decision, and benchmarks for other measures have not been associated with RTS outcomes. To provide guidance to the sports medicine clinician, Schwank, Blazey, Asker, et. al56 undertook an expert consensus process centered around shoulder injury and identified relevant domains to be included in a RTS decision-making process after shoulder injury. These include an athlete’s: pain, shoulder range-of-motion, strength, power, endurance, kinetic chain, sport-specific function, and psychological readiness. Although geared more generally towards upper extremity injuries, Barber, Pontillo, Bellm, et. al58 undertook an expert consensus process to clarify RTS decision-making. Consensus was reached on pain assessment via the Numeric Pain Rating Scale (NPRS), tissue healing timeframes, isometric strength ratios, use of the Disabilities of the Arm, Shoulder, and Hand (DASH) patient-reported outcome measure, shoulder range-of-motion, lower extremity/core tests, and two other physical performance tests: the Closed Kinetic Chain Upper Extremity Stability Test (CKCUEST) and seated shot-put test. Many other responses did not reach consensus in this work and the process was unable to define specific passing criteria for the overall battery or its specific components.
There is a paucity of prospective evidence on RTS outcomes based on the use of a specific, clinically feasible criteria-based RTS (CBRTS) testing battery for athletes. Drummond, Popchak, Wilson, et al.59 retrospectively demonstrated that those athletes who had undergone CBRTS testing after arthroscopic Bankart repair that included measures of isometric (external and internal rotation at 0 and 90 degrees of shoulder abduction) and isokinetic shoulder strength (external and internal rotation in modified neutral), rotator cuff (side lying external rotation) and scapular muscle (prone T and Y) endurance, the CKCUEST, and seated shot-put test, were nearly five times less likely to have recurrent instability over a year after surgery.59 In contrast, when analyzed in a small retrospective case series of athletes after the Latarjet procedure, the same battery was not found to be associated with recurrent instability or RTS outcomes at 3.6 years follow-up.60 It was, however, able to identify deficits that would be amenable to continued rehabilitation. The same CBRTS battery has also been shown to reveal strength and functional deficits in a significant proportion of athletes at six months postoperatively.61,62 Similar results were noted in an analysis of athletes within the MOON shoulder instability cohort at six months postoperatively.63 Noticeably missing from the testing batteries described in these works is an assessment of psychological readiness. Kelley, Clegg, Rodenhouse, et al.64 retrospectively demonstrated passing a battery of eight functional assessments, along with achieving a minimum score on the Tampa Scale of Kinesiophobia (TSK-11), was associated with at least one full season of successful return to competition in athletes who had undergone an arthroscopic Bankart repair for a primary dislocation. Interestingly, there was no formal isometric and isokinetic shoulder strength assessments included in this battery. They also found a low rate of redislocation (6.5%) in their cohort over two-year follow-up.64
The Shoulder-Santy Athletic Return to Sport (S-STARTS)65 composite score has been developed and initially validated for patients after undergoing the Latarjet procedure. The score is based on the results of multiple individual measures: isometric shoulder strength, SI-RSI score, a modified version of the CKCUEST, the seated shot-put test, and the Upper Quarter Y-balance test. The composite score demonstrated good measurement reliability and an ability to discriminate between healthy controls and those who had undergone the surgical procedure at three months post-operatively. The overall score also demonstrated sensitivity to change from three to six months post-operatively in those treated with Latarjet.65 The battery of tests, however, demonstrated poor internal consistency (Cronbach’s alpha=.55), indicating that the individual test items do not reliably measure the same construct, which in this case would be the ability to RTS.
The expert consensuses and work presented above, along with frameworks such as those presented by Otley, et al.55 provide valuable clinical guidance to the sports medicine clinician working with athletes after anterior shoulder stabilization. However, significant variety remains and no standardized set of tests and measures with specific passing criteria for RTS clearance has emerged or been rigorously developed and tested prospectively. This has led to significant variability in the RTS decision-making process among clinicians and in the literature.66
Clinical RTS Decision-Making
This review revealed inconsistencies and a lack of specificity regarding the RTS decision-making processes among the included studies. This finding is not unexpected, given the lack of clear standardized criteria established for RTS clearance of athletes after anterior shoulder stabilization procedures. However, some of the articles did not report any decision-making criteria other than time, and some of the domains which have reached consensus for inclusion in a comprehensive RTS decision (endurance, the kinetic chain, and psychological readiness) were only noted by one of the 29 included articles.25 These results are consistent with other recent findings. Hurley, Matache, Colasanti, et al.67 surveyed over 300 American and European shoulder and sports medicine surgeons to ascertain and evaluate their criteria for clearing athletes to RTS after Bankart and Latarjet procedures. Despite the lack of standardized criteria for RTS decision-making, they found little variation in surgeon decision-making across the groups. Over 98% of respondents identified time after surgery as a primary criterion after both surgeries. Strength (74.8% after Bankart; 67.5% after Latarjet), ROM (70% after Bankart; 65.9% after Latarjet), and the type of sport (85%) were also noted as widely used criteria. No information on how specifically these criteria were assessed and used was noted, and no other criteria were noted by more than half of the surgeons surveyed. The current review found that most (69%) of the included articles reported a RTS time of at least five months. In contrast, the survey by Hurley, Matache, Colasanti, et al.67 found that three to four months was the most identified timeframe for RTS, with clearance for those undergoing Latarjet being somewhat earlier than those after Bankart. Additionally, most surgeons noted waiting longer to clear collision athletes.
Another recently conducted survey68 garnered input from 63 French-speaking sports medicine and orthopedic surgeons and physicians evaluating their RTS decision-making criteria after first-time shoulder dislocation managed either operatively or non-operatively. They found that four criteria were used by over 90% of respondents: pain, instability/laxity, range-of-motion, and patient’s ‘subjective feeling.’ Over 75% of respondents also reported using strength, scapular dyskinesia, tendinous tests, and recovery time. These authors also asked the respondents to specify the relative importance of their used criteria and found that patients’ ‘subjective feeling’ and pain levels were the most important criteria rated. They also found significant variability in the specific methods used to assess the nine criteria described by the respondents and found that many of the methods were not supported by strong evidence. Regarding RTS criteria reported in research evidence, a scoping review of RTS criteria after rotator cuff and shoulder stabilization procedures and found that time alone was used by nearly half of the studies analyzed and they also found significant variability in the assessment methods reported for other criteria.69 For example, strength was reported as a criterion by 48% of studies and the methods of assessment ranged from broadly “full strength” to specific limb symmetry percentages on isokinetic or isometric testing.
Limitations
The results of this review must be read with consideration of its limitations. Not the least of these is the lack of prospective studies in this field. Most (93%) of the articles included were retrospective. This is indeed a well-documented issue in the shoulder instability literature as a whole70 and noted in systematic reviews analyzing athletic outcomes after shoulder stabilization procedures specifically11,45 with another finding that recurrent instability was higher in prospective compared to retrospective studies.71 Further, the aims of this review were purely and broadly descriptive, and due to the lack of high quality, prospective evidence among the included articles, no attempt was made to analyze or infer statistical differences between different surgeries, genders, or sport types. While there is some evidence to suggest there may be differences in outcomes based on surgery type48,72 and sport type,28 there has also been evidence suggesting there is not an effect.49 Others have found no differences in RTS outcomes based on gender, but did find sex-based differences in recurrence rates.51 Although no analysis was performed in this review based on gender, it must be noted that the vast majority of included athletes were male (93.4%), and caution should be applied in applying these results to female athletes. There was also no differentiation of outcomes in revision versus primary procedures done in this review, as this was not an objective therein, but it must be noted as there is evidence to support this differentiation may affect outcomes for athletes.73,74
Conclusion
Current, high-level prospective evidence analyzing RTSP and recurrent instability outcomes for competitive athletes after anterior shoulder stabilization procedures is lacking. Available evidence demonstrates significant heterogeneity and a lack of specificity regarding clinical RTS decision-making. Future work should emphasize prospective testing of specific, standardized CBRTS decision-making algorithms to improve competitive athletes’ chances to maximize their sport-related outcomes, minimize recurrent instability rates, and improve comparability between studies.
Disclosures
Adam Popchak is funded by Grant W81XWH-19-PROP-CTA (Department of Defense). The authors report no conflicts of interest.