Background
The Center for Disease Control and Prevention (CDC), monitors occupational injuries of emergency medical service (EMS) members via annual reports from emergency room visits. Rates of injuries are high, averaging >4,500 injuries per year among EMS members. This can lead to missed shifts, increased department expenses and staffing problems for vital services provided to communities.1 These data were collected from emergency room visits and do not include outpatient ambulatory care visits, which would increase the total number of cases.
A systematic review of occupational injuries among paramedics revealed an incidence of injury ranging from 29.7 to 345.6 injuries per 1000 workers per year. Sprains and strains were the most common injury, and the trunk and upper limbs were the main body regions effected. Physical use of the body was the most frequently reported mechanism of injury, accounting for 35%–55% of all injuries.2
Further investigation analyzing 82 worker’s compensation claims of EMS workers by Fratta et al. revealed 63% of injuries resulted in at least one lost workday. Fifty-one percent of these injuries occurred when a provider was moving a patient without a stretcher, 37.8% occurred from lifting or maneuvering a stretcher with or without a patient.3
To ensure basic physical readiness for active duties, fire departments, paramedics, police departments and military branches have developed physical fitness testing as part of their recruitment process and/or annual competency testing. Recently these disciplines have identified the need to transition these tests from assessments of generalized fitness to tests of specific work capacity. The Army began updating the Army Physical Fitness Test (APFT) from pushups, sit ups, and running to the Army Combat Fitness Test (ACFT) in 2013. The goal was to better test a soldier’s battlefield ability. The new functional testing protocol includes a hexbar deadlift, med ball throw, and sprint/drag/carry events. This has been instituted across the Army branch of military services.4 The Candidate Physical Ability Test (CPAT) was developed in 1999 (revised in 2007) by the International Association of Fire Fighters to assess physical abilities as part of an application to fire academies.5 The Madison (Wisconsin) Fire Department began instituting Standards (2017), a series of ladder and hose drills in full firefighter gear, to test firefighters with fireground specific functional tasks as a condition of employment and biannual competency.6
The Association of Critical Care Transport Standards Version 1.0 is a detailed document highlighting the recommended skills required of any critical care transport personnel/team in efforts to create a national standardization of care practices. This document outlines levels of training and certification, specific clinical skills required, and vehicle and equipment safety instruction. While many skills listed in this document have a physical element to them, the standards do not describe actual physical requirements such as the need to lift/carry, push/pull, walk prolonged distances, negotiate stairs while carrying equipment, etc.7
Many critical care transport organizations do not require a physical ability test. In the development of this specific institution’s Med Flight Physical Ability Test (MFPAT), institutions that do require a test were reviewed via professional electronic or telephone interaction. There was significant variation in the content and format of testing. Differences included: maximum body weight, body mass index requirements and the tests performed. Most testing involved some level of functional lifting, carrying, pushing and pulling, along with aerobic challenges. Tests ranged from lifting and carrying 25 lbs from floor to waist heights to a 185 lb mannequin drag. The format of the tests also varied. Many tests are performed using gym equipment in a clinical setting, while others perform simulated calls using actual equipment such as stretchers and ambulances. Cardiovascular assessments varied by institution and included walking, running, burpees, and stretcher management activities.
Methods
The UW Med Flight team, consisting of emergency medicine trained physicians, nurses and respiratory therapists, and the UW Health Sports Rehabilitation department began collaborative development of a health assessment for med flight crew members in November 2020. The health assessment was designed to include a maximum body mass limit for employees, hearing assessment, visual acuity exam, and a physical ability test.
The coordinator of the Sports Rehabilitation Tactical Athlete specialty program performed an onsite assessment to evaluate the distances and heights traveled, the size and weight of equipment managed, and the duties of emergency critical care providers. This included distances to and from the helipad, in and out of the helicopter, maneuvering within the helicopter and transport within the hospital.
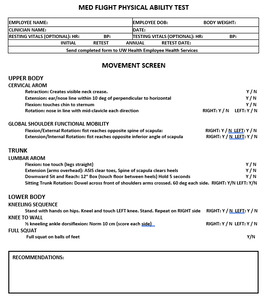
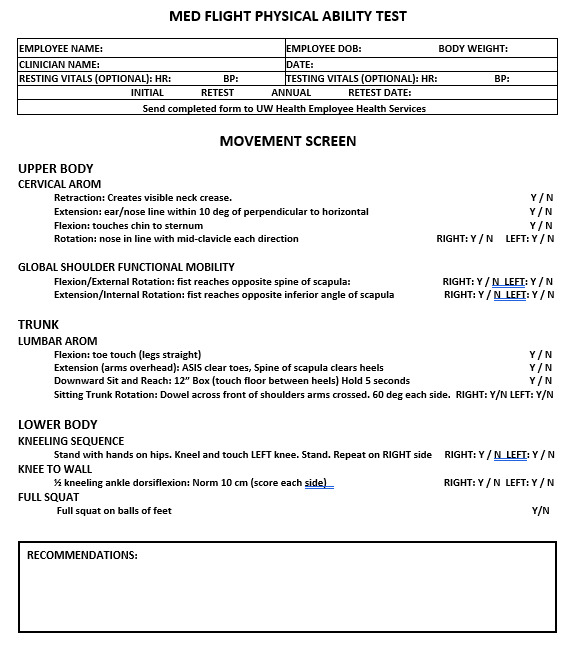
The decision was made to utilize a physical performance-based test in a sports rehab/performance center to avoid using equipment that may be necessary for a call (ambulance/helicopter), to avoid delays in testing due to inclement weather outdoors, and to allow a scenario where group testing could be implemented. Physical therapists and athletic trainers with tactical athlete sub-specialization were enlisted to develop and proctor the tests. These individuals had expertise in strength and conditioning, biomechanics, and return to sport and work testing. The initial test was designed with a total body movement screen to assess for significant asymmetries in fundamental movements of the trunk and upper/lower quarters. This screen also served as a dynamic warm up prior to the physical portion of the test. Movement screen items were selected from basic orthopedic examination as well as anticipated functional movements of med flight duties (i.e. squatting and kneeling.) Some movements are like those found in the FMSTM or SFMA, but without the additional equipment that the FMSTM requires. The overhead squat was not utilized as a basic full squat and kneel as would be used on scene was chosen to assess basic function. The movement screen was designed with the intention of quickly assessing regional movement quality to identify potential restrictions or painful movements that might translate to the practical portion of the test. In one case, a participant had difficulty squatting and kneeling during the movement screen secondary to knee pain. She then subsequently had difficulty completing the high step up and loaded walk, causing her to discontinue testing. In this particular case, it was recommended she follow up with her care team as she reported a known meniscal condition that she had not had evaluated. Others were made aware of any movement asymmetries that were noted and recommended physical therapy or consideration for sports performance training.
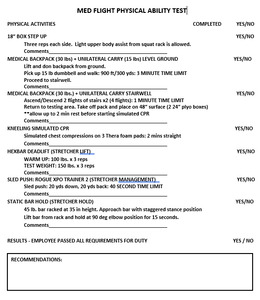
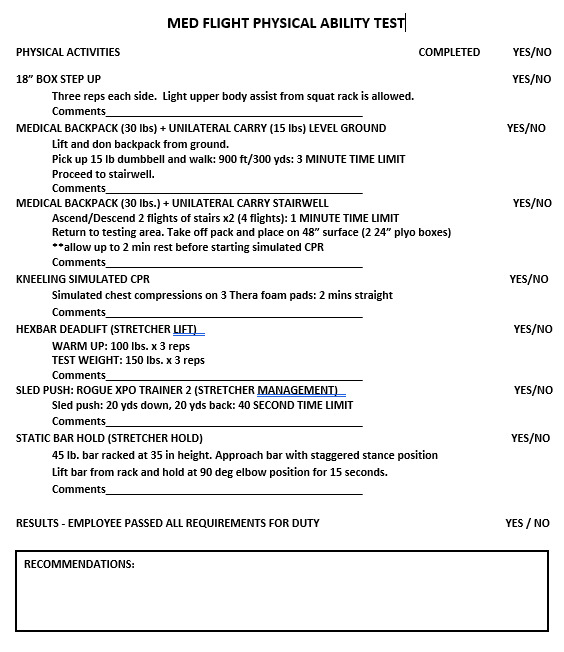
The MFPAT was designed to assess an individual’s ability to perform the necessary physical skills of critical care transport safely and efficiently. Scoring systems of other industry physical ability tests were reviewed, and a decision was made to utilize a dichotomous yes/no system to determine and record whether an individual could perform the necessary physical activity or not. A small group of med flight team members participated in a pilot practice session of the test. Timing and administration of the tests, content validity, and activity time limits were established. The 300 yd medical backpack + dumbbell carry, medical backpack + dumbbell carry stair climb and sled push initially did not have time limits set. Following the pilot practice session, 3 min, 1 min and 40 sec time limits were set respectively for these tests to establish a pace that simulated a typical response to an emergency.
The Med Flight management team hosted a series of team meetings to inform team members of the upcoming changes in policy, specifically the incorporation of the physical ability test. Videos of the test were made available for review online. Monthly practice sessions were held to allow team members the opportunity to practice each of the events and independently gauge their readiness. All staff/crew members were assessed during formal group testing sessions scheduled between January and May 2023.
Outcomes
Five group testing sessions were performed from January through May 2023. A total of 71 team members were tested, with 13 scheduled individually for logistical reasons. Of the tests performed, 69 out 71 individuals passed. One failure was due to a known knee condition that limited physical activity tolerance. That individual elected to move into a less physical role in a different department. An incoming EMS physician fellow failed the test secondary to a recent hand injury. While she was referred to physical therapy, occupational therapy and sports performance, she ultimately decided to focus her fellowship solely on emergency department medicine versus med flight.
Results of the conversations surrounding test preparation revealed that many team members were already engaged in fitness routines. Several team members were motivated to begin working out more frequently, to add resistance training to primarily cardio workouts, or to perform more functional lifts such as deadlifts, in preparation for the upcoming test. Those who came close to not passing the test admitted that they did not regularly exercise or engage in physical activity outside of work. Multiple team members had difficulty completing the medical backpack + unilateral carry on level ground and the staircase during the initial practice sessions. Some individuals also had difficulty completing the hexbar deadlift (unable to complete 3 reps at 150 lbs with good form.)
Discussion
Critical care transport team members seek to protect, rescue, transport, and care for the members of the communities in which they serve, frequently under high levels of stress and physical demands. Ensuring that team members are capable of performing not only the clinical skills, but also the physical requirements associated with the position is vital to having a team that is well prepared to respond appropriately to emergencies.
Initial attempts to screen for injury risk in groups such as firefighters using tools like the Functional Movement Screen (FMS) failed to identify a consistent cutoff score in this population.8 The Candidate Physical Ability Test (CPAT) for firefighters has been analyzed and qualities of those who have passed have been assessed. Michaelides found that upper body muscular strength, endurance, and lower body fat percentage were significantly related (p < 0.01) to better performances on the simulated firefighting tasks.9 The same author in another study found mean power during the Wingate Anaerobic Cycling Test (WAnT), fatigue index during WAnT, absolute VO2max, upper body strength, grip strength, and heart rate response to stair climbing were significantly related to improved CPAT performance time.10 Meanwhile, poor performance on the CPAT was associated with high resting heart rate, high body mass index, high body fat (BF)%, increasing age, and large waist size.11
Many tactical disciplines (fire, police, military) have instituted physical ability tests. It is unclear if this has aided in employee retention, reduced injury risk, or decreased lost work time (sick calls and missed work). Further outcomes-based research is needed. This institution intends to collect data in these areas for a longitudinal comparison, in hopes of answering some of these questions.
The implementation of this test anecdotally encouraged behavioral changes within a critical care transport team. Team members improved their fitness levels to pass the test and improve overall health which in turn improved the collective fitness levels of the group. Future group analysis is warranted to monitor injury rates and missed shifts.
Summary
This administrative case report outlined the development of a Med Flight Physical Ability Test for a critical care transport team. Many critical care transport teams across the United States do not utilize such a test. For those that do, the tests are inconsistent and lack standardization. The Med Flight Physical Ability Test was designed such that it could be replicated with relatively low-cost equipment purchases and performed in facility spaces common to other institutions should it be implemented. Further observational work of monitoring injury rates following implementation of such testing would be helpful as other teams across the nation consider such programs.
Conflicts of Interest
The authors report no conflicts of interest.