Introduction
Given their location on the most mobile, intricate portion of the human body, the susceptibility of the finger to injury is relatively high. Injuries to the fingers occur from repetitive injury from work or sports activities, or acute trauma, with trauma accounting for 28% of musculoskeletal injuries.1
Anatomy of the Extensor Tendon
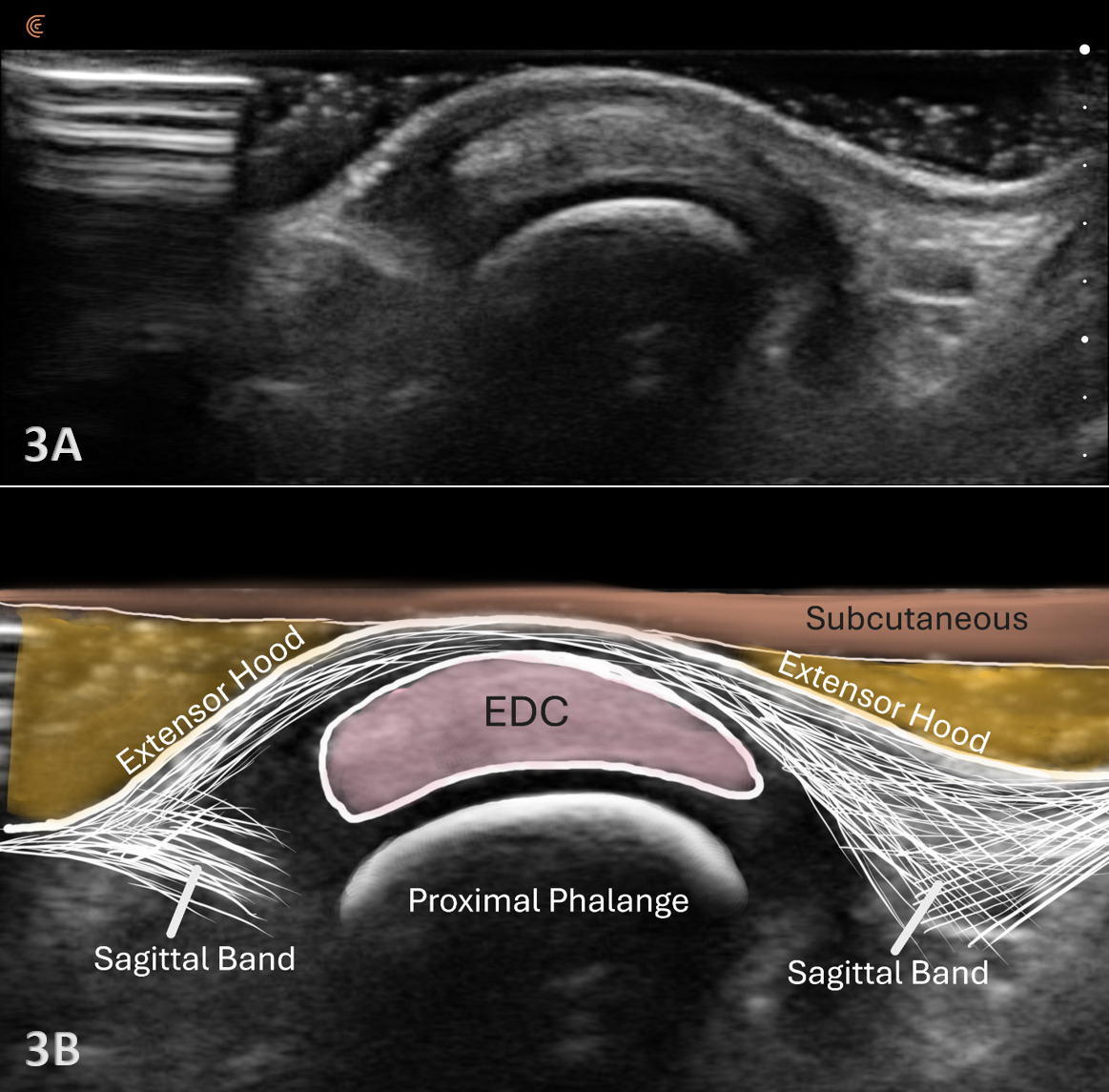
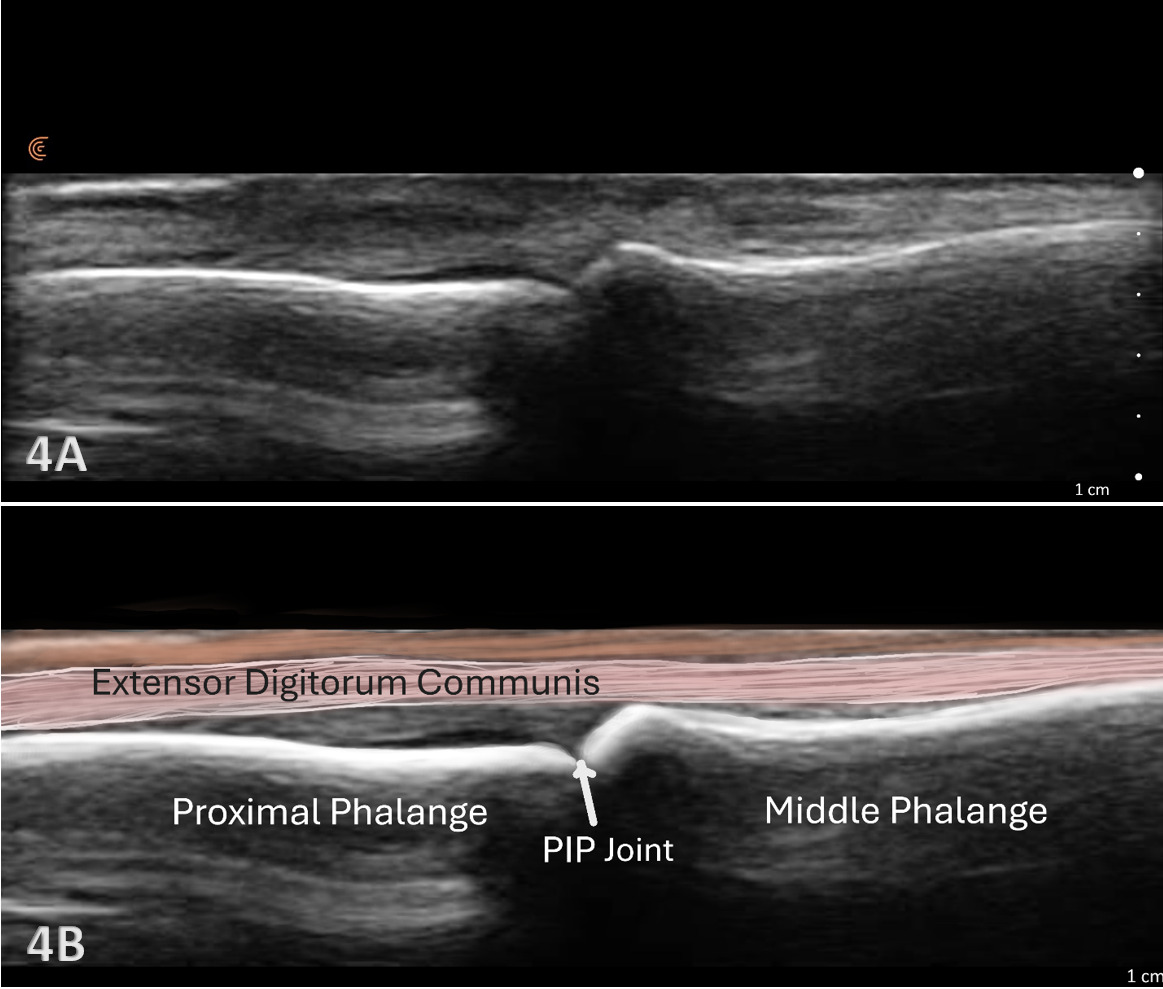
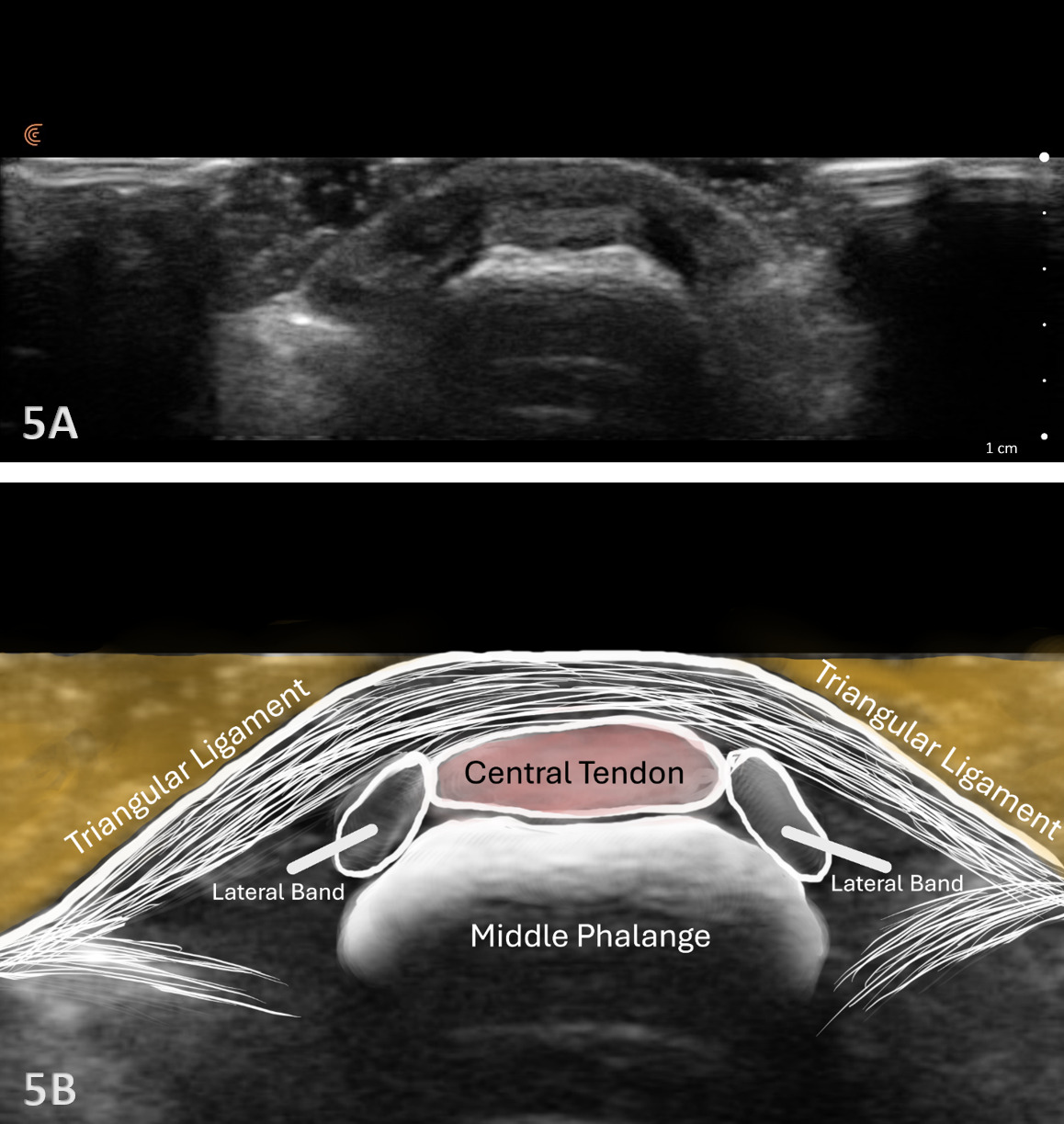
The extensor mechanism of the fingers involves 5 different zones. This article will mainly discuss the area around the metacarpals or zones III and IV. The extensor tendon runs along the dorsal aspect of the phalanges and inserts distally at the base of the middle phalanx (MP) to extend the proximal interphalangeal joint (PIP). The tendon requires other vital components to help stabilize the tendon and obtain active extension at the distal interphalangeal joint (DIP). These structures will be discussed in a later article.
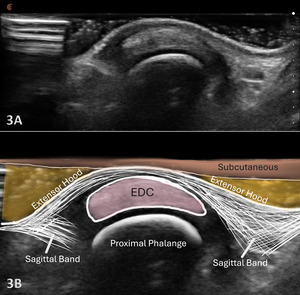
At the level of the metacarpophalangeal (MCP) joint, the extensor digitorum tendon is joined by the sagittal bands, which are part of the extensor hood. The sagittal bands on the extensor surface are further attached volarly to the palmar plate of the MCP joint. The sagittal bands are critical for stabilizing the tendon, limiting proximal excursion of the tendon, and assisting with extension at the PIP joint.
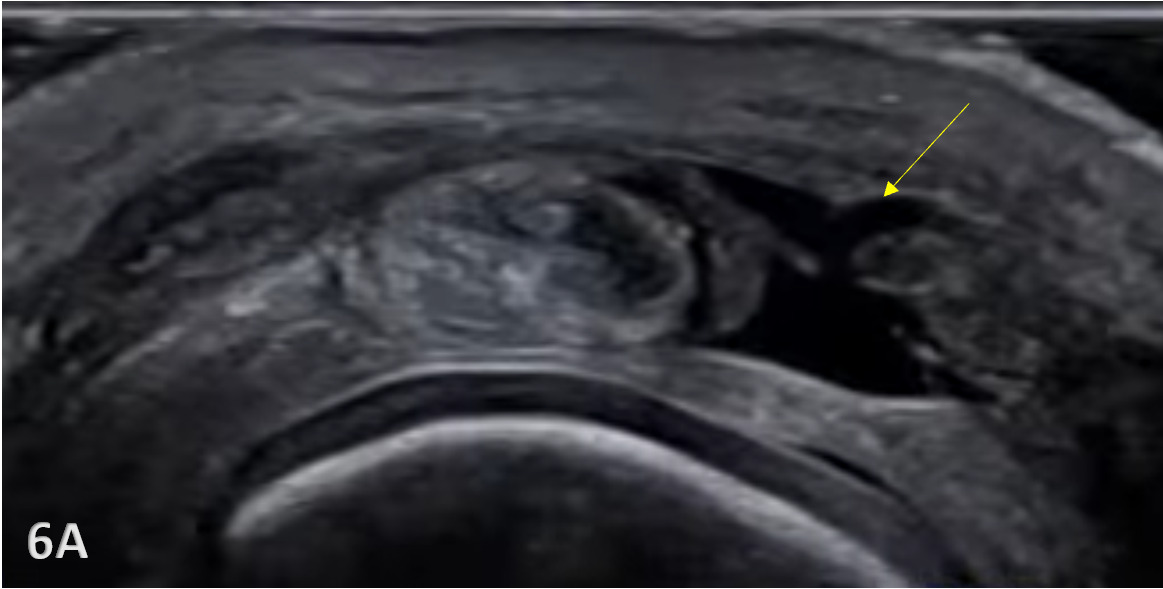
Because the superficial skin on the dorsal surface of the hand is thin, and the tendons are located superficially, they are susceptible to laceration and or avulsions from trauma. A sagittal band rupture known as “Boxer’s knuckle” can also be seen due to direct trauma or repetitive microtrauma to the MCP joint.1 With Boxer’s knuckle, the most affected finger is the 3rd, with the tendon seen dislocating ulnarly. With lacerations, obviously, an incision will be seen. However, with Boxer’s knuckle and an avulsion fracture, the injury may be closed. Pain, swelling, and diminished function of the suspected tendon will be present as the major signs and symptoms.
The Role of MSK Ultrasound in MCP/DIP Extensor Tendon
Advantages
-
Real-Time Imaging: Allows dynamic evaluation of extensor tendon integrity while the wrist and hand can be moved through the available range of motion.
-
High-Resolution Visualization: Provides detailed images of soft tissue structures, including the extensor tendon, sagittal bands, and their attachment to the PIP joint.
-
Accessibility and Cost-Effectiveness: MSK ultrasound is portable, widely available, and less expensive than magnetic resonance imaging (MRI).
Limitations
-
Operator Dependency: Requires skill and experience for accurate interpretation of findings. The ability to sonograph is to a large extent influenced by the operator and the availability and technical considerations of state-of-the-art equipment.
-
Depth Limitations: Because of the superficial location of the extensor tendons, visualization is very effective, and depth is not a limiting factor for their examination.
-
Artifacts and Shadows: Bone and calcifications may create image artifacts, requiring adjustments in probe positioning and frequency.
Sonographic Technique for Evaluating the Extensor Tendons
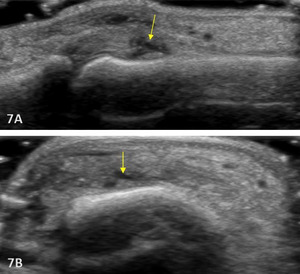
Equipment Setup
-
Transducer Type: Because of the superficial depth of the extensor tendons, a high-frequency, hockey stick transducer is commonly used. A standard linear array transducer may be used, but may not be optimal due to its size.
-
Patient Position: Patient is supine or seated with the hand resting on a pillow or supported on a table. Adjust the arm and hand position to allow optimal access to the dorsal surface of the hand.
-
Dynamic Assessment: Stress maneuvers, such as wrist and phalangeal passive or active flexion and extension, can be applied during MSK ultrasound to reveal tendon or disruptions, instability, or changes in echogenicity that may indicate partial tears, tendon ruptures, avulsions, or instability.
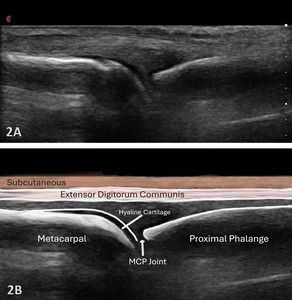
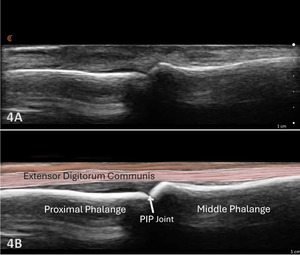
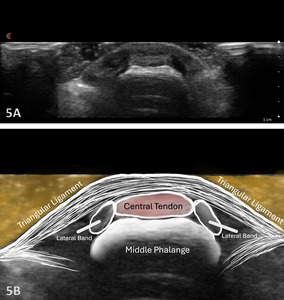
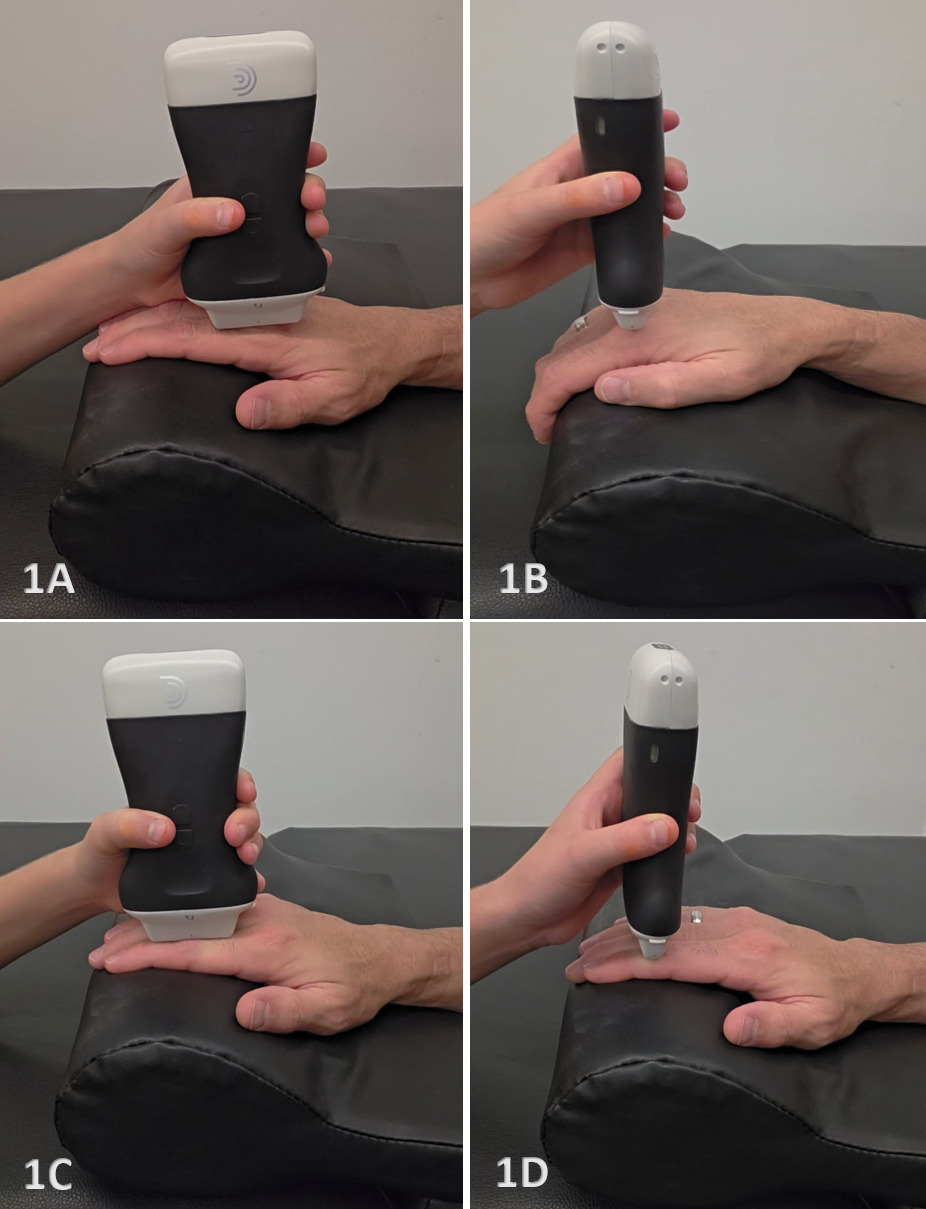
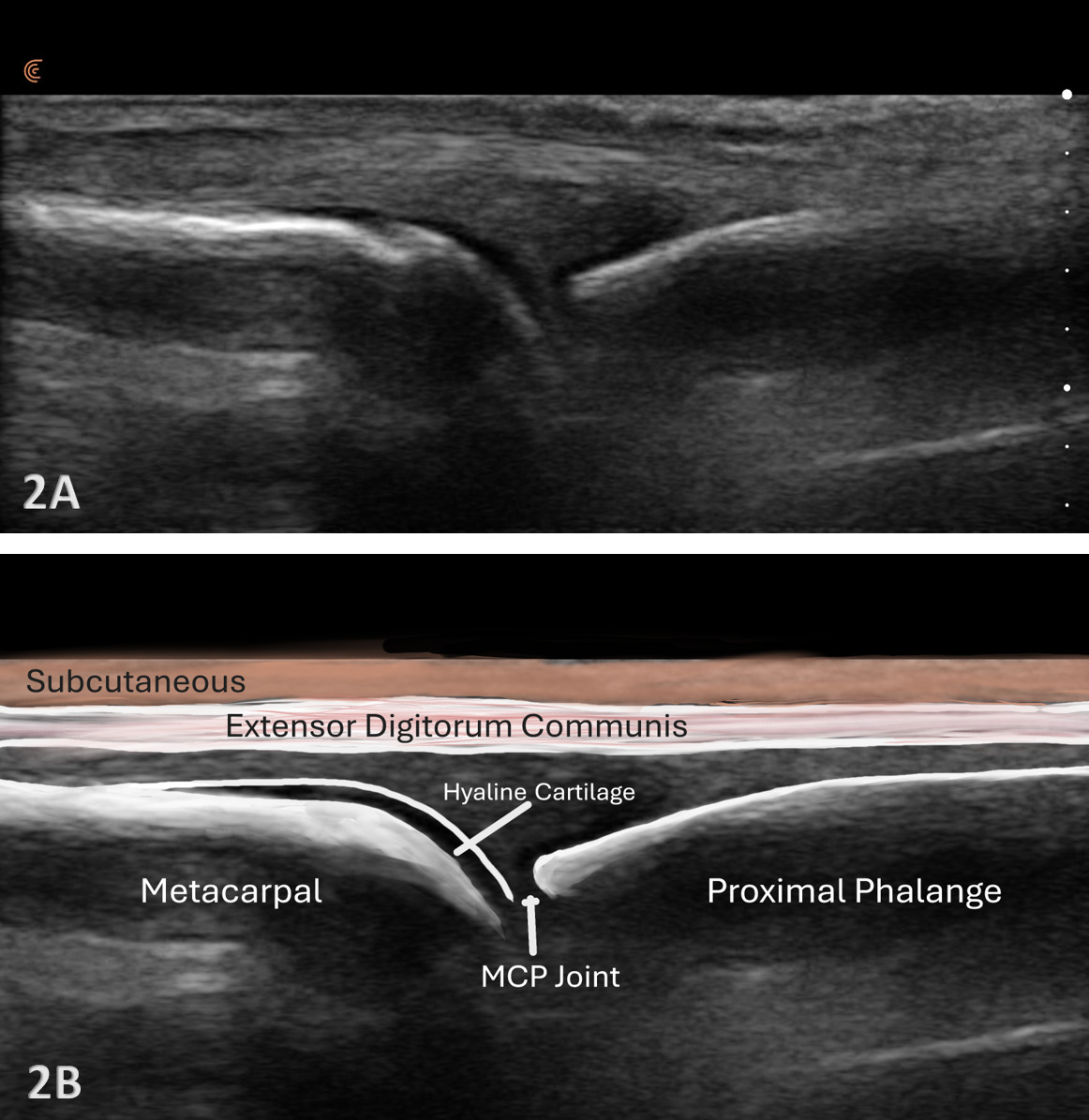
Examination Protocol Normal Sonographic Appearance
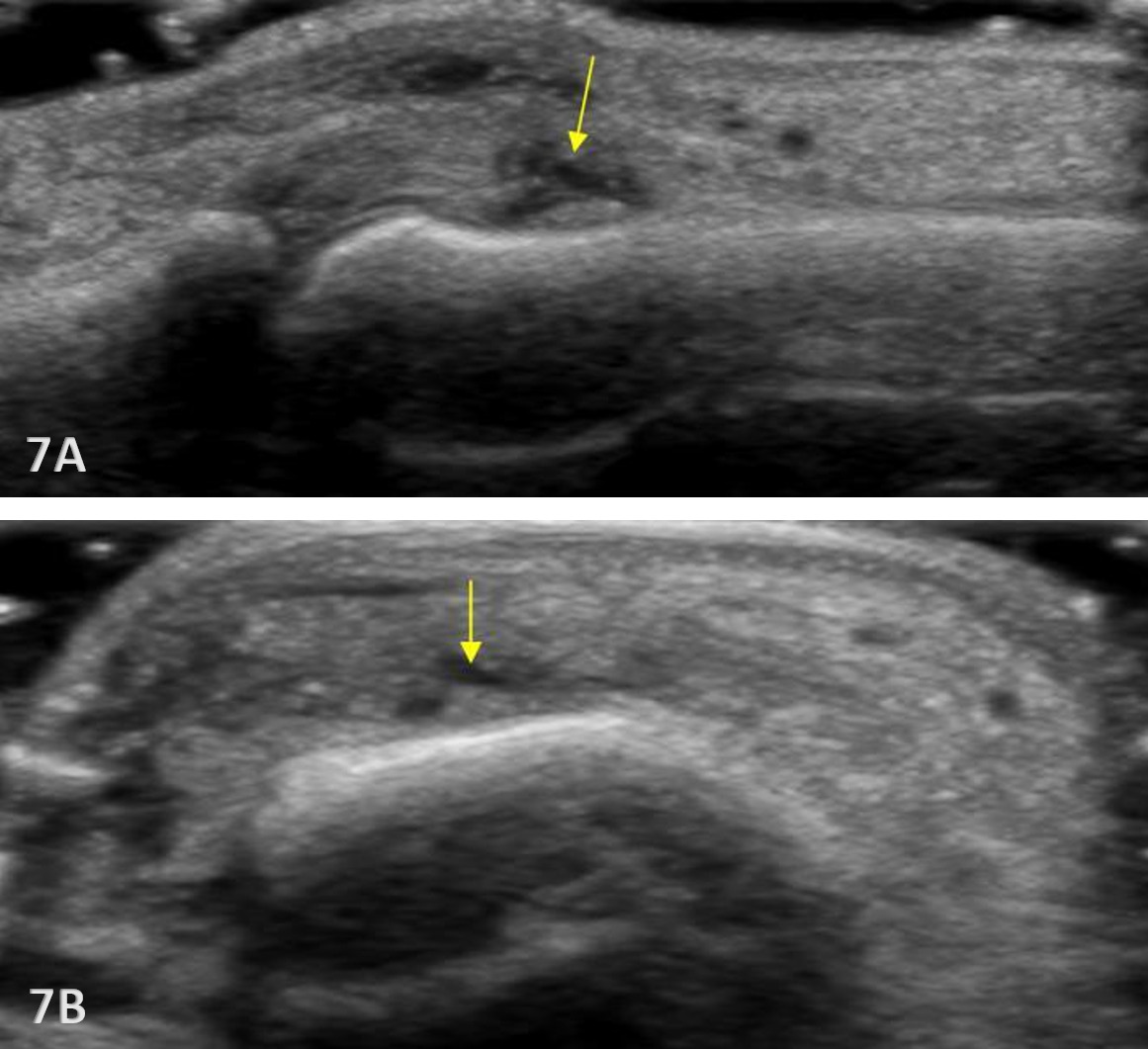
The extensor tendon can be examined in both long axis (LAX) and short axis (SAX) views. The tendons can each be seen at the MCP and PIP joints. The hyperechoic outline of the metacarpal and proximal phalanx will be seen at the MCP joint, while the proximal phalanx and middle phalanx will be visualized at the PIP joint. The extensor tendon will be an echogenic fibrillar structure in appearance. In the LAX view, the tendons will become smaller as they run more distally, making them slightly more difficult to visualize. In the SAX view, the tendon should be oval and fibular and should sit in the central position over the metacarpal. The soundhead may need to be toggled at the distal tendons’ insertion to avoid anisotropy. Dynamic visualization can be performed with resisted or active movement of the wrist or fingers.
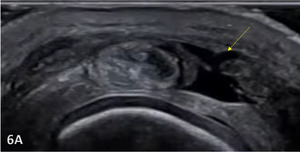
Pathologic Findings in Extensor Tendon Injury
-
Hypoechoic thickening due to swelling and edema.
-
Disruption of fibrillar pattern in partial tears and ruptures.
-
Cortical irregularity and interruption in bony avulsions of insertion.
-
Associated edema and effusion.
Clinical Implications for Rehabilitation Providers
MSK ultrasound provides real-time feedback for rehabilitation professionals, facilitating early diagnosis and intervention. Key applications include:
-
Early Detection of Injury / Accurate Injury Grading: MSK ultrasound can help guide treatment planning by quantifying tendinopathy, tendon ruptures, and bony avulsion of the insertion.
-
Dynamic Functional Testing: Rehabilitation professionals can use MSK ultrasound during physical therapy sessions to monitor recovery and assess tendon function dynamically. Serial MSK ultrasound imaging aids in assessing tissue remodeling, thickness and readiness for rehabilitation progression.
-
Guided Interventions: Ultrasound imaging assists in precision-guided injections, such as corticosteroids for inflammation.
-
Patient Education: Real-time imaging serves as a visual aid to explain the nature of the injury and set realistic expectations for recovery.
Limitations and Challenges
Despite its advantages, MSK ultrasound cannot entirely replace MRI for all finger injury cases. Additionally, the expertise required for optimal imaging technique limits its immediate adoption across all rehabilitation settings.
Conclusion
Diagnostic MSK ultrasound is a valuable tool for the evaluation of the extensor tendon injuries of the phalanges, offering fast, accurate, and cost-efficient imaging for rehabilitation professionals. Its ability to provide real-time, dynamic assessments makes it particularly suited for rehabilitation providers who can integrate the MSK ultrasound findings into clinical decision-making, optimizing treatment strategies and improving patient outcomes. However, practitioners must be adequately trained to maximize it’s diagnostic potential. By integrating MSK ultrasound into practice, rehabilitation providers can enhance patient care, improve outcomes, and reduce the burden of false diagnoses or delayed treatment.