INTRODUCTION
Rehabilitation following anterior cruciate ligament (ACL) reconstruction is crucial for restoring knee muscle strength and facilitating a successful return-to-sport.1–4 However, despite rehabilitation, muscle strength deficits following ACL reconstruction are common.5,6 This is concerning, as muscle strength deficits are associated with reduced patient-reported knee function and lower return-to-sport rates among both recreational and competitive athletes.6–10 Therefore, optimizing muscle strength recovery following ACL reconstruction is essential.
Heavy-load resistance training (HLRT), using external loads of more than 60% of one-repetition maximum (1RM), is currently recommended to improve muscle strength.11 However, there are concerns that HLRT following ACL reconstruction may have detrimental effects on knee pain.12 Therefore, low-load blood flow restriction training (LL-BFRT), using external loads between 20 and 40% of 1RM, has been suggested as an alternative to HLRT.10,12 During LL-BFRT, a pressurized cuff is applied to the proximal thigh that occludes venous outflow while partially restricting arterial inflow.13,14 The combination of venous occlusion and low-load (20-40% of one repetition maximum) resistance training during LL-BFRT is believed to induce muscle hypertrophy secondary to muscle tension and metabolic stress.15,16 Studies suggest that LL-BFRT can achieve muscle strength gains comparable to HLRT while exerting less mechanical stress on the knee joint.17–20 Additionally, LL-BFRT has demonstrated positive effects on functional outcomes in ACL-reconstructed patients and is increasingly applied in sport rehabilitation settings to support return-to-sport.18,20 While most existing studies have focused on clinical outcomes following LL-BFRT or HLRT, limited attention has been given to how athletes experience and perceive these rehabilitation methods in practice. Since successful rehabilitation depends not only on clinical efficacy but also on patient experience and adherence, a qualitative evaluation is essential to determine whether these rehabilitation methods effectively support recovery and return-to-sport participation. This study aims to explore patients’ experiences with strength rehabilitation using LL-BFRT or HLRT following ACL reconstruction. These results will provide insights that can contribute to more patient-centered rehabilitation approaches and ultimately improve return-to-sport outcomes.
METHODS
Design
This descriptive qualitative study using an inductive thematic analysis approach complies with the Declaration of Helsinki and was approved by the medical ethical committee. Furthermore, this study was performed in accordance with the Consolidated Criteria for Reporting Qualitative Research.21 All patients provided informed consent before enrollment.
Participants
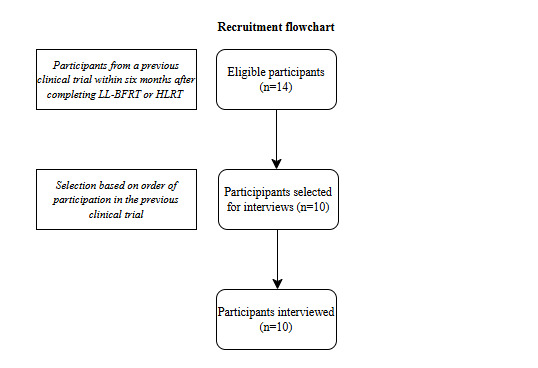
Participants were recruited from a clinical trial examining low-load blood flow restriction (LL-BFRT) and heavy-load resistance training (HLRT) following bone-patellar tendon-bone (BPTB) ACL reconstruction. The participants were contacted if they were within six months post-strength rehabilitation. Patients not willing or able to participate were excluded.
Additionally, patients with a history of venous thromboembolism, sickle cell anemia, hypertension or other relevant cardiovascular conditions were excluded from the study due to limited evidence regarding the safety of LL-BFRT in this population.22 The recruitment process and inclusion of participants are illustrated in Figure 1.
Surgical procedure
All participants underwent ACL reconstruction using an autologous BPTB graft. The anteromedial portal was used to place the femoral tunnel in the isometric anteromedial bundle position. The tibial tunnel was placed in the center of the native ACL footprint. This approach aligns with current concepts for achieving an anatomic tunnel placement and optimal ACL reconstruction.23 Titanium interference screws (Zimmer Biomet, Indiana, USA) were used for femoral and tibial graft fixation. Additionally, a modified Lemaire lateral extra-articular tenodesis (LET) was performed in patients with preoperative high-grade pivot shift or hyperlaxity.24 The surgical procedures were performed by high-volume ACL surgeons.
Strength rehabilitation protocol
All participants followed the same standardized rehabilitation program under the guidance of physiotherapists specialized in ACL rehabilitation. The only difference between groups was the type of strength intervention (LL-BFRT or HLRT), which was implemented between two and 14 weeks postoperatively. Two weeks after surgery, patients started a biweekly strength training protocol for 12 weeks if they had a knee range of motion of 0-90°, had no or minimal effusion during activity (defined as trace or 1+ based on the stroke test) and were able to perform repeated straight leg raises.12,25 The strength training included leg press, leg extension, deadlift and squat exercises, with 30 seconds of rest between sets and 120 to 180 seconds of rest between exercises. Blood flow restriction in the LL-BFRT group was achieved using an automatic tourniquet system (PTS; MAD-UP, Angers, France) designed to automatically calculate limb occlusion pressure. Limb occlusion pressure was defined as the minimum pressure required for arterial blood flow occlusion. Limb occlusion pressure of 80% was applied during each exercise and was determined in the position that the exercise was performed in. The cuff was inflated during each exercise and deflated during the 120 to 180 seconds of rest between exercises. Patients in the LL-BFRT group performed four sets per exercise, consisting of 30, 15, 15, and 15 repetitions, with 30 seconds of rest between sets while the cuff remained inflated. Each exercise was performed at 30% of 1RM.12–14 Patients in the HLRT group performed three sets (10, 10, 10 repetitions) of each exercise at 70% of 1RM.12–14 The 10RM strength was measured and used to predict 1RM strength.26 The external training load was increased by 10% if patients completed all repetitions on two subsequent strength training sessions.11
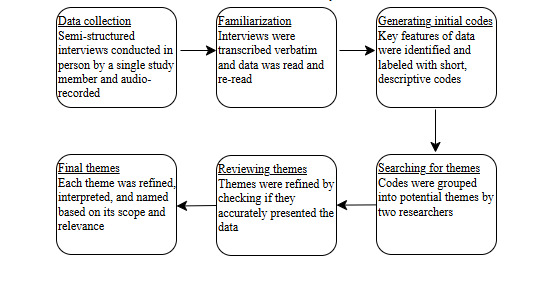
Data collection
Semi-structured interviews were conducted between May and June 2023 using an interview guide. The interview guide was based on a literature review and included topics and questions related to patents’ experiences with strength training (LL-BFRT and HLRT) (Supplemental File 1).18,27–30 A single study member conducted all in-person interviews, which were audio-recorded, transcribed verbatim and anonymized. Data saturation was reached when no new themes, insights, or dimensions emerged from the interviews.31 The number of participants depended on the time to saturation within every group. It was estimated that four participants per group would be sufficient to reach saturation. In total, ten participants were invited to participate in the study.
Data analysis
Demographic data, including age, gender, pre-injury Tegner score, trauma mechanisms, and concomitant treatments (such as partial meniscectomy and LET procedure), as well as patient satisfaction ratings (0-10, 10 very satisfied) were collected. An inductive thematic analysis was used to analyze the transcripts according to the six phases described by Braun and Clarke.32 One researcher read and coded the transcripts. After completion of the coding process, two researchers discussed and analyzed the codes to identify themes and subthemes of the study. These themes were then listed to ensure adequate representation of the data. An overview of the data collection and analysis process is presented in Figure 2.
RESULTS
A total of ten participants were included in the study, with five in the LL-BFRT group and five in the HLRT group (Table 1). Data saturation was reached after four participants per group, and this was confirmed after the fifth interview, as no new themes or dimensions emerged. The interviews were conducted, on average, four months after completing the strength rehabilitation protocol. Among the participants, six were male. The median age in the LL-BFRT group was 24.6 years (range 23-27), while in the HLRT group, it was 22.8 years (range 19-33). The median patient satisfaction rates were 8.5 (range 7.5-9.0) for the LL-BFRT group and 7.9 (range 7.0-9.0) for the HLRT group, respectively. In total four themes were identified: 1. experiences with strength training, 2. perceived benefits, 3. challenges encountered and 4. impact on the recovery process.
1. Experiences with strength training
The participants were satisfied with both strength protocols. They reported that physiotherapist-patient relationship, quality of physiotherapy care, expectations and results influenced their experience with strength training. “The experience of the physiotherapists and the personalized attention had a positive effect on my strength rehabilitation process” (Participant 2, HLRT group). The strength rehabilitation was acknowledged as challenging, yet all participants recommended the strength rehabilitation protocol to gain muscle strength. "The strength rehabilitation was intense, but the results exceeded my expectations" (Participant 1, LL-BFRT group).
2. Perceived benefits
All participants recognized a progression in muscle strength, stability and ability to undertake activities. The increase in muscle strength motivated the participants to continue with strength training. “I am pleased with the progress I have made in building muscle strength. I have more confidence in my knee” (Participant 4, HLRT group). In addition, with the exception of two participants in the HLRT group, all participants experienced a decrease in pain and increase in knee confidence during strength rehabilitation. “I had less knee pain, and I was more confident than at the start of my rehabilitation” (Participant 3, LL-BFRT group).
3. Challenges encountered
All participants stated that the strength rehabilitation program was challenging. Three participants in the LL-BFRT group noted thigh muscle pain during strength rehabilitation. Furthermore, one participant in the LL-BFRT fainted during the first training session. "The cuff pressure on my thigh was intense and I fainted during the first training session" (Participant 2, LL-BFRT group). In the HLRT group, two participants reported knee pain during strength rehabilitation, with two other participants reporting knee pain during and after strength rehabilitation. “I noticed significant knee pain during and following my strength training program” (Participant 2, HLRT group).
4. Impact on recovery process
All participants experienced positive effects on their recovery process, except for two participants in the HLRT group who experienced negative effects with a delayed recovery process. Participants who reported positive effects on their recovery process stated to be able to bear weight without crutches within six weeks, run without pain or swelling within 14 weeks and return to on field rehabilitation within 20 weeks post-surgery. "I felt stronger and more confident thanks to my muscle strength gains. I started on field rehabilitation four months after ACL reconstruction" (Participant 4, LL-BFRT group). Participants who reported negative effects on their recovery process stated that they were able to bear weight without crutches 10-12 weeks after surgery and were not able to run without pain. “Knee pain prolonged my rehabilitation and restricted the ability to perform kneeling activities” (Participant 3, HLRT group). The positive effects on the recovery process were the result of pain-free return to activities, unrestricted range of motion, improved muscle strength, confidence in the knee and improved physical performance. The negative effects on the recovery process were due to knee pain during and after activities.
DISCUSSION
This qualitative study showed high patient satisfaction with low-load blood flow restriction training (LL-BFRT) and heavy-load resistance training (HLRT) following anterior cruciate ligament (ACL) reconstruction. In addition, all participants reported improvements in muscle strength. However, differences were noted in the challenges faced and the overall impact on recovery.
Patient satisfaction was high for both LL-BFRT and HLRT, with all participants completing and recommending these rehabilitation protocols. Participants emphasized the importance of the physiotherapist-patient relationship, the quality of physiotherapy care, and the alignment of their expectations with their outcomes. These factors influenced their satisfaction with both LL-BFRT and HLRT protocols.
All participants experienced improvements in muscle strength, which is consistent with the results of previous studies examining the effectiveness of these rehabilitation methods after ACL reconstruction.33,34 In addition to the literature, the present study found that some participants experienced an improvement in knee confidence with both LL-BFRT and HLRT. This finding is significant because knee confidence can influence patient behavior, impacting rehabilitation outcomes such as adherence to physiotherapy sessions and training effort.35
Both strength rehabilitation protocols were perceived as challenging by all participants. However, side effects varied between the two groups. In the LL-BFRT group, one participant reported a temporary loss of consciousness during the first session, and three participants experienced thigh muscle pain during training. In the HLRT group, two participants reported knee pain during training, while two other participants noted knee pain both during and after training. Fainting during LL-BFRT is rare, with reported incidence in the literature being less than 4%.36 Hogan et al. suggested that fainting could result from a mismatch between cardiac output, sympathetic control of the vasomotor system, and local mechanisms of hyperemia.37 LL-BFRT may affect cardiac output by reducing the cardiac preload due to venous occlusion generated by the application of a pressurized cuff on the thigh.17 If an individual’s compensation mechanisms are insufficient, these changes could lead to fainting. However, in individuals without underlying medical conditions, fainting could also be triggered by stress or anxiety from cuff tightness or pain. The authors speculate that stress or anxiety could have contributed to the young female participant’s fainting in this study. Additionally, thigh muscle discomfort during LL-BFRT might be influenced by factors such as cuff pressure and inflation time.38–40 Participants in this study followed an LL-BFRT protocol based on current evidence recommending a cuff pressure between 40 and 80% of limb occlusion pressure (LOP) and intermittent blood flow restriction with 30 seconds of rest between sets.38 All participants of the present study following the LL-BFRT protocol had their cuff pressure set at 80% of LOP. A recent study using the same LOP setting showed that in 4% of training sessions a decrease in pressure was needed due to pain.41 Additionally, a recent systematic review demonstrated significant results on muscle strength when LL-BFRT was performed with LOP between 40 and 80%.42 Based on this evidence, the authors recommend using an individualized LOP between 40 and 80%. In contrast to LL-BFRT, knee pain was commonly reported in the HLRT group. Two participants experienced knee pain during HLRT, while two other participants noted knee pain both during and after training. These findings are consistent with previous studies.12,33,43 This may be the result of higher mechanical stress to the knee joint with HLRT by using higher external loads compared to LL-BFRT. Furthermore, the use of LL-BFRT may enhance the analgesic effects of exercise-induced hypoalgesia.44–46
Rehabilitation is vital for ensuring a successful recovery and follows a criteria-based progression that begins with controlling symptoms such as knee pain and effusion.1–4 Once these are managed, the focus shifts to rebuilding muscle strength and neuromuscular control, ultimately progressing to functional and sport-specific training.1–4 However, pain and effusion management remain essential throughout each phase of the rehabilitation.1–5 Failure to maintain control over these symptoms can negatively impact recovery, potentially hindering an athlete’s readiness and ability to return-to-sport at the desired performance level.47–51 All participants who adhered to the LL-BFRT protocol reported a beneficial impact on their recovery process. In contrast, two participants in the HLRT group experienced delayed recovery due to knee pain. As LL-BFRT promotes muscle strength while minimizing mechanical stress on the knee joint, this method may positively influence pain management, overall recovery, and ultimately enhance return-to-sport outcomes compared to HLRT. Nevertheless, to date there is no data available on the effects of LL-BFRT on functional performance assessments and return-to-sport rates in comparison to HLRT.
The present study has several limitations. First, the small sample size may limit the generalizability of the findings of the present qualitative study. However, the study reached data saturation with consistent and recurring themes in athletes’ experiences with LL-BFRT and HLRT, supporting the strength of the current findings. Secondly, the interviews were conducted, on average, four months after completion of the strength rehabilitation protocol with the potential of recall bias. Given that all participants received a bone-patellar tendon-bone (BPTB) graft for ACL reconstruction, the findings may not fully translate to populations treated with other graft types. This should be considered when interpreting the study’s outcomes. Finally, factors like graft morbidity and psychological factors such as beliefs (e.g. placebo-effect), stress and coping mechanisms may affect knee pain and were not assessed in the present study. However, this is the first study assessing patients’ experience with LL-BFRT and HLRT allowing participants to express their experiences in greater depth and detail.
CONCLUSION
The results of the present study provide valuable insights to enhance patient-centered strength rehabilitation following ACL reconstruction. Findings indicate that LL-BFRT may be more suitable in the early rehabilitation phase, as knee pain in the HLRT group may negatively affect the recovery process. However, further studies are needed to evaluate the role of LL-BFRT and HLRT on functional performance and safe return to sport after ACL reconstruction.
Corresponding author
Baris B Koc
Ziekenhuis Oost-Limburg, Synaps Park 1, 3600 Genk, Belgium
+32 484 19 12 24
baris.koc1991@gmail.com