Introduction
The rate of anterior cruciate ligament (ACL) tears is increasing in youth athletes with an estimated 400 injuries per 100,000 person-years reported in adolescents.1 Injury to the ACL often results in extended time away from sport and significant healthcare costs.2 Athletes who return to sport are also at high risk of sustaining a second ACL injury during their career, with secondary reinjury rates of up to 20% reported.3 Most ACL injuries are sustained during landing or deceleration phases of sport activity with approximately 80% of injuries classified as non-contact, or involving minimal to no contact.4,5 As ACL injury rates and subsequent surgical intervention continue to increase, injury and reinjury risk screenings are evolving to address these complications. Current screenings aim to assess common mechanisms of ACL injury while incorporating dynamic movements that simulate the sport environment. Specifically, the drop vertical jump (DVJ) task is frequently utilized to evaluate biomechanics related to increased risk of ACL injury. Tools such as the Landing Error Scoring System (LESS) have been validated to visually identify high risk movement patterns during a DVJ,6,7 but it is unknown whether these assessments capture realistic mechanics and loading forces similar to those experienced during in-game sport activity.6,8
The high rate of non-contact ACL injuries highlights how a lack of neuromuscular control during high risk movements may impact injury risk.5 While some factors associated with increased ACL injury risk, such as age, knee morphology, and rotational or anterior-posterior knee laxity, are non-modifiable,8,9 lower extremity biomechanics, specifically movement strategies to mitigate loading forces at the knee, can be modified.10 The knee valgus collapse is a common mechanism of ACL injury during loading.11,12 Contributors to valgus collapse, including hip adduction, hip internal rotation, and knee abduction, are commonly assessed to determine the quality of landing patterns.6,13 Current screening tools, such as the LESS, are designed to assess the first landing of the DVJ to identify potential injury risk. However, it has been shown that the second landing of a DVJ, following the maximum vertical jump, may better simulate the mechanism of non-contact ACL injury sustained during games.14,15 Thus, current screening methods that utilize the DVJ task may require design modifications to better represent in-game mechanics.
Previous researchers have examined the first and second landings of the DVJ in healthy, adolescent, female basketball players.14,15 Their results indicated that the second landing elicited greater side-to-side differences,14 or limb asymmetry, compared to the first landing, which has been established as a risk factor for injury.16 Findings also indicated decreased hip and knee flexion angles and moments were exhibited during the second landing. Since stiffer landings with less hip and knee flexion have been shown to elicit greater injury risk with less shock absorption,15,17 this may indicate a reduced protective landing strategy during the second landing. These findings highlight the potential utility of evaluating the second landing of the DVJ when screening for injury risk or RTP readiness.
No data have been published comparing the mechanics of the first and second landings of a DVJ for athletes who have undergone ACL reconstruction. Investigation into the clinical utility of each landing would allow for a more comprehensive assessment of RTP readiness and of secondary injury risk. Therefore, the purpose of this study was to compare biomechanical risk factors in the first and second DVJ landings in both the surgical (affected) and unaffected limbs in youth athletes recently cleared for RTP following ACL reconstruction. It was hypothesized that the second landing would better represent mechanics associated with ACL injury risk, and that greater asymmetry between limbs would occur in the second landing.
Methods
Participants
Male and female youth athletes, ages 12-19 who had undergone an ACL reconstruction and were granted RTP clearance from their physician were recruited to participate in this study. Date range for enrollment was between 2020 and 2024. Participants were excluded if they reported experiencing or were diagnosed with any musculoskeletal or neuromuscular conditions, in addition to the recent ACL injury, or were unable to perform the DVJ task. Approval from a regional Institutional Review Board (University of Texas Southwestern Institutional Review Board, Dallas, TX, USA) was obtained prior to initiating study procedures. Upon enrollment, informed consent/assent was obtained from all patients and parents, if applicable, prior to participation. All participants wore their personal athletic footwear and attire to allow familiarity and natural mechanics during testing conducted in a motion capture laboratory. Participants were provided with closed-toed, athletic footwear if deemed appropriate.
Procedures
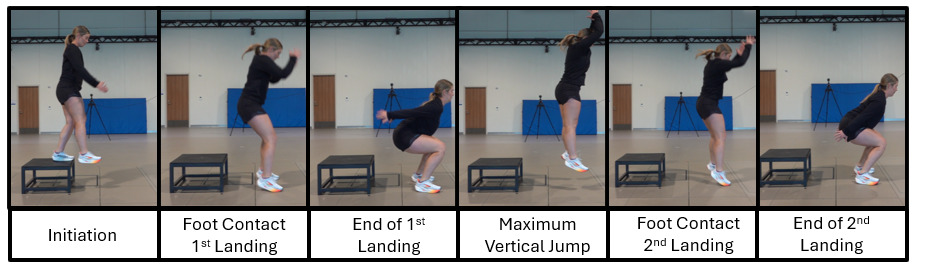
Participants were instrumented with retroreflective markers according to a modified Cleveland Clinic marker set18 which included lateral thigh clusters, anterior shank clusters and a 5th metatarsal marker.19,20 A 14-camera motion capture system (Vicon Motion Systems Ltd, Denver, CO, USA) with integrated force plates (Advanced Mechanical Technology Inc., Watertown, MA, USA) was used to collect marker and force plate data sampling at 240 Hz and 2,880 Hz, respectively. Data were collected while participants performed a series of dynamic tasks which included a DVJ. Verbal instructions were standardized to the participants to “Jump off both feet from the box. Hop forward (not up) and land with one foot in each square. Then, immediately jump up as high as you can and land back down with one foot in each square. Complete the entire task in one fluid motion”.20,21 Per standardized instructions, no cues were provided for how to perform the second landing. The jump was performed from a 31-cm-tall plyometric box onto two 60cm x 60cm square force plates with a jump distance of one-half of the participant’s height from the front of the box to the center of the force plates (Figure 1).21,22 Task setup and instructions were designed to reflect the LESS which is a common test used for identifying poor movement quality and determining RTP readiness.23 Three successful DVJ trials were collected for each participant to capture natural mechanics with a representative trial selected from each participant based on task performance, defined as jump height. Jump height was measured as the difference of the sacral marker in the static standing trial versus max height during DVJ trials and the trial with the greatest jump height was chosen to be included for analysis.21,22 A trial was deemed successful if the participant completed the trial according to verbal instructions, and an unsuccessful trial was noted if the participant did not land with one foot in each force plate during either the first or second landings or failed to perform maximal vertical jump following the first landing.
Data Processing and Analysis
Trials were processed in Vicon Nexus (OMG plc, Oxford, UK). A Woltering filter was applied to marker trajectories with a predicted mean square error of 10mm2, and force plate data were filtered using a 4th-order low-pass Butterworth filter with a cut-off frequency of 16 Hz.24 Trunk and pelvis segment angles and hip, knee, and ankle joint angles and moments were computed using a custom MATLAB (MATLAB 2022a, Natick, MA, USA) model. Trunk and pelvis segment angles were defined relative to the global coordinate system. External lower extremity joint kinetics were computed using inverse dynamics and normalized to body mass (in kilograms). Data from both limbs were used for subsequent analysis and defined as either “affected” (surgical limb) or “unaffected” (non-surgical) limb.
The descent phase for the first and second landings of the DVJ were determined by a custom MATLAB code that automatically identified the time points for initial foot contact and maximum descent for both landings.25 Peak trunk and pelvis angles, as well as peak lower extremity angles and moments were extracted for analysis across the descent phases of both the first and second landings.
Statistical Analysis
Mean and standard deviations were computed for all continuous measures, including age, height, weight, and all kinematic and kinetic peak measures. Given significant Shapiro-Wilk tests of normality, non-parametric analyses were performed. Specifically, to determine significant differences between the first (1st) and second (2nd) DVJ landings, as well as between the affected (AFF) and unaffected (UNAFF) limbs, Wilcoxon signed-rank tests were performed. Subsequently, effect sizes (r) were computed for all significant comparisons and interpreted as small (0.10), moderate (0.30), or large (≥ 0.50).26 All statistical tests were evaluated in SPSS Statistics (IBM, version 24.0, Armonk, NY, USA) with a significance level (α) of 0.05. Additionally, to control for multiple comparisons across biomechanics measures, a Holm-Bonferroni correction was applied within each comparison group, adjusting p-values to maintain the family-wise error rate at α = 0.05.
Results
A total of 58 participants (37 females, 21 males; 15.9 ± 1.9 years; 164.0 ± 9.5 cm; 66.0 ± 15.3 kg) were included for analysis (Table 1). Kinematic and kinetic measures from the first and second landing of both the affected and unaffected limbs during the DVJ are presented in Table 2 and Table 3, respectively.
Trunk and Pelvis
Increased trunk flexion (AFF: p < 0.001, r = -0.82; UNAFF: p < 0.001, r = -0.82) and anterior pelvic tilt (AFF: p = 0.002, r = -0.48; UNAFF: p = 0.002, r = -0.49) were observed during the first landing compared to the second landing. Similarly, ipsilateral pelvic drop (p < 0.001, r = -0.55) and internal pelvic rotation (p < 0.001, r = -0.75) were greater during the first landing on the unaffected limb. Between limbs, ipsilateral pelvic drop (p = 0.033, r = -0.39, mean difference: 1.85 degrees) and internal pelvic rotation (p = 0.003, r = -0.49, mean difference: 4.57 degrees) were greater on the unaffected limb compared to the affected limb during the first landing.
Hip
There were several significant findings for the hip comparing the first and second landings. Specifically, hip flexion (AFF: p < 0.001, r = -0.82; UNAFF: p < 0.001, r = -0.79), hip abduction AFF: p < 0.001, r = -0.13; UNAFF: p = 0.005, r = -0.39), hip internal rotation (AFF: p < 0.001, r = -0.61; UNAFF: p < 0.001, r = -0.90), hip flexion moment (AFF: p < 0.001, r = -0.81; UNAFF: p < 0.001, r = -0.80), and hip internal rotation moment (AFF: p < 0.001, r = -0.66; UNAFF: p < 0.001, r = -0.59) were increased during the first landing on both limbs. Hip adduction moment was increased during the first landing on the affected limb only (p = 0.023, r = -0.40). Between limbs, there was a greater hip adduction moment on the unaffected limb during both the first (p = 0.003, r = -0.48, mean difference: 0.26 Nm/kg) and second (p = 0.009, r = -0.45, mean difference: 0.27 Nm/kg) landings.
Knee
During the first landing, the knee elicited greater flexion (p < 0.001, r = -0.74), valgus (p = 0.001, r = -0.50), and external rotation (p < 0.001, r = -0.58) in the unaffected limb while greater flexion (p < 0.001, r = -0.71) and valgus (p < 0.001, r = -0.67) were observed in the affected limb. Comparing limbs, knee flexion (1st: p = 0.001, r = -0.45, mean difference: 2.06 degrees; 2nd: p = 0.019, r = -0.42, mean difference: 1.74 degrees), flexion moment (1st: p < 0.001, r = -0.82, mean difference: 0.64 Nm/kg; 2nd: p < 0.001, r = -0.79, mean difference: 0.57 Nm/kg) were greater for the unaffected limb during both landings. Conversely, knee external rotation (p = 0.036, r = -0.39, mean difference: 2.87 degrees) was increased on the affected limb during the second landing and external rotation moment (1st: p = 0.012, r = - 0.44, mean difference: 0.03 Nm/kg; 2nd: p = 0.004, r = -0.48, mean difference: 0.03 Nm/kg) was increased on the affected limb during both the first and second landing.
Ankle
At the ankle, dorsiflexion moment was significantly greater during the first landing, bilaterally (AFF: p < 0.001, r = -0.56; UNAFF: p = 0.001, r = -0.50). Likewise, between limbs, the unaffected limb demonstrated greater dorsiflexion (1st: p < 0.001, r = -0.69, mean difference: 4.48 degrees; 2nd: p < 0.001, r = -0.61, mean difference: 2.88 degrees) and dorsiflexion moment (1st: p < 0.001, r = -0.70, mean difference: 0.18 Nm/kg; 2nd: p = 0.019, r = -0.43, mean difference: 0.17 Nm/kg) for both the first and second landings.
Discussion
The purpose of this study was to compare kinematics and kinetics of the first and second DVJ landings in both affected and unaffected limbs in youth athletes recently cleared for RTP following an ACL reconstruction. Significant differences in biomechanical risk factors were demonstrated between landings as well as between limbs. There were a greater number of biomechanical risk factors associated with dynamic knee valgus in the first landing, specifically knee valgus, hip internal rotation, knee external rotation, and hip adduction moment. Overall, more biomechanical risk factors were noted to be significantly greater in the unaffected limb compared to the affected limb in both the first and second landings, indicating potential compensation techniques or inherent differences in these athletes. While statistically significant, most of these limb differences were less than 3 degrees, which may not be clinically measurable or seen as clinically significant. However, findings indicate moderate to large effect sizes among statistically significant comparisons, suggesting meaningful differences between landings and limbs.
These findings suggest that both limbs continue to demonstrate altered biomechanics following ACL reconstruction, which could indicate deficits in neuromuscular control, strength, proprioception, and compensatory strategies during deceleration tasks like the jump landing. Previous researchers have emphasized the importance of evaluating limb asymmetry16,27 and compensatory loading strategies11,28,29 as risk factors for secondary injury. For example, reduced knee flexion seen in the affected limb has been shown to be associated with greater frontal plane knee motion, including knee valgus and knee valgus moments.30 With decreased sagittal plane motion and subsequent increases in frontal plane motion, there is an observed decrease in shock absorption during landing.30 Increased knee flexion and knee flexion moment in the unaffected limb may indicate compensatory overloading, potentially placing the contralateral limb at risk for injury, which has been shown to be fifteen times more likely to occur in athletes who have undergone primary ACL reconstruction.31,32
Increases in knee external rotation and external rotation moment in the affected limb may suggest changes in rotational control at the hip and/or knee, which have been established as contributors to dynamic knee valgus and increased injury risk in the ACL.11,27 The changes in motor control at key knee stabilizing muscle groups that occurs following ACL reconstruction could be a possible cause for this decreased rotational control at the knee during landing.33,34 Previous literature discusses ligament dominance, or reliance on passive structures such as the ACL following this decrease in muscle strength or neuromuscular control. This ligament dominance may contribute to biomechanical components of dynamic knee valgus and decreases in stability with absorption phases of sports activities. It has been shown that this increase in knee external rotation can compromise dynamic control and increase ligamentous strain during landing.35,36 Postoperative strength deficits at the hip and knee may further contribute to alterations in loading at the knee.10,37 In addition to this neuromuscular inhibition following ACL reconstruction, others have emphasized a change in proprioception following damage to mechanoreceptors within the ACL.34 This alteration in proprioception can impair joint position sense and reduce the ability to control rotation during activity. As loading strategies, neuromuscular control, strength, and proprioception are modifiable risk factors for ACL injury, this highlights the role of physical therapy in addressing the biomechanical deficits and compensatory strategies in both limbs during loading phases of sports activity prior to RTP.
Overall, decreases in hip and knee flexion during the second landing indicate a stiffer landing, which has been shown to associated with greater vertical ground reaction forces and increased risk of ACL injury.17 Likewise, a stiffer landing has been shown to be more representative of in-game mechanics14,15 where ACL injuries are more likely to occur.3,38,39 Current assessments, such as the LESS, focus predominantly on the first landing of the DVJ, but results of this study indicate that biomechanical markers of the first landing alone may not fully capture risk factors following ACL reconstruction. With a greater amount of biomechanical risk factors observed in both limbs during the first landing and a stiffer overall second landing, these findings highlight the need for a comprehensive DVJ assessment of both landings and both limbs for evaluation of RTP readiness.
Limitations
Several limitations should be noted in this study. First, the cohort included an uneven sample size of male and female participants. The uneven distribution of male and female participants may limit generalizability of findings, particularly since previous researchers have noted significant differences in landing force and drop vertical jump performance between males and females.40,41 Specifically, males have been shown to demonstrate increased landing force attenuation capacity40 and females have demonstrated greater knee valgus during landing tasks.42 Additionally, the mechanism of injury (contact versus non-contact) was not collected and therefore could not be included for analysis in this study. Previous researchers have identified differences in biomechanical risk factors for sustaining a non-contact ACL injury.43,44 Moreover, inherent differences in muscle length and strength between groups may contribute to performance on the DVJ. Future work should collect injury mechanisms and explore effects of muscle differences on biomechanical risk factors.
The current study did not utilize a control group to compare inter-limb differences in a healthy population. The absence of a healthy control group limits the ability to contextualize observed asymmetries, however previous researchers have reported limb asymmetry in healthy populations based on limb dominance.45 Furthermore, researchers have previously noted greater kinetic asymmetry during a drop vertical jump in adolescents with a history of ACLR compared to healthy controls.46 Future work should further investigate the differences in the presence of biomechanical kinematic and kinetic risk factors between adolescents who have undergone ACLR and their healthy peers.
As highlighted in previous literature, performance on the DVJ as it relates to joint angles and moments at the trunk, hip, knee, and ankle is directly impacted by task instruction.21,47–50 One limitation of this study is that standardized instructions to “Jump off both feet from the box. Hop forward (not up) and land with one foot in each square. Then, immediately jump up as high as you can and land back down with one foot in each square. Complete the entire task in one fluid motion” emphasized instructions through completion of the first jump landing, but not the second. While lack of instruction can mimic game-like performance of a non-anticipated second jump landing, further research is needed to determine if verbal instructions that include both landings alter performance on the second landing of the DVJ.
Similarly, DVJ task protocol variation has been shown to impact lower body kinematics and kinetics.21 Some studies have utilized a standard horizontal jump distance, while others have normalized horizontal jump distance to participants’ body height or baseline jump performance.51,52 In addition to distance, variation in DVJ protocol as it relates to vertical jump height also exists, where some researchers have normalized vertical jump height to participants’ body height53,54 and others have a standardized jump height (30 cm; 12 in).6 However, previous literature has shown that jump height of the DVJ influences biomechanical risk factors,55,56 thus, jump height (31 cm plyo box) and distance (% body height) were controlled in the current study. Due to the influence of jump height and distance in DVJ protocol variations on joint kinematics and kinetics, current findings may not apply to all variations of DVJ protocol. Previous literature has shown that limb dominance affects biomechanical behaviors during landing tasks.45,57–61 While the current study was designed to assess affected and unaffected limbs following ACL reconstruction, limb dominance was not considered in analysis of biomechanical risk factors.
Conclusion
At RTP, significant kinematic and kinetic differences occurred both between first and second landings of the DVJ and between affected and unaffected limbs in adolescent athletes who had undergone ACL reconstruction. While less significant biomechanical risk factors occurred during the second landing, both the first and second landing of the DVJ elicited biomechanics associated with increased risk of ACL injury. A greater number of statistically significant differences were observed in the unaffected limb, suggesting continued asymmetry and compensatory landing strategies following ACL reconstruction that may contribute to increased risk of secondary injury. Given the findings of the current study, the authors recommend a comprehensive RTP assessment following ACL reconstruction with considerations of both landings and both limbs during the DVJ.
Corresponding Author
Katie M Sloma, PT, DPT, CSCS
Movement Science Lab Frisco
Scottish Rite for Children
Frisco, TX 75034, USA
Telephone: 469-515-7157
Fax: 254-296-8154
Email: katie.sloma@tsrh.org
Conflicts of Interest
The authors declare no conflicts of interest related to this manuscript.