Introduction
Baseball is a widely played popular sport in Japan, with a large number of participants at the youth level. Upper limb injuries, such as those affecting the shoulder and elbow, are common in baseball, and low back injuries are frequent.1,2 Recent systematic reviews and meta-analyses have reported a high prevalence of low back pain (LBP) in adolescent athletes (1-year prevalence: 29–55%), and identified risk factors, such as overweight/high body mass index (BMI), sport participation, and training volume/intensity.3
A survey of university athletes found that baseball players had the second highest prevalence of LBP after volleyball players, with an odds ratio (OR) 3.2 times higher than that of non-athletes for lumbar disc degeneration.4 A cross-sectional study of high-school baseball players revealed that 49.1% experienced LBP, with 20.3% classified as having chronic LBP (CLBP).5 Similarly, more than 30% of university baseball players reported experiencing LBP.6 These findings indicate that LBP is highly prevalent among Japanese baseball players.
Previous systematic reviews and meta-analyses have shown a correlation between an elevated BMI and the severity of LBP in the general adult population.7,8 This suggests that body composition may be an important factor for evaluating the risk of LBP, even among athletes. In cases of CLBP, specific physical or body composition characteristics, such as high body fat or low muscle mass levels, may increase the load on the lumbar spine and serve as contributing factors. Additionally, baseball players are exposed to repetitive and asymmetrical trunk movements during pitching and hitting, which generate substantial torsional and compressive forces on the lumbar spine.9 These biomechanical stresses may elevate the risk of spinal injury, particularly in the presence of physical factors, such as inadequate muscular support or excess adiposity.
Body composition is typically categorized into fat, fat-free, and bone mass. In athletic populations, assessments usually emphasize fat mass and lean mass, often expressed as relative measures, such as percentage body fat (PBF) and fat-free mass (FFM) index (FFMI), to account for differences in body size and height.
Studies of ice hockey and rugby players have reported associations between body composition and LBP, particularly in relation to the size and fat content of the multifidus muscles.10,11 In ice hockey players, higher PBF has been significantly correlated with smaller multifidus muscle size, suggesting that increased fat mass may hinder muscle development and elevate mechanical stress on the lumbar region.10Similar associations between muscle characteristics and LBP have been observed in rugby players.11
In contrast, few studies have examined the relationship between body composition and LBP in baseball players.5 Given that CLBP may be influenced by specific physical characteristics, including body fat distribution, a more detailed evaluation of body composition in this population is warranted. Therefore, the purpose of this study was to investigate the relationship between body composition parameters and the presence of chronic low back pain (CLBP) in high-school baseball players.
Materials and Methods
This retrospective cohort study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Review Board of Osaka Kawasaki Rehabilitation University (Approval No. OKRU-RA0003). Written informed consent was obtained from all the participants and their guardians, and additional consent was obtained from the team manager.
Participants
All participants were male high school baseball players from a school in Japan. All players trained six days per week, averaging approximately four hours per day. During the winter off-season (December to February), training emphasized running, strength training, and batting practice, with reduced pitching activity.
Players were recruited during their team’s annual medical assessments. Inclusion criteria were participation in regular team training, and completion of both first-year and second-year assessments. Players who reported low back pain lasting for more than three months in their second year, and meeting the clinical definition of chronic low back pain (CLBP; pain intensity ≥ 3 on the numerical rating scale persisting for at least 12 weeks) were assigned to a CLBP group.12 Players who reported no low back pain during either year were assigned to a non-low back pain group.
Exclusion criteria were (1) a history of low back pain not meeting the definition of CLBP, and (2) incomplete survey data. All participants and their guardians provided written informed consent, and additional permission was obtained from the team manager.
Questionnaire
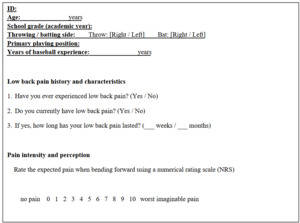
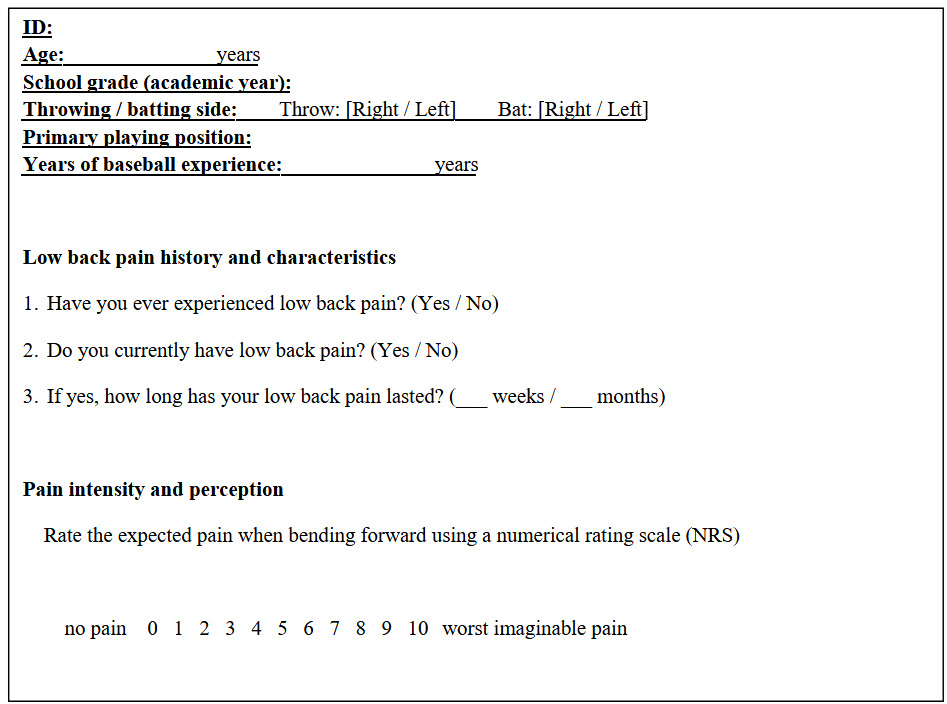
A self-administered questionnaire was used to assess the presence and intensity of LBP and gather baseball-related information. The questionnaire collected information on baseball experience (years) and primary playing positions (pitcher, catcher, infielder, and outfielder).
Players were informed in advance that their responses would not be shared with the coaches or team staff.
Pain intensity was measured using a visual NRS, ranging from 0 (“no pain”) to 10 (“worst imaginable pain”). LBP history and current symptoms were assessed separately to distinguish past and ongoing pain. The questionnaire used in this study is shown in Appendix 1.
Body Composition
Body composition data collected during the first year of high school were analyzed retrospectively. A bioelectrical impedance analyzer (InBody 270; InBody Co., Ltd., Seoul, Republic of Korea) operating at frequencies of 20 and 1000 kHz was used. The following parameters were recorded:
Anthropometrics included: Height (measured using a portable stadiometer), weight, and BMI; Lean and fat mass metrics: Soft lean mass, FFM, skeletal muscle mass (SMM), and body fat mass (BFM).Segmental analysis included: Lean and fat masses of the right and left arms, trunk, and right and left legs. Indices including PBF, SMM index, FFMI (FFMI = FFM/height²), and BFM index (BFMI = BFM/height²) were measured using the InBody 270. The InBody 270 has been previously validated for reliability and accuracy in estimating body composition across diverse populations, demonstrating high agreement with reference methods, such as dual-energy X-ray absorptiometry.13,14
Statistical Analysis
Statistical analyses were performed using the IBM SPSS Statistics version 27.0 (IBM Corp., Armonk, NY, USA). Statistical significance was set at p<0.05. Normality of distribution was assessed using the Shapiro–Wilk test. Between-group comparisons were performed using the chi-square test for categorical variables, Student t-test for continuous variables, and the Mann–Whitney U test for ordinal variables. Effect sizes for parametric comparisons were calculated using Cohen’s d to quantify the magnitude of between-group differences, interpreted as small (≥0.2), medium (≥0.5), and large (≥0.8) according to conventional benchmarks. Effect sizes were not calculated for variables analyzed with non-parametric tests due to distributional assumptions. Multivariate logistic regression was performed for variables that demonstrated significant differences in the univariate analysis. The dependent variable was the presence of CLBP, and body composition parameters were selected as independent variables. A forward stepwise model selection method was used. Model significance was evaluated using the model chi-square test, and model fit was assessed using the Hosmer–Lemeshow test, with p≥0.05 indicating a good fit.
Results
Of the 122 players initially surveyed, 27 were excluded because they reported LBP in the first year but no symptoms in the second year, while five were excluded due to incomplete questionnaire responses. The final analysis included 90 players: 31 (34.4%) and 59 (65.6%) in the CLBP and non-LBP groups, respectively. The mean (SD) age of all participants was 16.8 (0.4) years, with no significant difference between groups. Figure 1 presents the flowchart of participant inclusion and analysis.
Questionnaire Results
Table 1 summarizes the questionnaire results including age, years of baseball experience, playing position, and NRS score. Age, baseball experience, and position distribution did not differ between the two groups. However, the NRS scores in the CLBP group in both the first and second years were significantly higher compared to those in the non-LBP group (p < 0.001).
Body Composition Results
Table 2 shows a comparison of body composition between the CLBP and non-LBP groups. The CLBP group had significantly higher values of PBF, BFM, BFMI, and trunk fat mass. The effect sizes for these differences were large for PBF (d=3.24) and BFM (d=2.81), and moderate for trunk fat mass (d=1.68) and BFMI (d=0.93), indicating substantial between-group differences in fat-related measures.
Logistic Regression Analysis
Table 3 presents the results of logistic regression analysis for CLBP. The analysis identified the first-year NRS score and PBF as significant independent risk factors for CLBP (NRS score [first year]: B=0.773, standard error [SE]=0.201, Wald=14.766, OR, 2.16; 95% confidence interval [CI]: 1.46–3.21, PBF: B=0.235, SE=0.093, Wald=6.384, p<0.001, OR=1.26; 95% CI: 1.05–1.51). The model showed a good fit based on the Hosmer–Lemeshow test (p<0.05), and the overall classification accuracy was 78.2%.
Discussion
This study retrospectively examined risk factors for CLBP in high-school baseball players, focusing on body composition and pain intensity. The results identified PBF and first-year NRS scores as significant predictors of CLBP.
Several fat-related parameters—including PBF, BFM, and BFMI—were significantly higher in the CLBP group than in the non-LBP group. Notably, effect sizes for PBF (Cohen’s d=3.24) and BFM (Cohen’s d=2.81) were large, indicating that these differences were not only statistically significant but also of substantial practical relevance. These findings suggest that excessive fat accumulation may contribute to the development or persistence of CLBP in adolescent athletes by increasing mechanical load on the lumbar spine or altering spinal biomechanics. Increased abdominal fat may elevate anterior shear forces on the lumbar spine, shift the center of gravity forward, and increase lumbar lordosis.15,16
The body composition results align with prior studies. Uchida et al. reported an average PBF of 17.6% in experienced high-school baseball players,17 while Hikihara et al. reported 15.7%.18 Although PBF values vary slightly across studies, the present results (CLBP: 14.5%; non-LBP: 12.4%) are consistent with these findings.Elevated PBF in the CLBP group may be linked to mechanisms proposed in previous research, suggesting that adipose tissue contributes to pain.19 Excess fat can induce chronic low-grade inflammation, with adipose tissue secreting cytokines, such as tumor necrosis factor-α, adiponectin, and interleukins.20 In obesity, these cytokines may promote chronic inflammation, intervertebral disc degeneration, and muscle catabolism,21 all associated with CLBP.
Furthermore, trunk fat mass was significantly higher in the CLBP group. Given that the trunk supports spinal movement and posture, excess fat in this region may contribute to mechanical overload and back pain. Body composition in athletes can fluctuate seasonally and be influenced by training type, duration, and sport-specific demands.22,23 As body composition was measured during the off-season after several months of regular training, individual differences in training adaptation may have contributed to the observed variability. Personalized training tailored to body composition profiles may help reduce CLBP risk. According to recent systematic reviews and meta-analyses, resistance training programs lasting 14 weeks or longer are effective in reducing percentage body fat in youth populations. Moderate to high intensity exercise is generally recommended to improve body composition outcomes.24
Additionally, first-year NRS scores were a significant predictor of CLBP. Shafshak et al. reported that an NRS score >3 was associated with moderate functional disability, as measured by the Modified Oswestry Disability Index.12 In the current study, the average NRS score increased from 3.1 in the first year to 3.3 in the second year among participants with CLBP, suggesting that a score ≥3 may indicate a higher risk of developing chronic pain symptoms rather than directly predicting chronicity.
This study has several strengths, including objective measurement of body composition and a homogeneous sample of adolescent baseball players. However, several limitations should be considered. The retrospective design limits causal inference; body composition was assessed only once; and data on physical maturation, specific training volume, or lumbar structural integrity (e.g., imaging or functional muscle assessment) were not collected.
Conclusion
The results of this study indicate that higher percentage body fat and elevated baseline pain intensity may contribute to the development of chronic LBP in adolescent male baseball players. These findings should be interpreted in light of the study’s retrospective design and the absence of training and data on physical maturation and imaging.
Corresponding Author
Hidetoshi Nakao
Department of Physical Therapy, Faculty of Social Work Studies, Josai International University
1 Gumyo, Togane City, Chiba 283-8555, Japan
Email: h_nakao@jiu.ac.jp
Conflicts of Interest
The authors declare no conflicts of interest relevant to this study.
Acknowledgements
This work was supported by JSPS KAKENHI Grant Number JP60773182.