Introduction
Groin injuries account for up to 10–18% of all sports-related musculoskeletal complaints, with the adductor longus being the most commonly affected muscle of the adductor group. Accurate and timely evaluation is essential, given the functional role of the adductor longus in hip adduction, flexion, and stabilization during high-demand movements such as cutting, sprinting, and kicking resulting in acute injury. However, many injuries to the adductor longus are chronic and repetitive in nature. The mechanical enthesopathies generally present with pain of the inner and top of the thigh which radiate downwards toward the knee. Adductor rupture does occur but is rare compared to overuse. Most commonly in the younger athlete rupture of the tendon occurs as an antero-inferior public avulsion fracture.1
Magnetic resonance imaging (MRI) is widely considered the gold standard for complex groin pathology. However, diagnostic musculoskeletal ultrasound (MSK-US) provides a practical, dynamic, and cost-efficient alternative that allows direct visualization of the tendon and muscle in real time. The portability of ultrasound makes it particularly attractive for both clinical and sideline evaluation.2,3
Sonographic Anatomy of the Adductor Longus
The adductor longus is a large triangular shaped muscle located in the medial thigh compartment. Its origin varies. It can attach anteriorly from tendon fibers (40%) at the pubic body just inferior to the pubic crest, and also to the public symphysis posteriorly via muscular fibers (60%).4,5 It can also originate from just muscle fibers or all tendinous fibers. However, it generally inserts on the middle third of the linea aspera of the femur. It is a relatively small muscle in size measuring approximately 11.6 mm in length with a thickness of 3.7 mm with a cartilaginous enthesis.5,6
Normal Sonographic Appearance
The patient is typically examined in the supine position with a linear transducer. The thigh should be abducted approximately 30 degrees, externally rotated and the knee flexed.7 Assessment of the adductors begins with identifying the central aponeurosis of the adductor longus, then moving more proximally the musculotendinous junction or tendon proper. These images can be taken in either long axis (LAX) parallel to the muscle and tendon fiber orientation or short axis (SAX) perpendicular to the muscle and tendon fiber orientation.
The adductor longus is easily identified as it is the most superficial of the adductors. Asymptomatic cortical irregularities may be seen due to enthesopathy but may also be seen due to incomplete fusion of secondary ossification centers.8 Anisotropy is a common issue as the tendon runs in an oblique direction. The longus tendon is easily seen at its origin at the body of the pubis, just lateral to the pubic symphysis and slightly inferior to the crest. It will appear as a well-defined triangular hypoechoic structure in the SAX view.9,10
Key sonographic landmarks
-
Proximal tendon origin: Hyperechoic fibrillar tendon adjacent to the pubic symphysis.
-
Musculotendinous junction: Transition from tendon to pennate muscle belly, a common site of injury.
-
Dynamic imaging: Resisted hip adduction enhances visualization of subtle defects or tendon gapping.
Diagnostic Utility of MSK-US
Accuracy and Sensitivity
-
Ultrasound demonstrates high sensitivity in detecting partial- and full-thickness adductor longus injuries, with the advantage of dynamic evaluation and contralateral comparison.
-
Compared with MRI, MSK-US provides faster, lower-cost evaluation, though MRI may still be warranted in complex cases or when broader differential diagnoses are considered.
Typical Pathological Findings
-
Acute strains/tears: Hypoechoic or anechoic regions within tendon or musculotendinous junction; associated hematoma.
-
Chronic tendinopathy: Tendon thickening, heterogeneous echotexture, reduced fibrillar pattern, and possible neovascularization on Doppler.
-
Complete rupture: Loss of continuity with tendon retraction, surrounding hematoma, and fluid collection.
Advanced Techniques
-
Power doppler/Color doppler: Useful in identifying neovascularization in tendinopathy.
-
Microvascular imaging (MVI): May improve sensitivity in detecting low-flow neovessels, with potential relevance in chronic cases.
Comparative Role with Other Modalities
-
Clinical examination: Critical first step but limited in grading severity.
-
MRI: Comprehensive cross-sectional imaging; superior for complex or multi-structure involvement.
-
MSK-US: Portable, dynamic, repeatable, cost-effective; optimal for serial monitoring and sideline assessment.
Clinical Implications for Rehabilitation Providers
Although rehabilitation planning is not the primary focus here, the evaluation phase directly informs care decisions. For example:
-
Grading partial vs. complete rupture affects timelines for load progression.
-
Identifying tendinopathy versus acute tear differentiates between rest, progressive loading, or surgical referral.
-
Serial ultrasound imaging allows objective monitoring of healing before return-to-play clearance.
Thus, MSK-US is not simply diagnostic—it is integral to the continuum of clinical reasoning for rehabilitation providers.
Conclusion
Diagnostic MSK-US is a powerful and practical tool for evaluating adductor longus injuries. Its ability to provide immediate, dynamic, and repeatable insights makes it highly valuable in sports medicine and rehabilitation settings. While MRI remains important for complex cases, ultrasound offers unique advantages at the point of care, particularly for rapid diagnosis, injury grading, and monitoring. Rehabilitation providers who develop competency in sonographic evaluation are positioned to enhance diagnostic precision and improve patient outcomes.
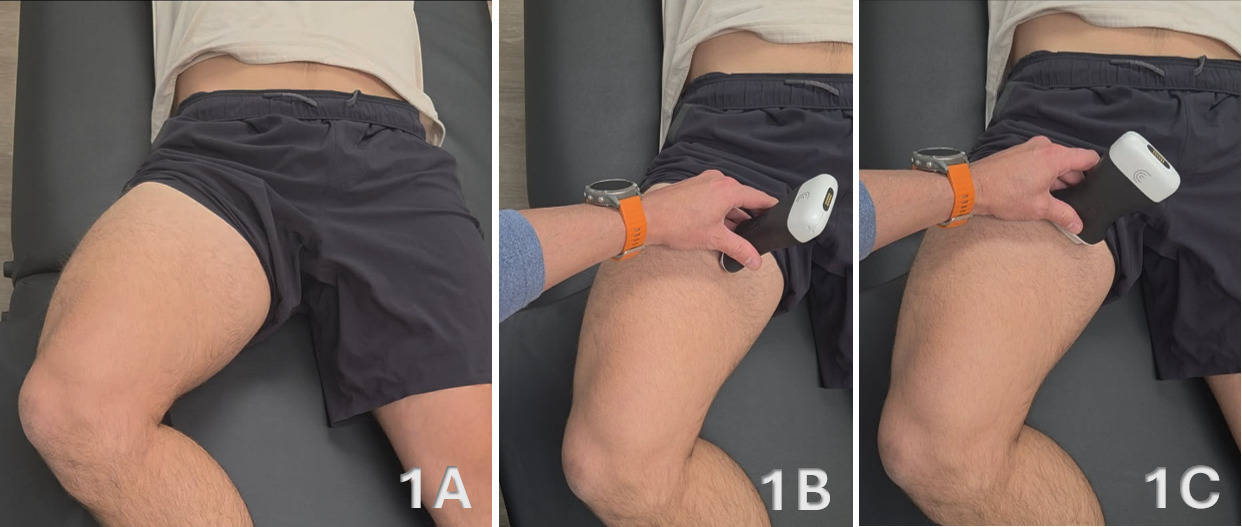
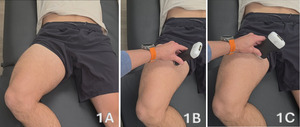
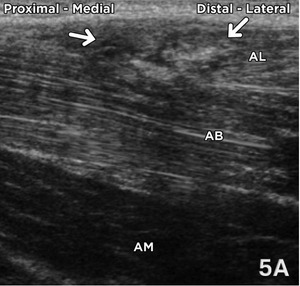
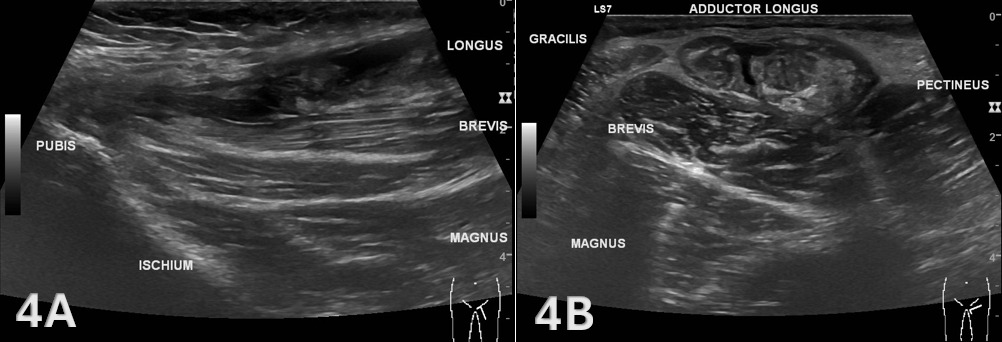
Figure 1A: Patient Positioning
The patient is positioned supine with the hip in neutral and the knee slightly flexed (~20–30°) to relax the adductor compartment. The thigh should be externally rotated slightly to expose the medial aspect. Support the knee with a towel roll as needed. For proximal tendon evaluation, ensure the groin and pubic region are appropriately draped and exposed for access from the pubic symphysis to the mid-thigh. Imaging is performed at rest, with optional dynamic adduction against gentle resistance to assess contractile thickening or focal pain reproduction.
Figure 1B: Transducer Placement for Adductor Longus in LAX
To obtain a LAX view, place a high-frequency linear transducer parallel to the long axis of the adductor longus muscle and tendon, centered along the medial thigh from its origin at the pubic body and pubic crest. The transducer marker should face proximally toward the patient’s head. Optimize depth so that the full tendon-to-muscle transition is visible. In this orientation, the fibrillar tendon extends distally and merges into the hypoechoic muscle belly. Slight heel-toe angulation helps minimize anisotropy. Follow the tendon proximally to its superficial insertion adjacent to the pubic symphysis, noting the relationship to the gracilis (superficial and medial) and the adductor brevis (deep and posterior).
Figure 1C: Transducer Placement for Adductor Longus in SAX
For SAX imaging, rotate the transducer 90° so the marker points toward the patient’s right. Begin at the proximal origin of the adductor longus just inferior to the pubic tubercle, identifying the round to oval echogenic tendon surrounded by hypoechoic muscle tissue. In this plane, the gracilis appears medial and slightly superficial, while the adductor brevis and magnus lie deep and posterior. Sweep proximally toward the pubic insertion and distally through the muscle belly to ensure continuity and assess for localized disruption, edema, or hematoma. Subtle probe tilting should be used to maintain perpendicular insonation and prevent anisotropy of the tendon fibers
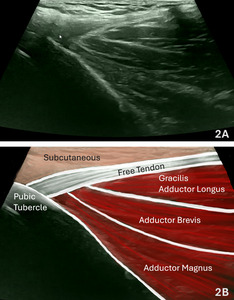
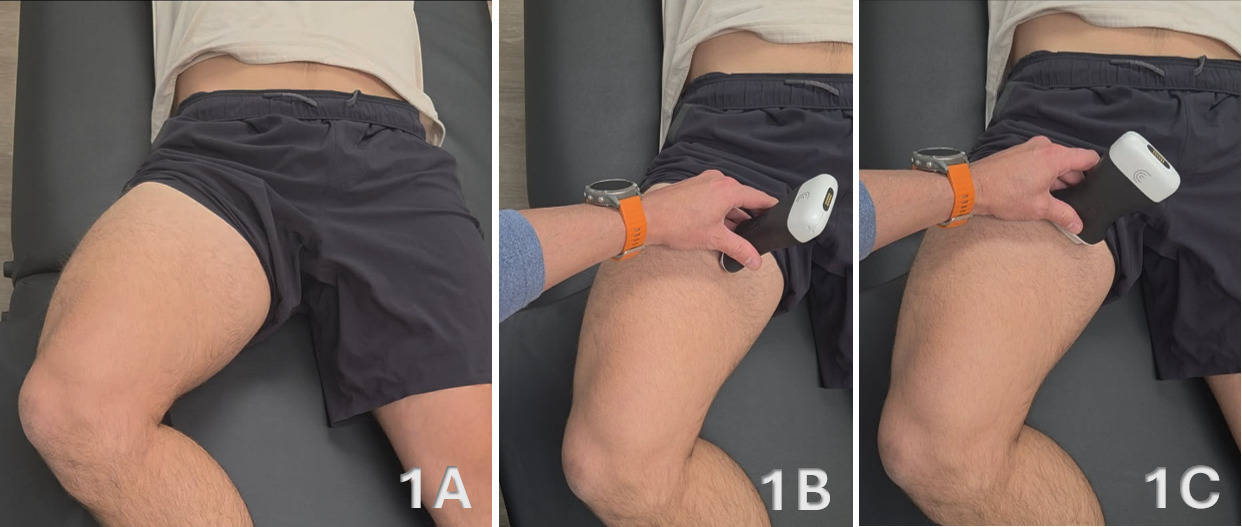
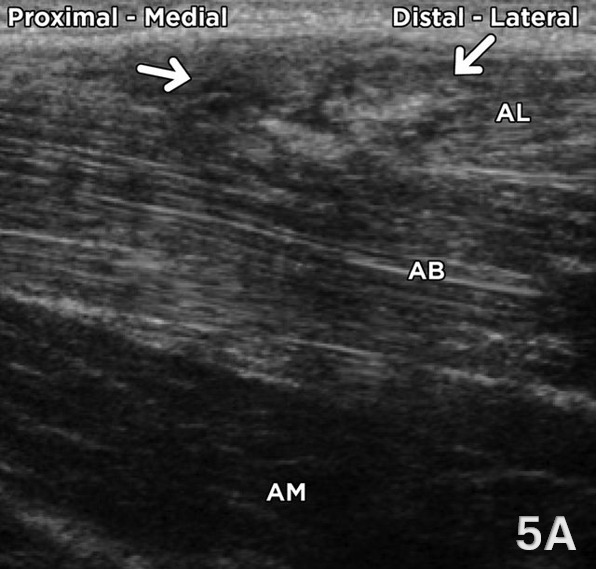
Figures 2A and 2B: Normal Adductor Longus in LAX
Refer to Figure 1B for the transducer position for this image. In LAX, align the transducer parallel to the adductor longus fibers and center the muscle belly longitudinally. The adductor longus appears as a hypoechoic, pennate muscle with a uniformly fibrillar tendon proximally that transitions smoothly into the muscular portion distally. The tendon demonstrates parallel hyperechoic lines converging toward its bony attachment on the pubis, just lateral to the symphysis. Deep to the adductor longus, portions of the adductor brevis and adductor magnus can be visualized, while the gracilis lies more superficial and medial. Optimize imaging so the proximal tendon and its insertion are clearly visualized, positioning the posterior border of the muscle in the lower third of the image with the focal zone at or just deep to this level. Use slight heel-toe adjustments to minimize anisotropy and maintain a consistent insonation angle. Document tendon continuity, echotexture, and thickness at rest, and, when appropriate, during gentle resisted adduction to assess for contractile integrity and pain reproduction.
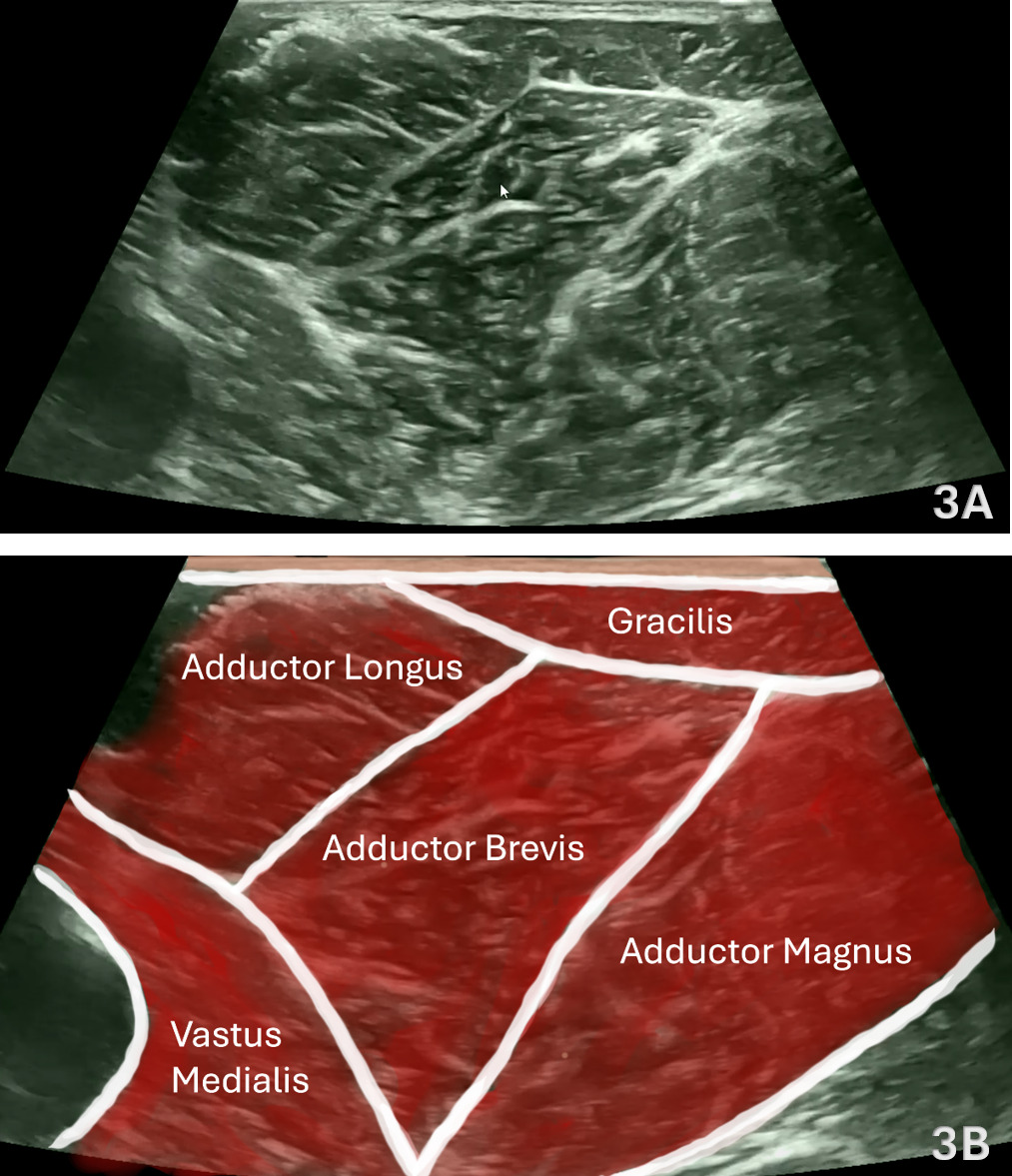
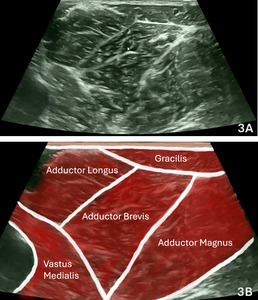
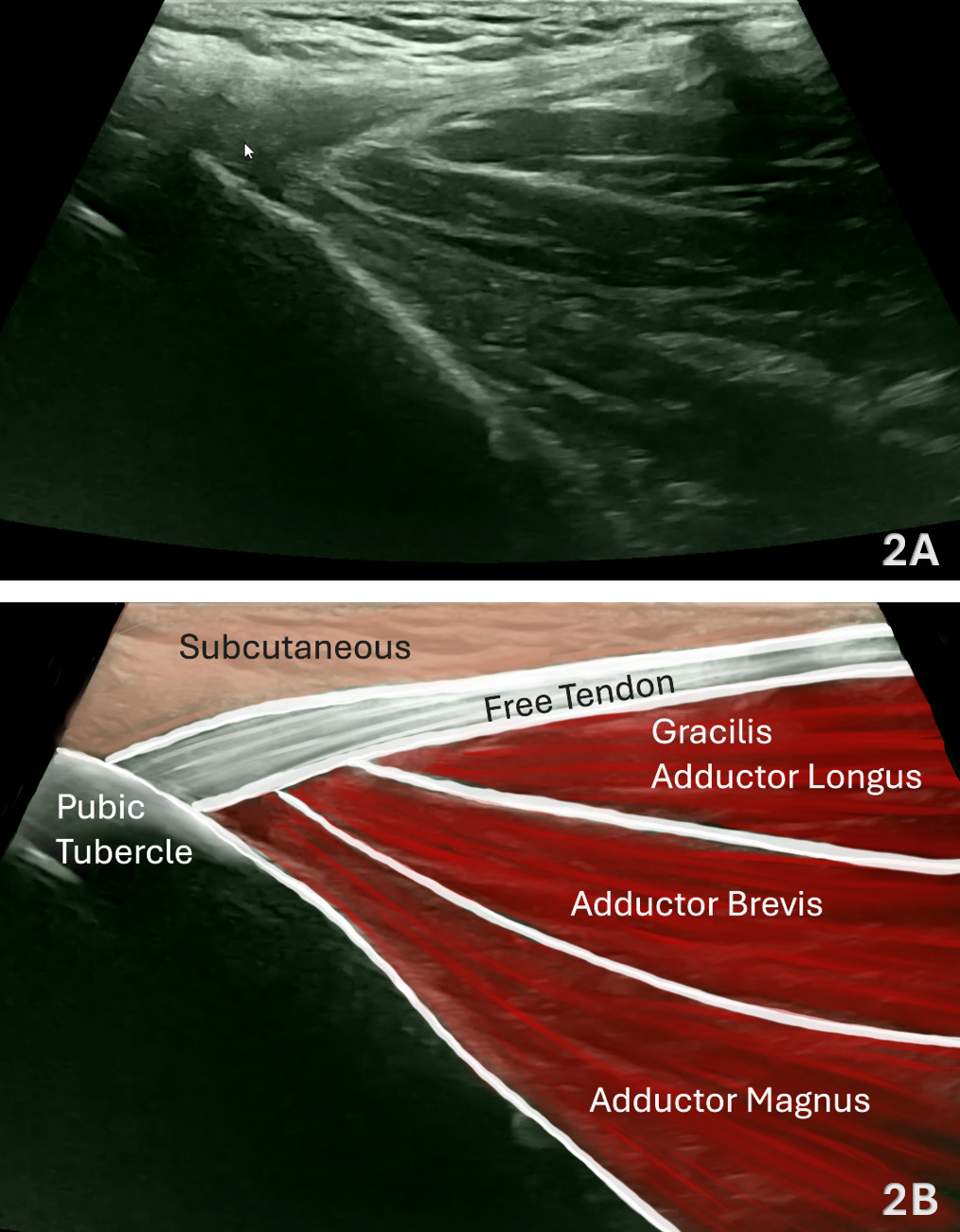
Figures 3A and 3B: Normal Adductor Longus in SAX
Refer to Figure 1C for the transducer position for this image. In SAX, position the transducer transversely just posterior to the adductor longus tendon and center over the muscle belly. The gracilis serves as a consistent superficial and medial landmark, with the adductor longus positioned deep to it, and the adductor brevis and adductor magnus lying deeper and more posterior—forming the characteristic layered appearance of the medial thigh (gracilis → longus → brevis → magnus). The intramuscular tendon of the adductor longus may be seen centrally as an oval echogenic structure surrounded by hypoechoic muscle tissue. Use light transducer pressure to avoid compression artifacts and maintain consistent depth and contrast. Sweep proximal ↔ distal along the muscle to evaluate continuity from the pubic attachment through the myotendinous junction and into the distal belly. Apply gentle probe toggling to minimize anisotropy, particularly near the tendon, ensuring that echogenicity accurately represents fiber alignment. Document tendon thickness, echotexture, and continuity bilaterally for comparison, noting any focal hypoechogenicity, loss of definition, or asymmetry that may indicate tendinopathy or partial tearing.
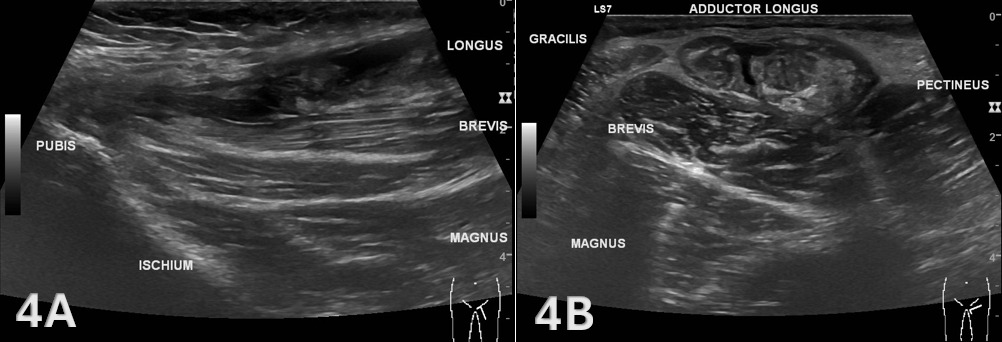
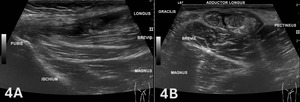
Figure 4. Adductor Longus Tear (LAX and SAX)
Figures 4A and 4B demonstrate a complete non-bony avulsion of the adductor longus tendon from its pubic attachment, with approximately 32 mm of tendon retraction and an intervening fluid-filled defect consistent with acute hematoma or edema. The retracted tendon end appears thickened and oedematous, indicative of acute injury. The adductor brevis, adductor magnus, gracilis, and pectineus muscles demonstrate normal echotexture and continuity, confirming that the injury is isolated to the adductor longus.11
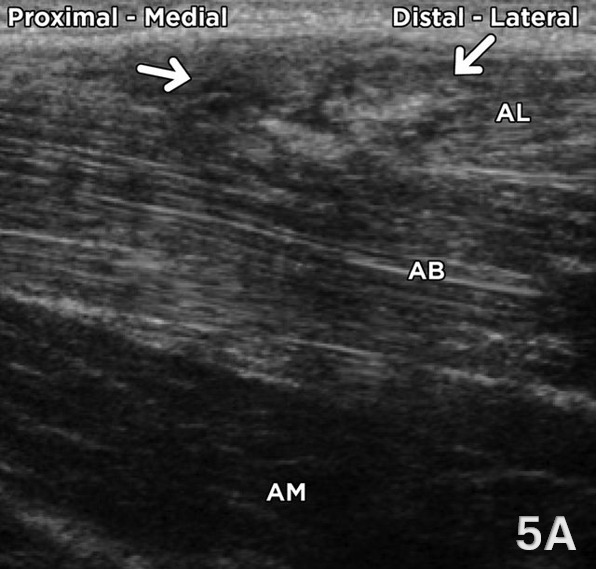
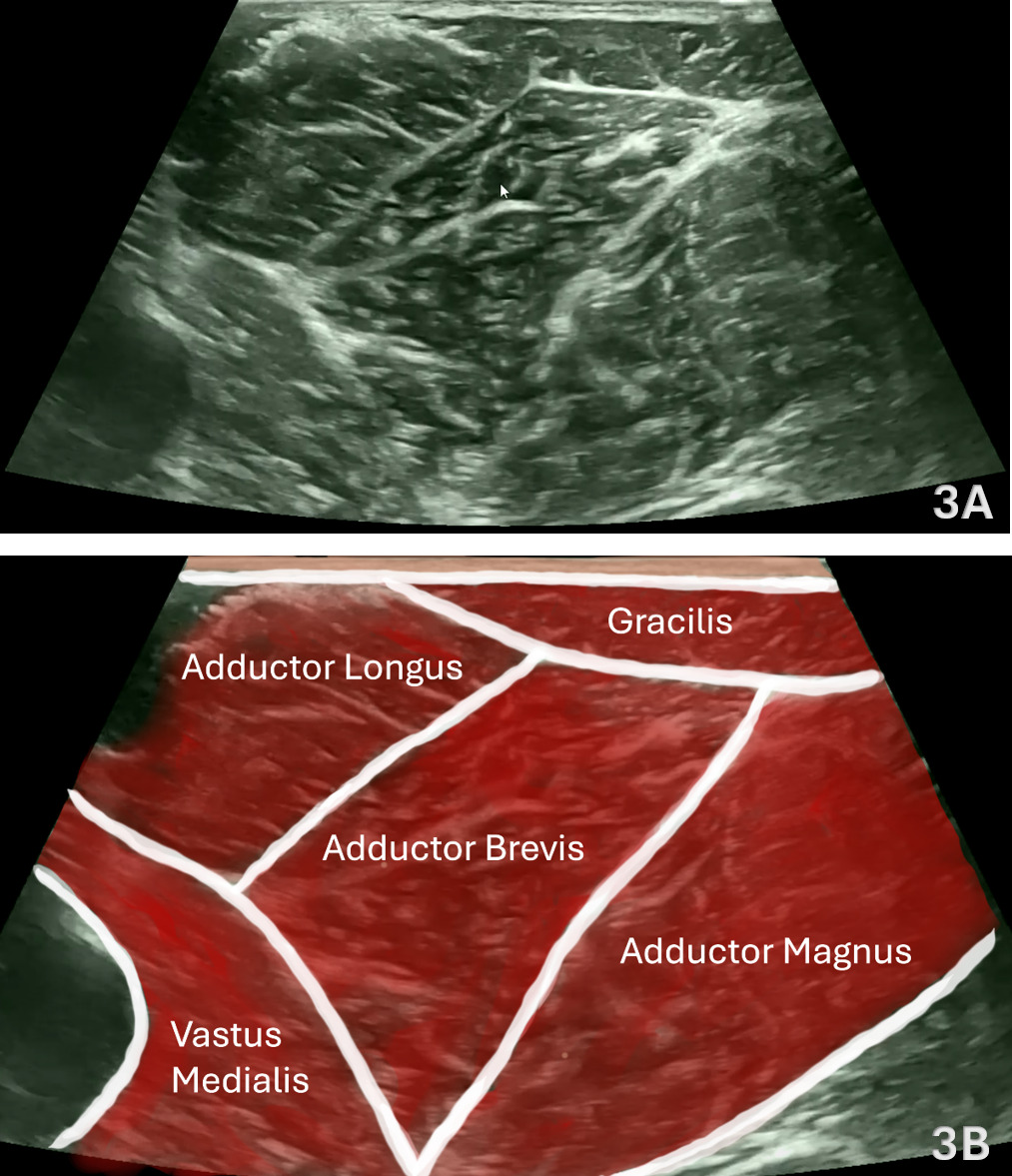
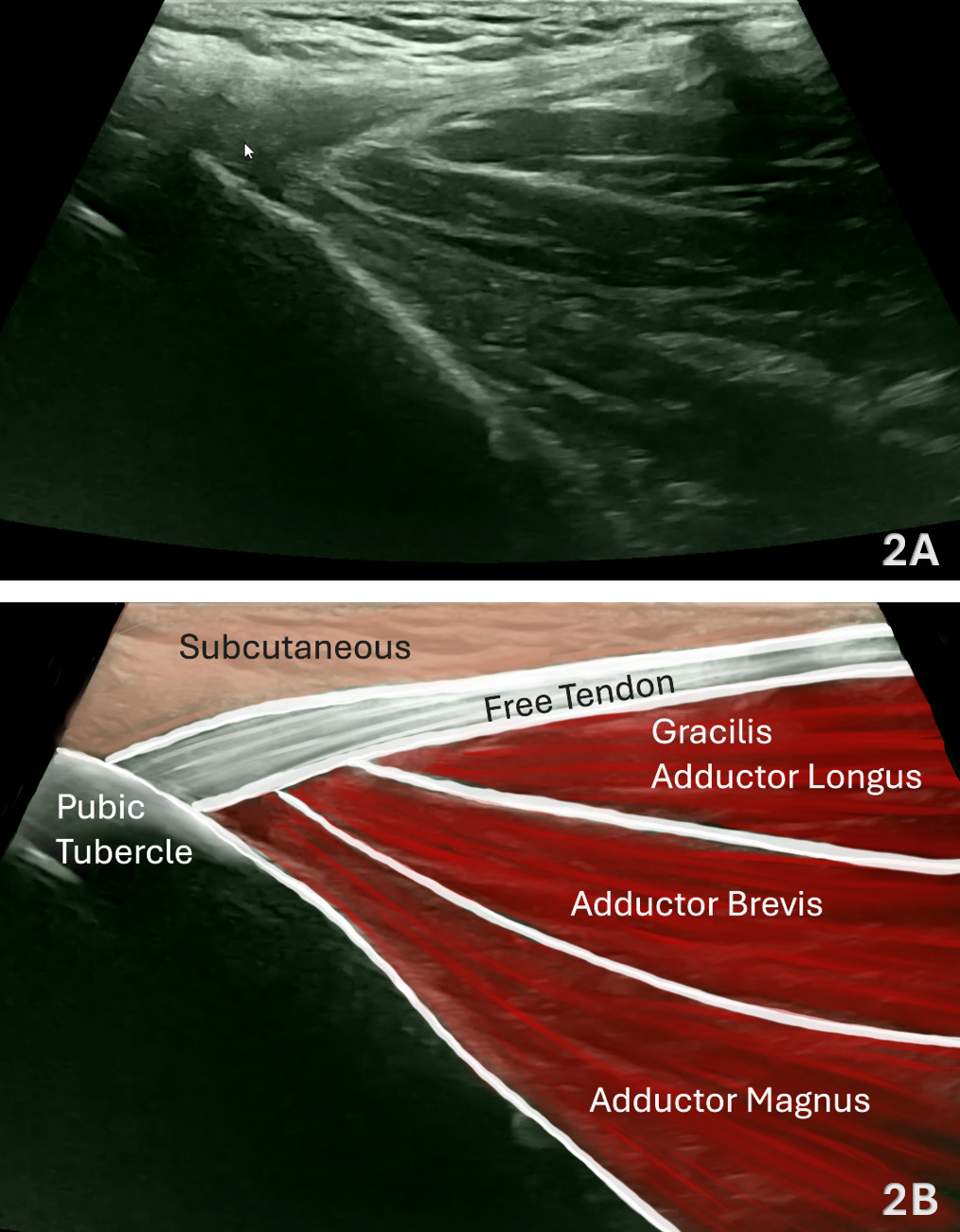
Figure 5. Partial Adductor Longus Muscle Tear in LAX
Figure 5A shows a partial adductor longus muscle tear in a 22-year-old male tennis player presenting with an acute tearing sensation in the right inguinal region. A longitudinal oblique ultrasound image of the proximal adductor compartment demonstrates focal heterogeneity, architectural distortion, and fiber discontinuity within the adductor longus (AL), consistent with a partial muscle tear. The adductor brevis (AB) and adductor magnus (AM) appear intact and maintain normal echotexture and architecture.12

Figure 6. Adductor Longus Tendinosis in LAX
Figure 6A shows a chronic adductor longus tendinopathy in a 36-year-old male runner with a history of bilateral groin pain. LAX ultrasound imaging of the contralateral left adductor longus demonstrates a thickened, hypoechoic tendon origin consistent with tendinosis, accompanied by a small focal detachment at the pubic attachment (arrow). The adjacent adductor brevis, adductor magnus, gracilis, and pectineus muscles appear normal in echotexture and architecture, confirming that the pathology is isolated to the adductor longus.13