Introduction
Baseball is one of the most widely played and highly competitive sports in the world, particularly in Japan. As of 2022, over one million players, including approximately 130,000 high school players, were registered with Japanese baseball organizations.1,2 Upper extremity injuries are common among baseball players and are primarily attributed to chronic overuse.3–6 In particular, more than 54.3% of Japanese baseball players aged 6–17 years have experienced elbow pain.7 Throwing-related injuries predominantly affect the shoulder and elbow joints,8,9 and in severe cases, these injuries necessitate surgical intervention and prolonged rehabilitation,10 significantly impacting an athlete’s career. Despite advancements in research on throwing-related injuries, the incidence of upper extremity injuries among high school baseball players continues to increase.5
In the context of upper extremity injury prevention, the early identification of at-risk athletes is crucial to mitigate the progression of dysfunction and facilitate timely interventions.11 Playing despite pain or discomfort under high physical load is a well-established risk factor for injury progression and the eventual need for surgical intervention.12,13 Traditional assessments of upper extremity function in baseball players primarily rely on range of motion (ROM) tests, strength tests, and orthopedic evaluations, focusing primarily on structural or mechanical features.14 However, they often fail to detect early-stage symptoms, such as discomfort, fatigue, or decreased performance, which are subjective in nature and difficult to capture through objective measures alone.
Recently, patient-reported outcomes (PROs) have been recommended as effective tools for evaluating upper extremity function and injuries.15 They provide valuable insight into athletes’ self-reported symptoms, offering a complementary perspective on throwing-related injury severity.15 The Kerlan–Jobe Orthopaedic Clinic Shoulder and Elbow Score (KJOC) was developed as a PRO to specifically assess upper extremity function in overhead athletes and is widely used in English-speaking countries.11,16 Although it is primarily used for postoperative evaluations and return-to-play assessments after elbow surgery,16–18 its application in field-active athletes who continue to play despite experiencing mild symptoms remains limited. Conventional objective measures may not adequately reflect the lived experience of athletes playing with pain, underscoring the need to evaluate whether the Japanese version of the KJOC (J-KJOC) can reliably detect early upper-extremity symptoms in this population. Establishing a sensitive and practical screening tool would enable medical staff and coaches to intervene before the symptoms progress to more severe injury.
Therefore, this study aimed to determine the clinical utility of the J-KJOC for identifying symptomatic high school baseball players and to establish a cutoff score for the early detection of upper extremity dysfunction. It was hypothesized that the J-KJOC would be more sensitive than conventional physical assessments for detecting symptomatic and at-risk players.
METHODS
Study Design
This cross-sectional study was conducted between March 2023 and April 2024 on high-school baseball players from a single team in Japan. This study adhered to the ethical principles of the Declaration of Helsinki and was approved by the Research Ethics Committee of the Kitasato University School of Allied Health Sciences (Approval Number: 2022-032). Before participation, all players received a detailed explanation of the study’s objectives, methods, potential risks and benefits, and data protection measures, verbally and in writing. Written informed consent was obtained from all participants. Although all participants were minors (≥16 years old), the institutional review board approved that they possessed sufficient cognitive capacity to independently provide consent. In addition, parents or legal guardians were notified of the study and were provided with the opportunity to have their child opt out, in accordance with the approved ethical protocol. Data were collected using self-reported questionnaires and physical assessments. All data were anonymized to ensure confidentiality.
Participants
This study included 89 high-school baseball players from a single team in Japan. The eligibility criteria required participants to be active members of the team and to participate in practice at least six times per week. Participants were excluded if they did not provide informed consent, were unable to undergo physical assessments due to pain or other reasons or had undergone upper limb surgery within the previous six months.
The participants were classified into three groups based on their self-reported evaluations using the J-KJOC.
-
Asymptomatic player group (AP group): players who reported no upper extremity discomfort or pain during play.
-
Symptomatic player group (SP group): players who reported upper extremity discomfort or pain but were able to continue playing.
-
Inactive symptomatic player group (ISP group): players who reported upper extremity discomfort or pain that prevented them from playing. Although these players were temporarily unable to participate at the time of evaluation due to pain, they routinely participated in baseball practice ≥6 days per week under normal circumstances, consistent with the study’s inclusion criteria.
All responses were classified according to predefined criteria to ensure consistency and reliability of group allocation.
Procedures
The assessment session lasted approximately 30 min and included the completion of the J-KJOC, followed by physical assessments. Player characteristics (age, baseball experience, playing position, body mass index, and throwing-arm dominance) were collected at the same time as the J-KJOC. Physical assessments included measurements of shoulder range of motion (ROM), isometric shoulder strength, grip strength, and pinch strength. Physical assessments were conducted in a randomized order to minimize potential biases related to the measurement sequence. All assessments were performed by physiotherapists with one to three years of clinical experience. Before data collection, all examiners completed a standardized training session that included confirmation and practice of key measurement procedures such as ROM assessment and handheld dynamometry to ensure consistency and reliability.
Outcome measures
J-KJOC
The KJOC has been reported as a highly sensitive tool for detecting subtle changes in upper extremity function in baseball players.17 The J-KJOC consists of two sections: a demographic information section and a 10-item visual analog scale (VAS) section evaluating upper extremity health and function, and it was administered using a paper-based questionnaire. It has demonstrated good reliability and validity in assessing upper extremity performance among Japanese collegiate baseball players.19
The demographic section collected data on throwing arm dominance, playing position, highest level of baseball participation, and current playing status, including the presence or absence of pain/discomfort and ability to continue playing.
In the VAS section, athletes were instructed to mark an “x” on a 10-cm (100-mm) line corresponding to each of the 10 items. The position of the “x” was measured in millimeters from the left endpoint and recorded as the score for each item. The overall score was calculated as the mean of the 10 item scores, with a maximum possible score of 100 and higher scores indicating better perceived upper extremity function and performance. The VAS assessed key aspects of upper extremity function including pain severity, muscle weakness, fatigue, instability, and difficulty in initiating movement. Additionally, the questionnaire evaluated the impact of upper extremity symptoms on critical performance factors, such as throwing mechanics, velocity, power, endurance, control, and overall competition level.
Isometric Strength of Shoulder Internal and External Rotators
The isometric strength of shoulder internal and external rotators was assessed with the participants positioned in a prone posture, with the shoulder abducted to 90° and the elbow flexed to 90°. Two examiners conducted the measurements: one examiner manually stabilized the scapula by placing a hand over the lateral border, whereas the other used a digital handheld dynamometer (Mobile ZMT−201; Sakai Medical Co., Ltd., Tokyo, Japan) to measure isometric strength. The dynamometer was positioned 5 cm proximal to the wrist joint. Internal rotation was performed with the dynamometer positioned on the volar aspect of the forearm, whereas external rotation was performed with it positioned on the dorsal aspect. A make test was performed, in which a verbal cue was given, and the participant exerted a maximal isometric contraction that was held for 5 seconds.20,21 Strength values were recorded in kilograms-force (kgf). Each measurement was performed twice for both the throwing and non-throwing sides, and the mean value was used for the analysis.
Shoulder Internal and External Rotation Range of Motion
Shoulder ROM was assessed with the participants positioned in a supine posture, with the shoulder abducted to 90° and the elbow flexed to 90°. The examiner manually stabilized the scapula by placing a hand over the coracoid process to prevent compensatory movements. Passive internal and external rotations were performed to the end range,22 and angles were recorded using a digital inclinometer (Huepar AG01; Huepar, Shenzhen, China) aligned with the longitudinal axis of the forearm, using the olecranon process as the axis and the ulnar styloid process as the reference point. Each measurement was performed once for both the throwing and non-throwing sides, and the value was used for the analysis.
Grip Strength
Grip strength was assessed with participants in a standing posture, maintaining their arms at their sides with the elbows fully extended in a neutral position.23 They were instructed to exert maximum grip strength for three seconds while maintaining this posture. A digital dynamometer (Grip-D, Smedley type, Takei Scientific Instruments, Niigata, Japan) was used for measurements, and values were recorded in kilograms-force (kgf). Each hand was tested twice on both the throwing and non-throwing sides, and the mean value was used for the analysis.
Pinch Strength
Pinch strength was assessed in the standing posture, with the arm at the side and the elbow fully extended. The pads of the index and middle fingers and the pad of the thumb were placed flat on the pinch sensor, with the forearm fully pronated and the wrist maintained in a neutral position.24 A digital handheld dynamometer with a pinch attachment (Mobile ZMT-201; Sakai Medical Co., Ltd., Tokyo, Japan) was used to measure pinch strength, and values were recorded in kilograms-force (kgf). The participants were instructed to exert maximum effort for three seconds while maintaining the specified posture. Each hand was tested once on both the throwing and non-throwing sides, and the value was used for the analysis.
Statistical analysis
The required sample size was calculated a priori using G*Power (version 3.1.9.6; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany [http://www.gpower.hhu.de/]) to ensure adequate statistical power. An effect size of 0.7, reflecting a medium-to-high effect, was selected based on previous studies that reported significant differences in outcomes between players with and without throwing-related pain.11,16,17,25 With a desired statistical power of 0.80 and a significance level of 0.05, a total sample size of 56 participants was deemed sufficient for between-group comparisons. For the logistic regression analysis, the rule of a minimum of 10 events per variable (EPV) was applied to reduce the risk of overfitting and ensure model stability.26
Normality of all variables was assessed using the Shapiro–Wilk test. Because several variables violated the normality assumption, nonparametric tests were applied uniformly across all group comparisons to ensure analytical consistency. Comparisons between the asymptomatic player group (AP group) and symptomatic player group (SP group) were conducted using the Mann–Whitney U test. The Kruskal–Wallis test was used for comparisons across the three groups (AP, SP, and ISP groups). When a statistically significant difference was observed, post hoc comparisons were performed using the Steel–Dwass method for nonparametric multiple comparisons.
Receiver operating characteristic (ROC) curve analysis was used to determine the optimal cut-off value of the J-KJOC score for distinguishing between asymptomatic and symptomatic players. The optimal threshold was determined using the Youden J statistic, calculated as sensitivity + specificity − 1. The area under the curve (AUC), sensitivity, specificity, positive likelihood ratio (LR+), and negative likelihood ratio (LR–) were also calculated.
Multivariate logistic regression analyses were performed to identify factors associated with the presence of symptoms during play. The dependent variable was the presence or absence of upper-extremity symptoms during play. The independent variables included the total J-KJOC score and physical assessment measures including shoulder internal and external rotation ROM, isometric internal and external rotation strength, grip strength, and pinch strength. Three separate models were constructed by grouping physical assessments variables into domains (shoulder internal/external rotation ROM, isometric strength, grip strength, and pinch strength). Variables were entered stepwise, and the model with the highest Nagelkerke pseudo-R² was selected as the best-fitting model, because traditional R² values are not appropriate for logistic regression. Multicollinearity was assessed using variance inflation factors (VIFs). All VIF values were below 5, indicating no multicollinearity according to established criteria.27 Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for all predictors.
All statistical analyses were performed using JMP version 17 (SAS Institute, Cary, NC, USA). Statistical significance was set at p < 0.05.
RESULTS
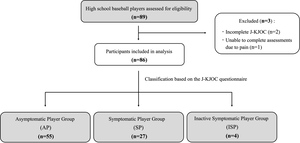
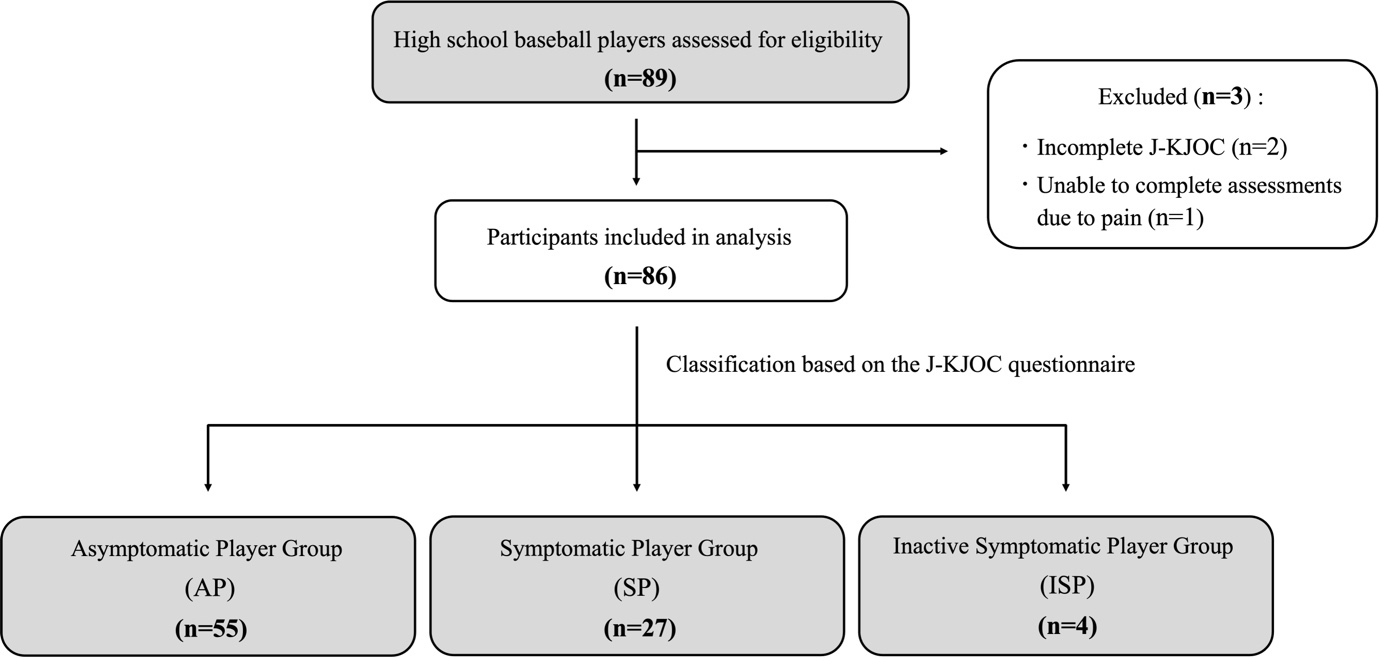
Of the 89 players initially enrolled, three were excluded (two due to incomplete J-KJOC responses and one due to an inability to complete physical assessments), resulting in a final sample of 86 participants (Figure 1). All participants were male, with a mean age of 16.3 ± 0.8 years. Based on self-reported symptoms using the J-KJOC, 55 players were classified as asymptomatic (AP group), 27 as symptomatic but active (SP group), and four as inactive symptomatic (ISP group). The group-wise characteristics, including age, body mass index (BMI), years of baseball experience, and positions played, are shown in Table 1. Age, BMI, and baseball experience did not differ among the three groups (all p > 0.05).
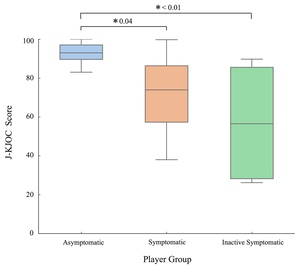
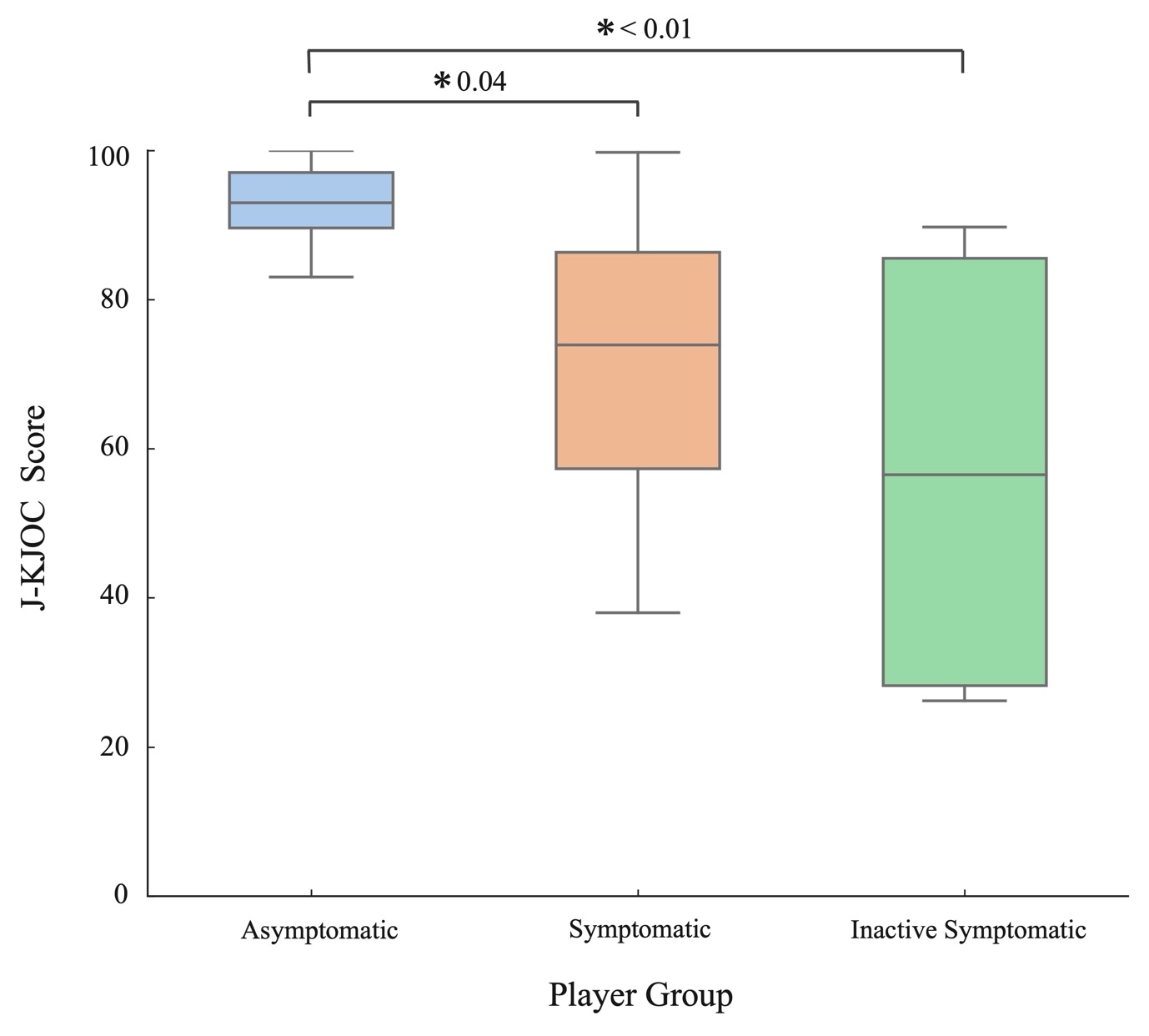
The mean J-KJOC scores were 90.3 ± 9.0 for the AP group; 71.2 ± 18.3, SP; and, 57.2 ± 34.3, ISP. Significant differences in the J-KJOC scores were observed among the three groups (p < 0.01). Post-hoc analysis revealed significant differences between the AP and SP groups (p = 0.04) and between the AP and ISP groups (p < 0.01). However, the SP and ISP groups had no significant differences between them (p > 0.05; Figure 2). In contrast, no significant differences were found among the groups in any of the objective physical assessment measures including shoulder internal and external rotation ROM, isometric shoulder rotation strength, grip strength, or pinch strength (Table 2). The AP and SP groups showed no significant differences in these physical parameters.
The ROC curve analysis identified an optimal cutoff value of 87.6 points for the J-KJOC score to distinguish SP from AP. The AUC of 0.815 indicated good discriminative performance, consistent with established interpretation criteria (AUC 0.8–0.9 = good; >0.9 = excellent).28 The cutoff yielded a sensitivity of 81.5% and a specificity of 72.8%. The positive likelihood ratio (LR+) was 3.00, and the negative likelihood ratio (LR–) was 0.25 (Figure 3).
Multivariate logistic regression analyses were conducted using three separate models to identify factors associated with the presence of symptoms during play (Table 3). In all three models, the J-KJOC score was a significant predictor of symptomatic status. In the ROM model (Model 2), both the J-KJOC score (OR = 0.89, 95% CI: 0.84–0.93, p < 0.01) and shoulder internal rotation ROM (OR = 0.95, 95% CI: 0.91–0.99, p = 0.02) were significantly associated with the presence of symptoms during play. In contrast, no physical assessments variables were significant in either the strength or grip/pinch models. The ROM model showed the highest coefficient of determination (R² = 0.33), suggesting superior explanatory power compared with that of the other models.
DISCUSSION
This study evaluated the clinical utility of the J-KJOC in identifying symptomatic or at-risk high school baseball players. The key findings were as follows: (1) J-KJOC scores significantly differed among the AP, SP, and ISP groups; (2) an optimal cutoff score of 87.6 effectively distinguished symptomatic players with good sensitivity and specificity; and, (3) the J-KJOC score consistently demonstrated stronger associations with pain during play than conventional physical assessment measures in all regression models. These findings suggest that the J-KJOC serves as a complementary tool to traditional objective assessments, particularly for detecting early or subclinical symptoms, rather than implying superior predictive ability.
Notably, none of the conventional physical assessments parameters, including shoulder internal/external rotation ROM, isometric strength, grip strength, and pinch strength, showed significant differences between asymptomatic and symptomatic players, suggesting that objective assessments alone may lack the sensitivity required to detect early-stage dysfunction, particularly in athletes who continue to participate despite having mild symptoms. Moreover, based on previous research, we explored both the absolute values of the throwing arm and the side-to-side differences. Although glenohumeral internal rotation deficit (GIRD) and shoulder strength asymmetry have been identified as risk factors for upper extremity injuries in overhead athletes,20,29–31 the current results did not reveal any significant group differences in either absolute or bilateral values. This further highlights the limitations of conventional physical assessments testing in identifying early dysfunction in field-active players. However, although IR ROM did not reach a statistically significant difference (p = 0.06), the consistent decline across groups may reflect a clinically meaningful pattern commonly reported in overhead athletes, and may have achieved significance with a larger sample size.
The optimal cutoff score of 87.6 established in this study aligns with previous reports. Kraeutler et al. reported a mean KJOC score of 94.8 (95% CI: 92.9–96.7) in healthy professional pitchers, with scores <90 potentially indicating early functional decline.32 Similarly, Wilkins et al. reported a median score of 90.5 (IQR: 76.6–97.2) among collegiate players, suggesting that high KJOC scores are generally expected in healthy overhead athletes.33 These findings reinforce the potential of the J-KJOC cutoff score of 87.6 as a practical reference value for screening for high school players. Although the likelihood ratios represented only small shifts in post-test probability, such small changes may still be clinically meaningful when identifying early-stage or subclinical dysfunction. The cutoff value identified in this study (87.6/100) is higher than the value reported by Monti et al.,25 who proposed a score of 68.6/100 based on a much broader age range (10–18 years). Because younger athletes may have limited experience with self-reported outcome measures and differ substantially in physical maturity, symptom awareness, and baseball-specific training exposure, directly comparing their cutoff scores to those of high school athletes may not be appropriate. By focusing solely on high school players with a relatively homogeneous educational level and training background, the present study may provide a more interpretable and contextually relevant cutoff value for this specific population.
Multivariate logistic regression analyses showed that the J-KJOC score was the only consistently significant predictor of symptomatic status across all models. Among the physical assessments variables, only internal rotation ROM on the throwing side was significantly associated with pain during play, reinforcing the well-established role of the GIRD as an injury risk factor. Collectively, these findings demonstrate that the J-KJOC is a highly sensitive and practical tool for identifying athletes with early-stage or subclinical upper extremity dysfunction. Unlike conventional tests, the J-KJOC captures subjective complaints, including pain, fatigue, instability, and performance decline, which may not yet be apparent in physical parameters, thereby enabling early detection of “hidden dysfunction.” This early identification is critical for timely intervention and may help prevent injury progression, thereby supporting long-term athletic performance. As such, PROs like the J-KJOC should be integrated into routine screening protocols, particularly for adolescent athletes, where symptom underreporting is common. By providing a noninvasive and athlete-centered screening method, the J-KJOC offers significant clinical value for injury prevention in high-risk athletic populations.
Limitations
This study had several limitations. First, although the total sample size was sufficient for group comparisons, the low number of symptomatic players (n = 27) may have limited the statistical power of the multivariate regression analyses. To reduce the risk of overfitting, the authors constructed three separate models based on measurement domains, rather than a single model with multiple variables. This strategy aligns with the widely accepted guideline of requiring at least 10 EPV for logistic regression,26 thereby ensuring more robust and interpretable results. Second, because all participants were recruited from a single high school baseball team in Japan, the generalizability of the findings may be limited. Future studies involving multisite recruitment and broader sampling are necessary to validate the applicability of the J-KJOC cutoff score across different populations. Third, the ISP group (n = 4) was small and represented only a few severe cases. Therefore, the findings related to this group should be interpreted with caution and regarded as preliminary.
Conclusions
The J-KJOC demonstrated strong clinical utility in identifying upper extremity symptoms in high school baseball players. Compared with conventional physical assessments, the J-KJOC score more effectively identified players who continued to play despite discomfort or pain. A cutoff score of 87.6 accurately distinguished symptomatic from asymptomatic players, underscoring its potential as a practical screening tool for the early detection and prevention of upper extremity injuries in adolescent athletes.
Conflicts of Interest
The authors declare that they have no conflicts of interest related to this study.