Introduction
Meniscus injuries can be highly problematic to the health and function of the knee. A tear in one of the menisci will increase joint mechanical stress by limiting the knee’s normal shock-absorbing capacity, which may contribute to joint degeneration over time.1,2
Anatomy of the Meniscus
The menisci are two crescent-shaped structures situated between the femur and the tibia. The slightly concave surface of the proximal tibia turns into a deeper concavity to accept the large convex distal femoral condyles. This is especially important on the lateral side of the knee joint, as the lateral tibial plateau is flatter and at times slightly convex. These intervening structures help dampen high compressive forces across the knee. Secondarily, menisci are involved with joint lubrication and nutrient distribution.3–6
The Role of MSK Ultrasound in Meniscus Evaluation
Advantages
-
Non-Invasive: Point-of-care ultrasound is a non-invasive imaging technique that can be used on a variety of soft tissue knee pathologies, including the meniscus.7–11
-
Real-Time Imaging: MSKUS allows evaluation of the medial or lateral meniscus during both weightbearing and non-weightbearing. Ultrasound can be used at the same time the knee is loaded12–15 while it is moved through the available range of motion.16 Displacement of meniscal tissue can be seen dynamically.17,18
-
High-Resolution Visualization: MSKUS provides detailed images of the outer rim of the medial and lateral meniscus along the respective tibiofemoral joint lines.
-
Accuracy: Sensitivity and specificity for the diagnosis of meniscal tears via ultrasound are reported as high as 88% and 85% respectively.19,20 Specifically, medial meniscus tears have been shown to have sensitivity and specificity ranging from 83% to 97.2% and from 83% to 100%, respectively.
- Accessibility and Cost-Effectiveness: MSKUS is portable, widely available, and less expensive than magnetic resonance imaging (MRI).
Limitations
- Operator Dependency: MSKUS requires skill and experience for accurate interpretation of findings. The ability to sonograph menisci is to a large extent influenced by the operator and the availability and technical considerations of state-of-the-art equipment.
- Depth Limitations: Visualization is usually not a problem for the peripheral meniscus rim; however, deeper structures are not well seen. Deeper tears may not be visualized and, at times, may be more clinically significant and symptomatic.
- Artifacts and Shadows: Bone and calcifications may create image artifacts, requiring adjustments in probe positioning and frequency.
Sonographic Technique for Evaluating the Menisci
Equipment Setup
- Probe Type: Because of the superficial nature of the peripheral meniscal rim, a standard high-frequency, linear array transducer is normally used.
-
Patient Position Lateral Meniscus: The patient is lying on their side with the examined extremity on top and the knee barely flexed. To examine the lateral meniscus better, a small bolster may be placed between the knees to create a small varus stress to the knee that opens with the posterolateral joint line, allowing better visualization. The transducer should be placed longitudinally at the crease of the popliteal fossa.
-
Patient Positioning Medial Meniscus: The patient is placed in supine with a bolster under the knee to provide a slight amount of flexion. With the bolster in place under the knee and some slight external rotation at the hip and knee, the medial aspect of the joint is easily exposed. The transducer is placed across the posteromedial knee.
-
Dynamic Assessment: A varus or valgus stress, or movements of knee flexion and extension can be applied during evaluation.
Examination Protocol
Normal Sonographic Appearance
Typically, the menisci are viewed in the long axis (LAX). The meniscus is easily seen because it is triangular in shape and bounded superiorly by the femur and inferiorly by the tibia. The bones are easily seen by their hyperechoic texture. The meniscus itself is a well-defined, homogeneous, triangular-shaped mass of tissue.
Pathologic Findings in Injured Meniscal Tissue
-
Hypoechoic bands or stripes in meniscal tissue may indicate a tear.8,11,20–24 The hypoechoic band will vary depending on the size, shape, and location of the tear.
-
Anechoic pockets of associated joint effusion.
-
Extruded meniscus tissue. Meniscal extrusion may be seen when the meniscus is displaced off the tibial plateau, resulting in extrusion.25
-
Parameniscal cysts are a fluid-filled cystic mass in continuity with meniscal tears. These are more common on the medial side of the knee. These cysts arise from degenerative meniscus tears and may also present as external soft tissue swelling along the medial or lateral knee joint line. These are usually seen as thin-walled anechoic cysts abutting the meniscus body and, at times, have fluid cleft extensions running from the cyst to the actual meniscus tear.
Clinical Implications for Rehabilitation Providers
MSKUS provides real-time feedback for rehabilitation professionals, facilitating early diagnosis of meniscal injury and intervention. Key applications include:
-
Early Detection of Injury / Accurate Injury Grading: MSKUS can quickly differentiate between a torn meniscus, effusion, or extruded meniscus to help guide treatment planning.
-
Dynamic Functional Testing: Rehabilitation professionals can use MSKUS during loaded weight-bearing activities or in non-weight-bearing activities through a range of motion to assess the effect of functional dynamic movements on the meniscus.
-
Guided Interventions: Ultrasound imaging assists in precision-guided injections, such as corticosteroids for inflammation.
-
Patient Education: Real-time imaging serves as a visual aid to explain the nature of the injury and set realistic expectations for recovery.
Limitations and Challenges
Due to MSKUS’s limited visibility of deeper meniscus structures, magnetic resonance imaging (MRI) may still be the imaging modality of choice; however, MSKUS can evaluate the meniscus very quickly and at a lower cost, and pathologic findings can be seen in many instances.
Conclusion
MSKUS is a valuable, dynamic, and cost-effective imaging modality for evaluating medial and lateral meniscus injuries of the knee. Its ability to provide high-resolution, real-time visualization of peripheral meniscus pathology, continuity, and surrounding soft-tissue structures makes it an excellent first-line tool in both acute and chronic settings. Ultrasound allows visualization of the meniscus in standing and non-weight-bearing positions using a gentle range of motion. While MRI remains the reference standard for meniscus tears due to MSKUS’s limited visibility of the entire meniscus, MSKUS offers distinct advantages in accessibility, rapid assessment, lower cost, and guidance for therapeutic interventions such as injections or rehabilitation monitoring. Incorporating MSKUS into physical therapists’ clinical practice enhances diagnostic accuracy, supports timely management decisions, and ultimately improves patient outcomes in suspected meniscus injury cases.
Lateral and Medial Meniscus
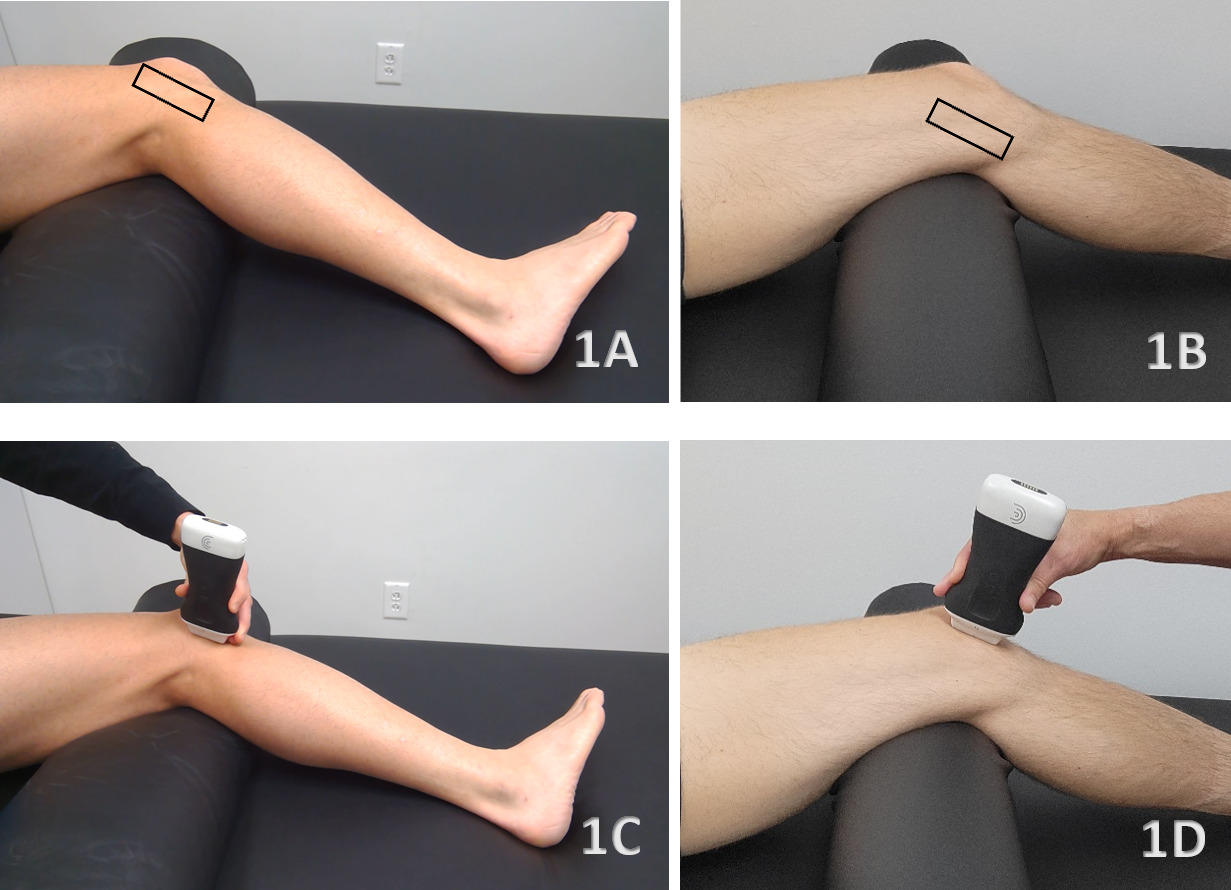
Figures 1A and 1B Patient Position with Transducer Outlined
The patient is positioned supine with a small bolster under the knee to maintain approximately 20–30° of flexion. This position relaxes the quadriceps and opens the joint space, creating an optimal acoustic window for visualizing both the medial and lateral meniscus.
Figure 1A: For lateral meniscus imaging, the lower leg is internally rotated to expose the lateral joint line.
Figure 1B: For medial meniscus imaging, the foot and leg are externally rotated to expose the medial joint line.
Dynamic assessment can be enhanced by gently applying valgus stress to better visualize the medial meniscus or varus stress to open the lateral joint line.
Figures 1C and 1D Long Axis Transducer Placement
Figure 1C: For the lateral meniscus, palpate the fibular head and position the transducer just superior to it in a long-axis (LAX) orientation. Sweep the probe anteriorly until the lateral meniscus becomes visible deep to the lateral collateral ligament and adjacent to the popliteus tendon. Because the lateral meniscus sits deeper and has more curvature, subtle heel-to-toe rocking is essential for minimizing anisotropy and clarifying the cartilage–bone interfaces.
Figure 1D: For the medial meniscus, begin on the posterior aspect of the medial knee and place the transducer in a LAX orientation along the medial joint line. Gently skim anteriorly until the triangular fibrocartilaginous wedge of the medial meniscus appears beneath the medial collateral ligament (MCL). Minor tilting adjustments are often necessary to optimize visualization because the MCL lies superficial to the meniscal body.
Normal View in LAX
A complete sonographic assessment of the medial and lateral meniscus involves systematically sweeping the transducer from anterior to posterior to visualize the anterior horn, body, and posterior horn. Throughout the examination, gentle rocking of the transducer is necessary to minimize anisotropy, which can otherwise produce misleading hypoechoic regions that mimic pathology. Careful attention should be given to the relationship between the meniscus and surrounding ligamentous structures, particularly the MCL overlying the medial meniscus and the LCL–popliteus interface on the lateral side. Identification of adjacent soft-tissue landmarks, including the pes anserine complex and semimembranosus tendon medially, as well as the biceps femoris and iliotibial band laterally, further aids in orientation and diagnostic accuracy. Compared with the medial compartment, vascular structures are less prominent on the lateral side, reducing the likelihood of mistaking vascular pulsation for meniscal pathology.
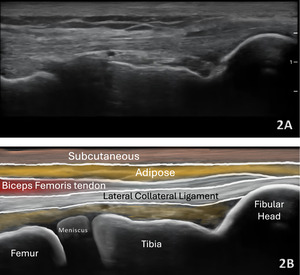
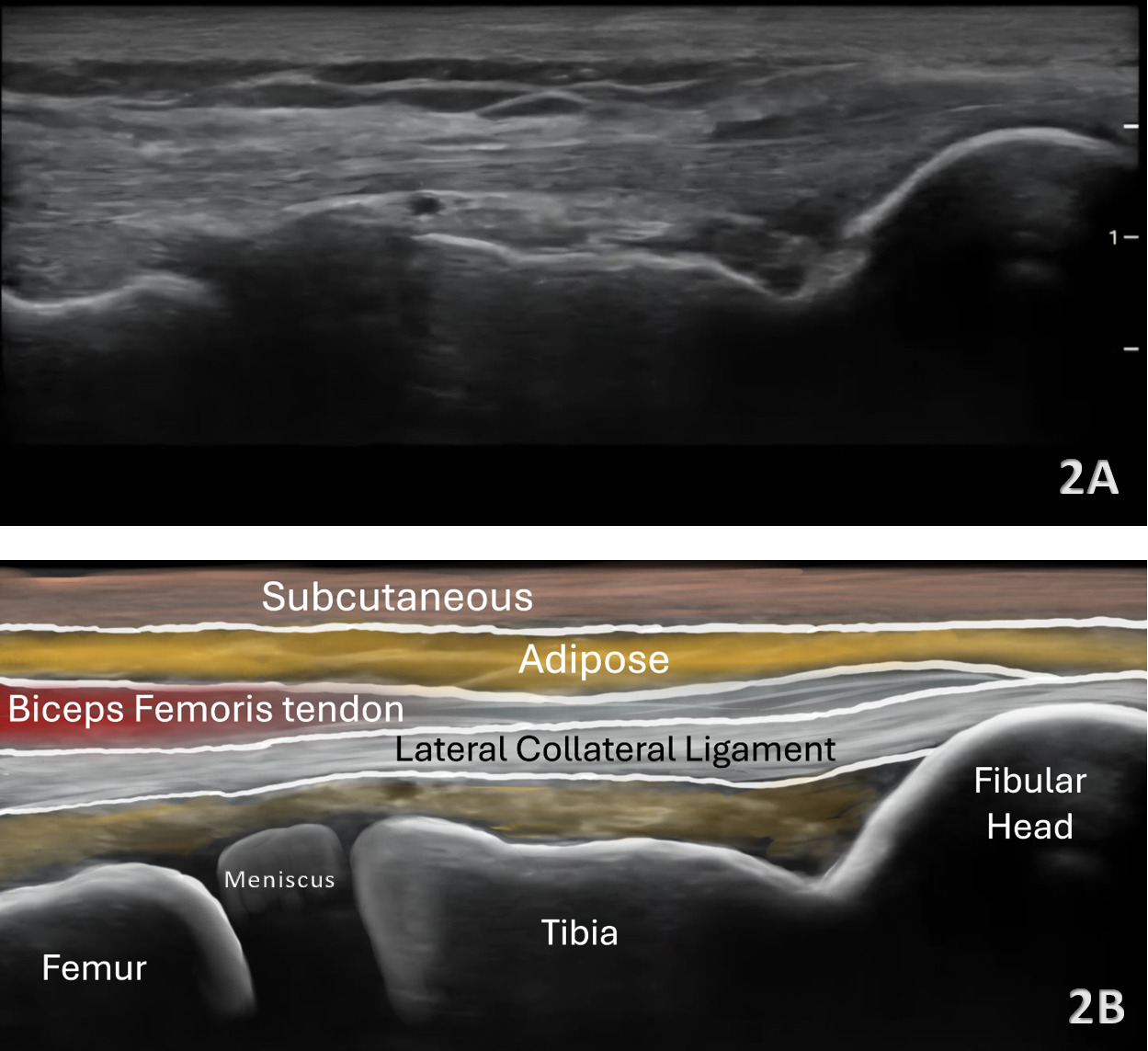
Lateral Meniscus
Figures 2A and 2B LAX View of Lateral Meniscus: The lateral meniscus demonstrates a triangular configuration but often appears slightly deeper and more curved than the medial meniscus. It lies beneath both the LCL and popliteus tendon, requiring careful angulation to eliminate anisotropy. Its increased mobility relative to the medial meniscus can be appreciated during subtle varus stress.
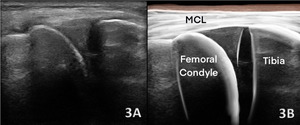
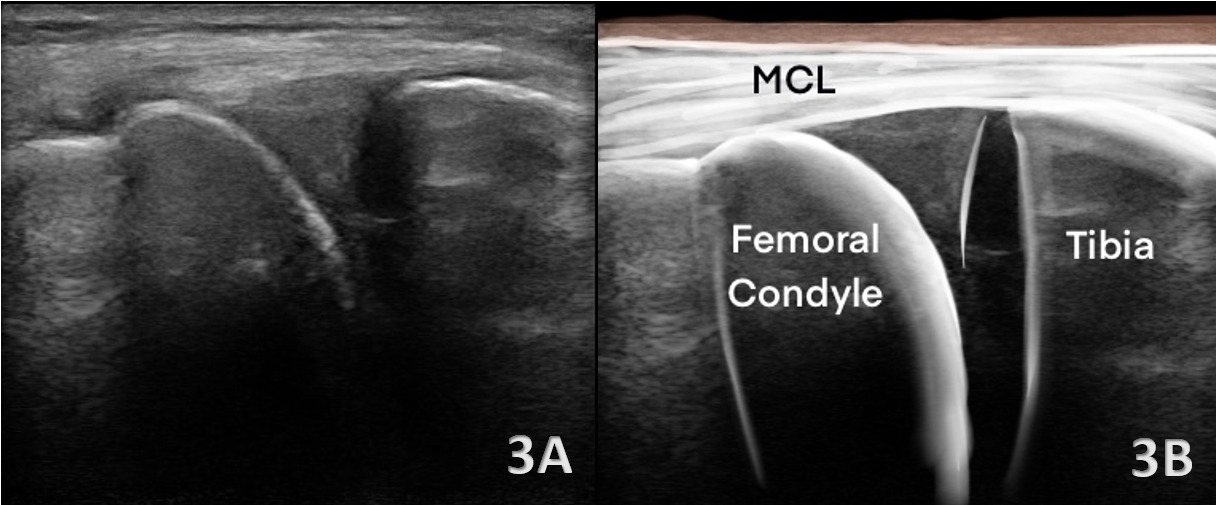
Medial Meniscus
Figures 3A and 3B LAX View of Medial Meniscus: The medial meniscus appears as a homogeneous, moderately hyperechoic, triangular structure positioned between the medial femoral condyle and the tibial plateau. The superior and inferior margins are smooth and well-defined. Sweeping the transducer from anterior to posterior allows visualization of the anterior horn, body, and posterior horn.
Pathology
Meniscal Tear General Findings
Meniscal tears on diagnostic ultrasound are characterized by disruption of the normal homogeneous, wedge-shaped architecture of the meniscus, most commonly visualized as focal hypoechoic or anechoic clefts within the fibrocartilage. Depending on transducer orientation and scanning plane, vertical, horizontal, flap, or radial tear patterns may be identified. Diagnostic confidence is increased when additional features are present, including irregular or truncated meniscal surfaces, extrusion of the meniscus beyond the tibial margin, hypoechoic clefts extending to the articular surface, and associated joint line fluid or synovial thickening.
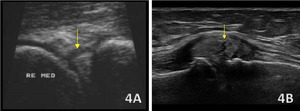
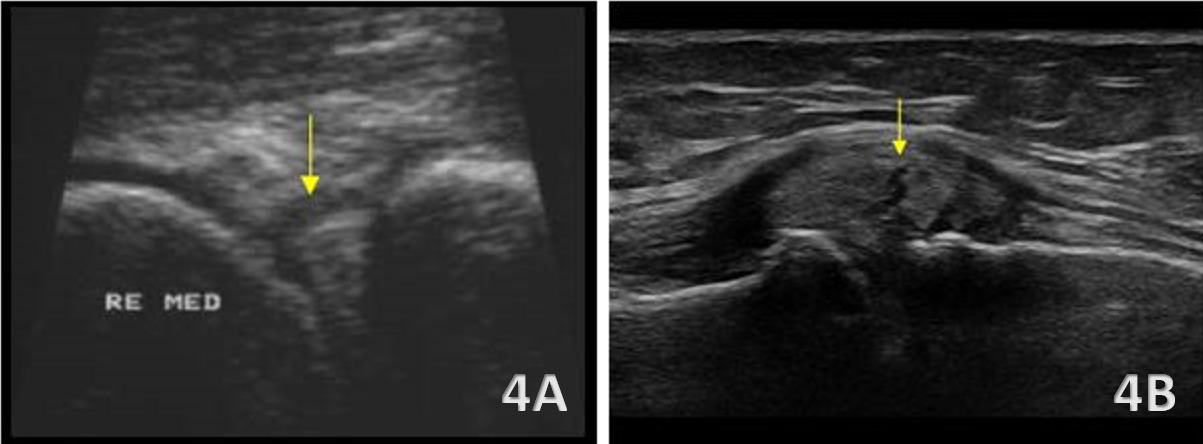
Medial Meniscus Tear and Cyst Formation
Figures 4A and 4B: Tears of the medial meniscus are often more readily visualized due to its superficial location and firm attachment to the joint capsule and MCL. Sonographic findings include loss of the normal triangular contour, focal hypoechoic or anechoic clefts within the meniscal body as seen above in Figure 4A, and extrusion beyond the medial tibial margin as seen above in Figure 4B. Associated findings such as joint line fluid, capsular thickening, or adjacent MCL involvement are common and may further support the diagnosis, particularly in degenerative or chronic presentations.
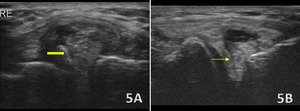
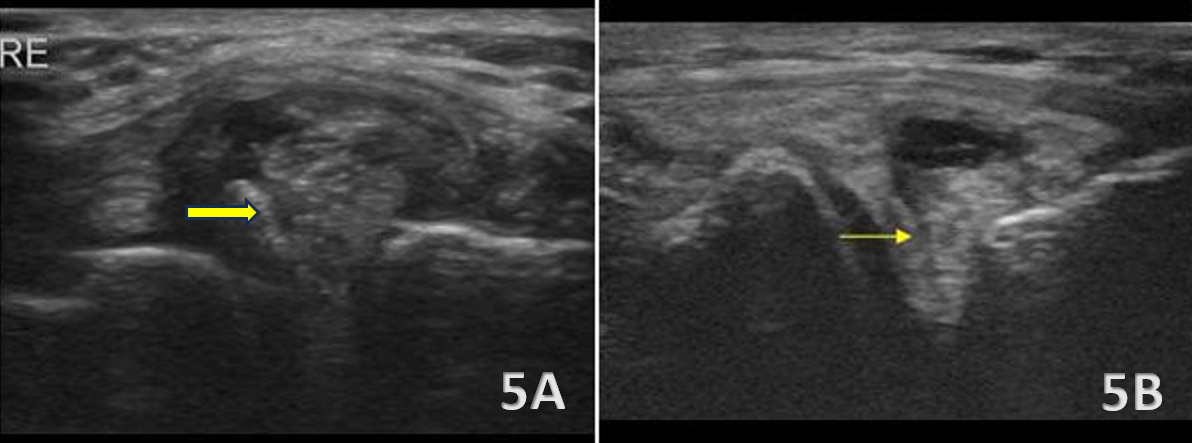
Lateral Meniscus Tear and Cyst Formation
Figures 5A and 5B: Tears of the lateral meniscus can be more subtle on ultrasound due to its deeper location and the presence of overlying structures such as the LCL and popliteus tendon. Pathology is suggested by hypoechoic defects, irregular margins, or distortion of the normally well-defined triangular meniscal wedge. Additional findings may include abnormal contact between the meniscus and popliteus tendon, small displaced fragments or loose bodies adjacent to the joint line, and parameniscal cyst formation, which is commonly associated with lateral meniscal tears. Joint line fluid may further accentuate the tear plane. The application of gentle varus or valgus stress during imaging can improve visualization by accentuating meniscal extrusion or revealing instability within torn segments.