Introduction
Rotator cuff lesion (RCL) is a common disorder of the shoulder that can exist from unknown etiology or be associated with mechanisms such as trauma or progressive degeneration of the tendon.1,2 In general, traumatic RCLs are associated with higher energy injury mechanisms and result in complete or extensive ruptures, while atraumatic RCLs originate from pre-existing partial ruptures, which can eventually progress to total lesions.3,4 Traumatic RCLs are primarily treated surgically and good functional results can be achieved if surgery is performed within a period of up to six months after the initial trauma has occurred.5,6
The Danish National Clinical Guideline on Shoulder Injuries7 recommends, following surgical repair of RCLs, immediate immobilization and rehabilitation. The negative impacts of immobilization during the injury period may be minimized by a comprehensive rehabilitation program (restoration of mobility, scapular stability, shoulder strength, and muscle endurance), increasing the probability of success after surgery and ensuring a return to functional activities with a better quality of life.8 Scapular rehabilitation has important clinical relevance in the alignment and function of the glenohumeral (GHJ) and acromioclavicular joints.9 Imbalance in the scapular stabilizing muscles, such as high upper trapezius muscle activity, low activation of the middle trapezius and lower trapezius, and serratus anterior insufficiency, may be associated to abnormal scapular movement and pain in the shoulder.10,11 As such, scapular rehabilitation is a critical component of the post-surgical comprehensive rotator cuff rehabilitation regimen.
Pre-operative physiotherapy was reported in 1980 by Noyes12 in individuals with chronic anterior cruciate ligament (ACL) deficiency, to promote the restoration of function prior to surgery, maximize dynamic muscle stabilization prior to reconstruction, and facilitate post-operative recovery. Pre-operative lower extremity rehabilitation is widely used in clinical practice, and studies have shown its effectiveness in muscle stabilization prior to reconstruction, improved stability, and in some cases possibly avoiding surgery.13–15 In a preoperative rehabilitation program for ACL rupture, data showed that the pre-operative group presented a significant post-operative improvement in quadriceps strength, static balance, agility, and subjective performance, compared to the control group.13
Pre-operative scapular rehabilitation before shoulder surgery has also been described. Düzgün et al.16 opined that pre-operative scapular rehabilitation program aims to reduce pain, restore the normality of scapular movements, and strengthen the periscapular muscles, providing painless movement in the shoulder. However, publications on scapular rehabilitation prior to surgical treatment of traumatic rotator cuff injuries are scarce. The aim of this study was to evaluate the impact of preoperative scapular rehabilitation before arthroscopic repair of traumatic rotator cuff injury, regarding pain, range of motion of the shoulder, and functional activity. The hypothesis is that the individuals who participated in the pre-operative scapular exercises would develop better range of motion with less pain than those in the control group.
Methods
This was a pilot randomized clinical trial (RCT) experimental study, of 22 adult individuals, with a history of shoulder pain after trauma, and diagnosed with RCL by an orthopedic shoulder surgeon, through clinical examination (full passive range of motion of the shoulder, positive tests for rotator cuff tear: Jobe or full can test; Infraspinatus test: External Rotation Lag Sign, Patte, Drop arm; Subscapularis test: Gerber, Belly Press or Bear Hug) and confirmed by magnetic resonance imaging (MRI). All had a medical indication for surgical treatment with arthroscopic repair of their lesions, and a pre-operative scapular rehabilitation program would be evaluated as an intervention. Those who had previous fractures or pre-existing shoulder conditions such as adhesive capsulitis, joint instability, or labral lesions were excluded.
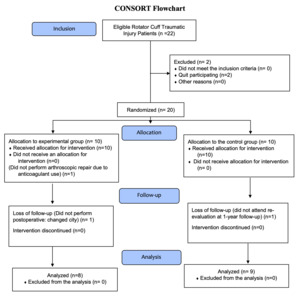
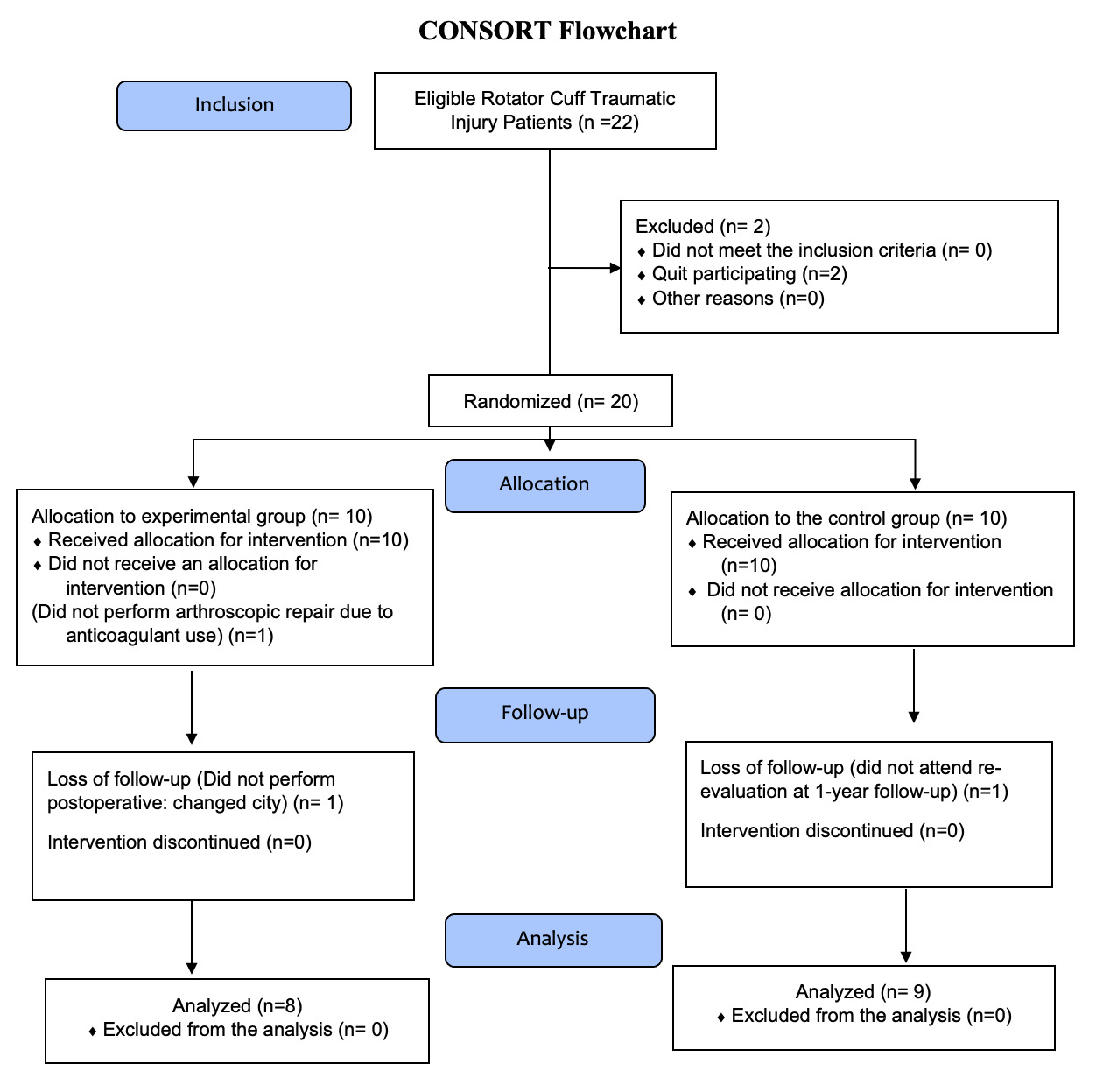
The individuals who agreed to participate in the study provided informed consent prior to the start. The study was approved by the Ethics and Research Committee of the institution (Opinion No. 421.569). After inclusion in the study, all underwent a physiotherapist assessment consisting of history and physical examination, including goniometry to assess joint range of motion (ROM), and the visual analog scale (VAS) for assessing pain. Two patients did not attend the assessment and were excluded, with an initial group totaling 20 individuals. Because this was a pilot study, the individuals were recruited by convenience from a group of patients who were already waiting for the surgical procedure, without previous calculating of the sample size. Randomization was accomplished through the RANDOM.ORG program, and the participants were allocated into two groups: experimental (EG) and control (CG), with a numerical code assigned according to arrival order (Figure 1).
Participants in the EG received an exercise booklet and were instructed by physiotherapists to perform, in the home environment, exercises for scapular and core stabilization, mobility of the cervical spine, elbow, wrist, and hand, as well as exercises to improve shoulder proprioception, and on pain control (Appendix 1). CG members also received a home exercise booklet, but only with exercises involving mobility of the cervical spine, elbow, wrist, and hand, and analgesics guidelines. Each study participant received verbal guidance and training on the execution of each exercise to be performed. Individuals were challenged to perform all exercises in the booklet, three times a day (once in the morning, once in the afternoon and once at night), 10 repetitions of each exercise, or according to availability and pain tolerance. In case of pain during or after the exercises, they were instructed to perform analgesic procedures with local cryotherapy for 20 minutes. The groups followed the preoperative routine for six weeks, with reassessments by the same physiotherapist every two weeks, in which they were asked about the execution of exercises and perception of pain, either in person (among those who could present to the rehabilitation center) or via telephone. After six weeks, with the surgeons blinded as to the individuals’ participation in the rehabilitation program, the patients underwent arthroscopic repair of the rotator cuff lesions using standard procedures, performed by one of the three orthopedic surgeons co-authors (Table 1).
The post-operative rehabilitation protocol (Appendix 2) was the same for both groups and began one week after surgery. All individuals were reassessed in the third month and in the one-year post-operative follow-up, using the VAS, ROM, the Disabilities of the Arm, Shoulder and Hand Questionnaire (DASH), the Western Ontario Rotator Cuff Index (WORC), and 12-item health survey (SF-12). This study was conducted in accordance with the CONSORT guidelines for clinical trials.
Statistical analysis
A descriptive and exploratory analysis of the data was conducted. The analysis of the comparisons between the groups regarding the characteristics of the patients was performed using Fisher’s exact test for the qualitative variables and the Student’s t-test for the quantitative variables. To determine the normality of the data, the Shapiro-Wilk test was used. Taking into account the assumptions of a parametric analysis, a methodology of mixed models for measurements repeated over time, ANOVA and Tukey-Kramer test, was applied. Data unsuitable for a parametric analysis were analyzed using the Mann Whitney (comparison between groups) and Wilcoxon (comparison between timeframes) tests. VAS and goniometry measurements (flexion, abduction, internal and external rotation) were analyzed using mixed models for measurements repeated over time and the Tukey-Kramer test. For the abduction data, since there was a significant difference between the groups in the pre-operative period, the analysis was rerun considering the pre-operative period as a covariate. The WORC data (physical symptoms, sports/recreation, work, lifestyle, emotions, and total score), DASH, and the SF-12 domains (physical and mental) did not meet the assumptions and were analyzed using the Mann Whitney (comparison between groups) and Wilcoxon (comparison between timeframes) tests. The analyses were performed in the SAS17 and R18 programs, with a p-value of 0.05.
Result
From the initial sample of 20 participants with traumatic RCL, in the EG group one patient did not perform surgical repair and one was lost to follow up; one patient in the CG group was lost to follow up, and the final sample for analysis consisted of 17 individuals According to their characteristics, as shown in Table 2 and Table 3, there were no significant differences between the groups regarding gender and age, however there was a significant difference between the two groups for subscapular lesion, as 66.7% of the CG and 12.5% of EG presented with this lesion (p < 0.05).
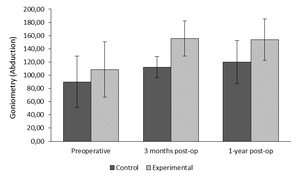
The results of the goniometry measurements are presented in Table 4. In relation to the pre-operative period, flexion and external rotation increased significantly in both groups after three months (p < 0.05). The abduction was significantly higher in the experimental group than in the control group (p < 0.05), after three months and at the one-year follow-up (Figure 2). Regarding internal rotation, there was no significant difference between the groups, nor between the two post-operative reassessment points (p > 0.05).
Regarding the pain assessment (VAS), it was noted that in the CG there was a significant decrease between the three-month and the one-year timeframe (p < 0.05), and in the EG, a significant decrease between the pre-operative period and after one year (p < 0.05). Regarding functional results the WORC total in the EG, after one year, presented scores significantly lower than in the control group (p < 0.05), however, the DASH scores were not significantly different between the groups or between the timeframes (p > 0.05). Analysis of the SF‑12 (Figure 3) showed that after three months, the EG presented significantly higher scores than the CG in the physical component domain of the SF-12 (p < 0.05). (Table 5)
Results from the WORC domains (Figure 4) show that after three months the EG presented values significantly lower than the CG for physical symptoms, work, and emotions (p < 0.05). After one year, the EG presented scores significantly lower than the CG for physical symptoms, sports/recreation, lifestyle, emotions, and WORC total score (p < 0.05).
Discussion
Pre-operative rehabilitation aims to improve the functional capacity of the individual to enable him/her to prepare for the period of inactivity associated with the surgical procedure.17 Described in the literature as having the potential to improve post-operative function, it decreases shoulder stiffness, which is considered a common complication of rotator cuff repair, leading to pain and frustration in patients.19–21 The results showed a significant improvement in pain in the experimental group, between the pre-operative period and one year after, with a significant increase in relation to goniometry of flexion and external rotation in both groups, after three months, and significantly higher values for abduction in the experimental group after three months and one year.
The six-week pre-operative rehabilitation program as described by Seyahi et al.22 provided, after arthroscopic cuff repair, faster recovery of shoulder ROM, scapular muscle and rotator cuff strength, diminished scapular dyskinesis, improved quality of life, and better results in the VAS, DASH, and Constant scores than those who did not utilize the program. In the present study, those receiving education specifically on scapular-focused exercise outperformed on EVA, WORC total, and physical component of the SF-12 in relation to the control group, corroborating the data in the literature. Analyzing the relationship between quality of life (QOL) and WORC, in the evaluated post-operative periods, there were better values of the physical component of SF-12 in the experimental group compared to the control group. However, there was no statistical correlation between WORC and the QOL score, which may be due to the small sample size of this pilot study.
Exercises that focus on the scapula are beneficial to patients with many types of shoulder disorders. Saito et al.23 showed that in adults with subacromial impingement syndrome, scapula-focused exercises could improve pain and shoulder function in the short-term. In the present study, the group that underwent pre-operative rehabilitation with a focus on scapular stabilization presented better results for abduction ROM in the follow-up at three months and one year, and lower WORC values. Baskurt et al.,24 investigating the efficacy of scapula stabilization exercises in patients with subacromial impingement syndrome, found that ROM measurements and quality of life improved statistically in both groups after treatment (p < 0.05), but the group who underwent the six-week scapular stabilization exercise program had a significant improvement in abduction ROM, scapular muscle strength, lower WORC score, and better scapulohumeral rhythm after treatment (p < 0.05).
The purpose of the current study was to analyze the post-operative clinical effects of scapular and core activation before the treatment of a traumatic injury with surgery. These activation with exercises were guided by a physical therapist, who described their execution and frequency. In this sense, the authors believe that the role of this professional in guiding the exercises had a positive impact on the adherence of participants and its clinical results.
The current study was conducted on patients diagnosed with traumatic RCL with surgical treatment indicated, and even with the presence of the lesion, the pre-operative rehabilitation program had patient adherence, and the results of pain control, range of motion of the shoulder, and quality of life were significant. This is similar to the study by Björnsson et al.,25 in which they evaluated the function of 42 shoulders after repair of traumatic lesion of the rotator cuff and showed significantly better scores for the WORC while finding no significant difference for the DASH. In the present study, the EG had lower WORC scores in the three-month period and in the one-year follow-up (p < 0.05), with no significant difference in the DASH between groups.
Düzgün et al.16 described an accelerated rehabilitation protocol consisting of a pre-operative rehabilitation program of four to six weeks and for 24 weeks post-operatively. The accelerated protocol was associated with less pain during activities and at night, after the fifth week, being superior to the slow protocol in terms of functional activity level, as determined by the DASH (p < 0.05). However, they did not determine which variable of the accelerated protocol was responsible for the improvement of the symptoms and the score, unlike the present study where the experiment was pre-operative and both groups followed the same post-operative protocol. The authors believe that pre-operative scapular exercises improve the scapula stability, re-establishing the roles of the scapula9 such as favoring the optimal position of the humerus in the subacromial space and the recovery of shoulder function, which was evidenced by the results of abduction and reduced pain in the patients of the intervention group.
The analysis of the WORC score of the groups showed that the experimental group had better results in the period of one year, which was not observed in the control group, whose value was worse in one year than in three months, with no statistically significant difference. This occurrence may have something to do with the lack of preoperative scapular exercises in the control group.
The post-operative rehabilitation protocol in the present study was the same for both groups, with emphasis on joint mobility gain through passive and active mobilizations, and strengthening of the shoulder girdle, core, and rotator cuff musculature (Appendix II). It is known that post-operative rehabilitation has an important role in functional improvement after rotator cuff repair.26 It is suggested that rehabilitation should include the re-establishment of ROM, shoulder function, and muscle strength, taking into account the healing time of the repaired tendon.27 However, considering the post-operative rotator cuff protocol was effective at aiding the recovery for both groups, the likely factor that positively influenced the experimental group’s results compared to the control group’s results was the inclusion of the pre-operative scapular strengthening program. This suggests that addressing the roles of the scapula9 prior to surgery could benefit rotator cuff function following surgery.
This study presented has limitations such as small sample size (because it was a pilot study), the non-blinding of the evaluator in the post-operative period, and the uncertainty about the patients’ adherence regarding performance of the home based exercises. Despite this, there was a uniform sample of patients in which one physiotherapist came into frequent contact during the preoperative period to both groups and performed the postoperative rehabilitation exercises in the same manner in all participants. Regarding the positives, the study shows that the preoperative rehabilitation significantly improved the physical parameters, demonstrated through the ROM and the functional scores in the follow-ups evaluated. In light of these results, a next study is planed with greater control of these variables. Using the results of WORC for the purpose of calculating the sample size, with a power of 80% and a significance of 0,05, there will be need a total of 86 volunteers.
Conclusion
Pre-operative scapular rehabilitation had a positive impact on the ROM and pain outcomes of individuals who underwent arthroscopic repair of traumatic rotator cuff injury, contributing to good clinical recovery of the patients, as demonstrated by the results of ROM, SF-12 physical component after three months of intervention, and WORC after one year of follow-up. The authors recommend performing pre-operative scapular rehabilitation, focusing on periscapular muscular activation, for patients who will undergo surgical repair of a traumatic rotator cuff lesion.
Conflicts of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.