Is it Injury or Management That is on the Rise?
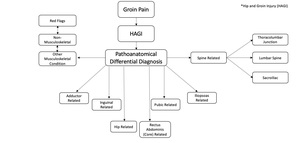
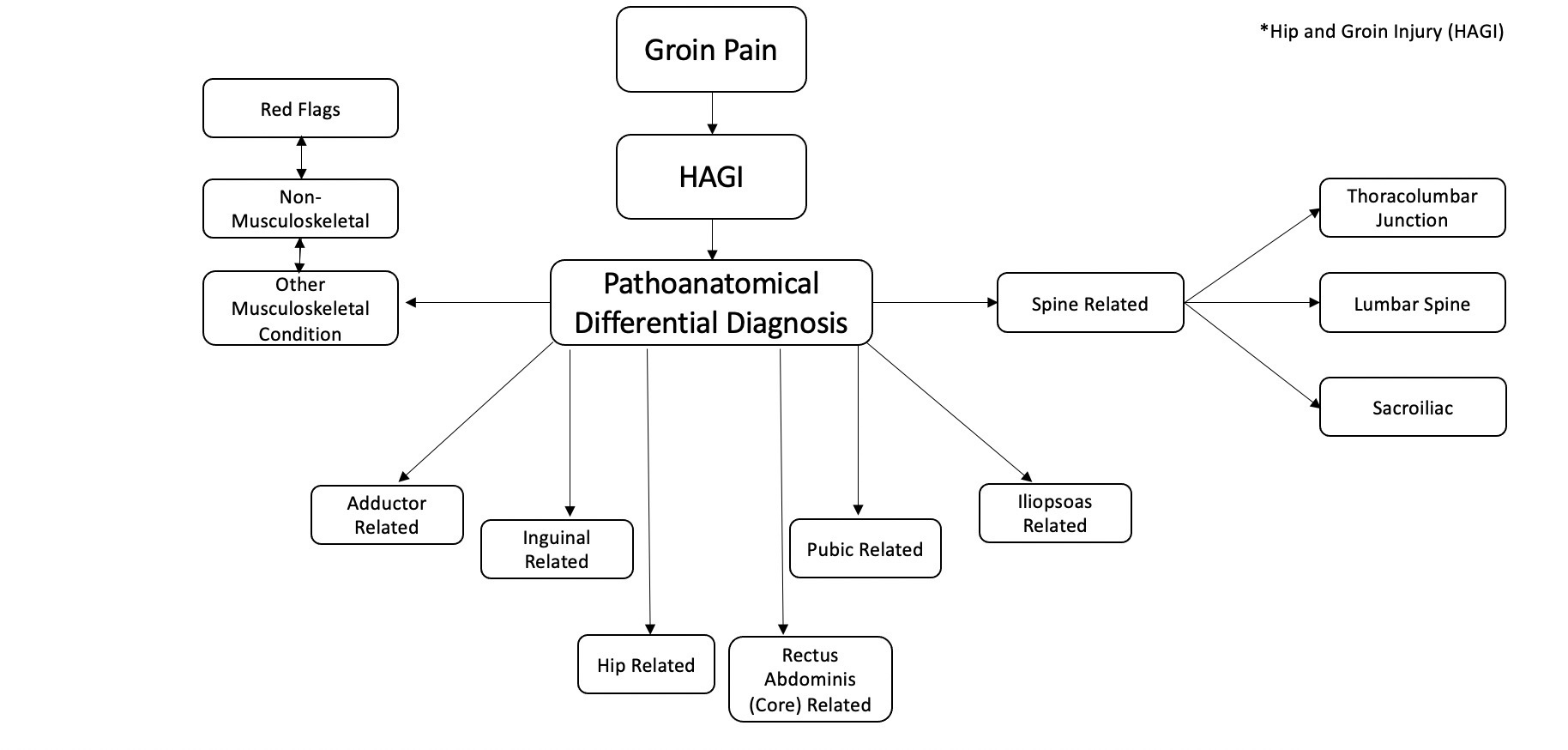
Clinical practice related to hip and groin injury (HAGI) has progressed from broad terminology (i.e chronic athletic groin pain, Gilmore’s groin, athletic pubalgia, etc) regarding diagnosis and management to highly specific subgrouping of regional diagnoses related to pathoanatomics. Recent consensus statements have attempted to define current best practice in the diagnosis and management of HAGI.1,2 While beyond the scope of this paper to explore all sources of HAGI, it is important to note some common structures and associated athletic-related pathologies. These include, but are not limited to, bony structures (femur, femoral head and neck, acetabulum, pubis) extra-articular, (adductor musculature, iliopsoas, rectus femoris), intra-articular, (acetabular labrum, acetabular cartilage, pubic symphysis), and neural structures. (Figure 1) The noted anatomy may be accordingly impacted by sprain, strain, tendinopathy, bony and/or joint stress, osteoarthritis, or a combination of pathology such as osteoarthritis and labral degeneration. Many strategies have been implemented to properly diagnose injury as demonstrated by the Doha agreement1 and have been expanded upon in follow-up clinical commentaries.3 These guidelines have recommended HAGI to be defined specifically as adductor, pubic, inguinal, iliopsoas, or hip-related groin pain.1
Improved diagnostic capabilities and clinical awareness of HAGI has likely resulted in an increased incidence and prevalence of related diagnosis, which has coincided with expanded coverage within the literature. This combination of factors suggests the presence of historical underdiagnosis,4,5 the possibility of modern day overdiagnosis,2,6 and creates the potential for bias in management strategies and reported outcomes. The heterogeneity related to the comprehensive research and management of HAGI has made best practice elusive, especially when targeting isolated structures.7,8 Syndrome-based recommendations2,9 have been endorsed to better appreciate the complex, regionally interdependent and often concomitantly pathological9–11 nature about the hip, pubis, and lumbopelvis. Regional impairments such as mobility loss, strength deficits, and altered force distribution and motor control have been associated with these defined syndromes, ultimately affecting the athletic movement system. Thus, despite the diversity of specific pathoanatomy, shared clinical characteristics such as pain referral region and aforementioned residual impairment constructs (mobility, strength, motor control, deconditioning, etc) often present irrespective of sensitized or injured structure.12–14 (Figure 2)
Considering the persistent historical challenges associated with management of HAGI, warranted attention has been growing towards mitigating its impact before an athlete becomes medicalized. Risk reduction for HAGI is a hot topic with limited reported success,15 and the available literature-base to support practical, evidence-based practices across various elite sports is often limited and biased.16,17 Current prevention strategies are generally based upon soft-tissue injury while still broadly being grouped in the HAGI spectrum.18,19 Select populations (professional and semiprofessional soccer, rugby union, ice hockey) dominate the literature upon which current evidence-based practice relies.17 Professionals practicing in sports outside of those populations and specifically within sports such as basketball, American football, or elsewhere may be presented with athletes who are currently underrepresented in the literature. Considerations that raise questions regarding the carryover of current risk identification and treatment strategies to a wide range of athletes include, but are not limited to, anthropometric and biomechanical profiles, sport specific demands (i.e volume of short space cutting and jumping volume vs time at defined high speed running, etc) and differing historical practices of sports medicine and science in a team-based setting across sports and countries.
Reviewing the Clinical Question
The New Oxford American Dictionary defines risk as the chance of unfortunate consequences by engaging in an action.20 In the case of athletics and exercise, the primary adverse event is musculoskeletal injury. The consequences of sporting injury are multifactorial, and can result in the worsening of mental and physical wellbeing as well as increasing the risk of future injury and disability. In elite sport, the consequence moves beyond individual harm, as competitive success and monetary investment are at stake.12,21 As sports medicine professionals, we have the potential to impact risk on microscopic and macroscopic scales. Our responsibility is to investigate methods to reduce the risk of the injury burden to our athletes, medical systems, and institutions. Despite what seems like overwhelming, yet diversely varying,16,17 consensuses on how to accomplish this goal, a critical investigation on injury prevention is necessary when trying to implement best practice in action for the field of play.
Caring for athletes involves navigating complex interacting systems which makes prediction and prevention quite challenging.22 Each sport exposes athletes to different risks and dynamic challenges and thus the initial steps in risk reduction are to identify common athletic demands and clinical problems. For example, in professional basketball, much effort has been put into the prevention of ankle and knee injury, as they have been identified as the most common and result in greatest time loss due to injury. Substantial attention has also been paid to catastrophic injuries, that often result in surgery, such as anterior cruciate ligament (ACL) rupture. As a result, research and clinical practice has focused on identification of related risk factor and prevention methods for such high-profile injuries. However, for example, in the National Basketball Association, all knee sprains, not just ACL tears, accounted for just 3.1% of all injuries over 17 seasons.23 Meanwhile, clinical cases of less investigated injuries, such as hip and groin injury (HAGI), have been identified as just as common, and are potentially increasing in occurence.4,23
While HAGI has been reported as 5-10% of injuries across multiple sports, in previously identified high risk sports HAGI has been reported to be a greater source of time loss, accounting for approximately 10-23% of all injury.12,18 Numerous structures within the region can be drivers of pain and injury. Additional consideration is warranted for the likelihood of concurrent pathology, injury reoccurrence, the chronicity of varying regional pathologies, and suboptimal athletic and health care outcomes.1,2 As the diagnosis and management of HAGI remains challenging, efforts should be made to investigate and improve specific injury risk reduction strategies to avert these historical challenges before they arise.
Identified Risk Factors
Highlighted non-modifiable risk factors identified in the literature include past injury history, age, time in season, and anatomy and morphology.21 While injury history and age have consistent backing in the evidence base, utilizing diagnostic imaging for identifying a priori pathoanatomic risk factors may be challenging. ‘Abnormal’ and ‘pathological’ findings about the hip and pubis, such as cam morphology2 or tendinous changes at the rectus abdominis and adductor longus origins,6 are commonly observed in asymptomatic athletes and may be sport specific adaptations. Of clinical interest are modifiable risk factors specific to the hip and groin including range of motion, hip and trunk strength, special testing, movement pattern assessment, and training variables.21,24 The evidence behind these identified risk factors and the observed difficulties in their application will be highlighted.
Analysis of ‘Modifiable’ Risk Factors
Range of Motion
Limited hip internal and external rotation in various positions, including seated, prone, bent knee fallout (flexion abduction external rotation), and the flexion adduction internal rotation (FADIR) test have all been related to HAGI. A measure of total hip rotation less than 85 degrees has also been identified as a risk factor.25 As with the consideration of total arc of motion compared to a single direction measure (such as the bent knee fall out), relative limb to limb range of motion and range of motion in sport specific positions may warrant deeper consideration as position specific findings may be related to injury.25,26 Clinical experience, unpublished data, and homogenous population data27 indicates that if clinicians are flagging ranges of motion (i.e 85 degrees total arc, bent knee fallout) as a risk factor cutoff point, nearly every athlete within select sports populations could be at risk due to limited hip mobility. In other words, if following the findings of systematic reviews,18,25 entire sporting populations would be defined as at risk of groin pain, limiting its effectiveness as a risk factor measure.
There is also a reliance on standardized ROM assessment of the hip which supports validity within studies, but may overlook the natural variance in pelvic morphology between individuals, especially when assessing hip internal rotation (IR). The natural arc of hip motion may vary between individuals due the variations in femoral version and acetabular alignment, such that an individual may demonstrate reduced hip IR in standard testing with excessive ER, but not when the individual’s natural plane of hip motion (which could be defined as hiption, similar to the concept of scaption in the glenohumeral joint) is assessed.28 Further, this measure may be impacted by the timing of data collection, as rotation has been shown to change following competition29 and may continue to be dynamic over the course of a season and career.30
Considering the prevalence of variations in athlete morphology and its complex relationship with mobility, how modifiable hip range of motion is warrants a more thorough investigation, as evidence for preventative interventions to address mobility deficits is limited and rarely included in reviews.18,27,31,32 Transient in-session range of motion increases made by modalities, manual therapy, and therapeutic exercise may be clinically important, potentially redistributing force or changing pain pressure thresholds. However lasting tissue change has not been documented nor have mobility-based intervention programs been identified as protective.32
Strength
Strength measures about the hip and trunk have been related to hip and groin pain. Of consistent interest is absolute and relative adductor strength. Common assessment methods include squeeze testing, during which a sphygmomanometer is used to measure the maximal isometric ability of the adductors in various supine positions. Other primary strength measures include handheld and isokinetic dynamometry.18,26 Low strength ratios of hip adduction to abduction, and high hip flexion to extension ratios and trunk flexion to extension ratios have all been identified as risk factors.12,26 The timing of muscle activation may be meaningful, but it has not been determined as a cause or a result of HAGI and it is currently nearly impossible to identify functional motor recruitment in sport-specific context. Furthermore, documented standardized strength assessment may not accurately measure strength variables as they relate to sport-specific tasks and associated mechanisms of injury such as defensive shuffling, kicking, single leg jumping, or how an ongoing strength profile improves any tissue’s capacity to handle such tasks. Simple strength metrics have been shown to vary according to population,33 morphology,27 timing,34 presence of pain,33 fatigue,34 and many other factors indicating a need for clinical reasoning for interpretation and application.
Similar to hip range of motion, a clinical challenge of applying strength data is that current reference data is likely population and context specific. Most documented strength assessments are performed prior to competitive seasons and not intra-season. The differing sporting and training demands, as well as differences in athlete’s biomechanical profile (i.e mechanical advantage according to leg length when performing long lever squeeze assessment) likely limits clinicians ability to interpret and apply normative data across sports, as empirical analysis of subgroup scores are quite different from current published values.33 If strength is assessed in-season or following competition, whether immediately or next day, there are minimal recommendations on the best ways to interpret or act on such information, particularly when considering congested competition schedules during which optimal recovery from intense activity is impaired.34–36
Special Testing
Special testing often combines elements of range of motion and strength for symptom provocation and the tissue and/or system impairments as they relate may indicate a level of risk for example squeeze testing37 and the FADIR test.38 Consistent monitoring of special tests may identify significant variance in prior findings and could be related to training volume or pain.34,39 These tests provide value for daily clinical reasoning in a dynamic test-retest model, but since these tests generally identify sensitized actions, structures, and/or movements, they are currently more valuable once the athlete is already nursing an injury as opposed to providing prognostic value.
Movement Assessment
Clinical movement assessments have been found to have minimal utility in identifying those at risk for hip and groin injury, despite potential construct validity. It has been shown that those with HAGI demonstrate different movement patterns in tasks of varying intensities compared to controls.40,41 Differences have been identified in star excursion balance test of posterolateral reach and altered intersegmental biomechanics in various cutting tasks in those with HAGI.42,43 Variable movement patterns during a cutting task have not been established as predictive of HAGI, however changes in these patterns, in addition to improved adductor strength, have been shown to occur with intersegmental-focused training when returning from a prior HAGI.43,44 It is unclear whether this assists in the cause of the resolution of injury or is changed due to the absence of pain and natural history. While training movement patterns is often a focus in physiotherapist practice, it warrants questioning whether changes in multi-segmental control and/or movement patterns transfers to sport specific and reactive variations of movements, or if changing asymptomatic movement patterns may provide a protective stimulus, and even potentially provide a false level of comfort to the clinician and athlete. With or without symptoms, it has been shown that efficient force distribution about the pelvis is recommended (i.e avoiding excessive trunk lean displacement, excessive displacement beyond the center of mass) and may have implications with HAGI.43–45
Monitoring Load and Objective Outcome Measures
Monitored training variables and resultant outcomes of sport training such as body composition, aerobic fitness, and sport-specific training load volume has been reported as related to injury risk. Load monitoring strategies vary greatly and include internal (physiologic) or external (mechanical) variables.46 For other highly studied injuries, such has hamstring strain, variables such as distance covered and high-speed running metrics have been documented as injury risk factors.39,47,48 It has been proposed that these factors should be applied across sports and injuries, without consideration of the differing demands of various sports.47 Court athletes may never achieve similar high speeds or distances as field athletes, while being stressed by different mechanical forces and associated physiologic consequences associated with tasks such as high volume jumping or limited-space, high intensity cutting maneuvers.49 Sport specific preparation has been identified as a common risk factor, thus, an importance must be placed on defining and training these identified variables, yet are not commonly detailed in the literature, training or in sporting practice.49 In order for sport-specific training to be provided, these qualifiers must be defined, tested, and trained to evaluate their potential protective capacity.50 Practical challenges are numerous when attempting to consistently collect and utilize objective outcome measures,49 especially when considering clinical time demands, the substantial size of data sets, the impact of internal and external factors in elite sport, and the numerous athlete health and performance demands aside from HAGI that present in daily practice.
Practical Gaps in Screening
Despite significant investigation, much debate continues to take place regarding the value of screening for athletic injury risk factors and its effectiveness has been extensively questioned.24,51 Current evidence pertaining to heterogenous HAGI risk factors is often disproportionately represented from select homogenous populations. Derivation of risk factors frequently relies on retrospective study design as opposed to more rigid prospectively designed trials. The lack of prospective studies is not shocking, as data collection and application in elite sport presents numerous practical challenges, including appropriate design, collection, sharing, and publication of relevant data.24,51 The culture and history of each individual sport presents with varying attitudes and opportunities to cultivating and prioritizing the development of research practices.49 These limitations leave questions as to whether or not sample sizes are robust enough to hold clinical value, if specific qualities are the result of, or potential cause of injury, if these factors are able to be shared across various sports and genders, or if risk reduction research and development can even take place in environments of interest.49
Intervention Over Identification
As opposed to a narrow focus on isolated risk factors, reducing the occurrence of hip and groin injury or otherwise may be best served by focusing on global neuromuscular training combined with individualized and context- specific ‘prevention’ programs that avoid training load error.52 With shared regional factors (mobility, strength, motor control, altered force distribution, tissue tolerance, etc) about HAGI, global principals are appropriate to apply to mitigation programs. Ultimately, achieving less injury may rely on an adequate volume and adherence of training in these risk reduction strategies, most specifically, appropriately dosed and performed exercise.32,53 Despite this working hypothesis, a general well planned, balanced, and executed multi-component exercise training program may be protective regardless of the targeted constructs listed above.15 Developing numerous qualities within the variables of strength and aerobic capacity may be key modifiers in decreasing an athlete’s risk for HAGI regardless of underlying proposed risk factors defined earlier in this paper.53–55 Objective data obtained historically via traditional screening methods may not be predictive in a classical prevention ideology, but may continue to hold secondary value in establishing baselines profiles, and be used to monitor progress and changes in the athletes dynamic system to inform clinical reasoning and athlete care.34,39,46,56,57 Monitoring profiles of strength and exercise load metrics are emerging as recommended evidence-based practice for secondary risk reduction allowing for clinicians to make real-time programming decisions to reduce risk.34,39,57 The nature of dosing requires further investigation,58 as an adequate baseline and minimal effective dose of exercise may serve as protective.59 Timing the dose as it relates to match day and in relation to activity timing may provide improved adherence and effectiveness.59–62
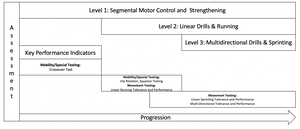
Again, despite the heterogeneity of the pathology of HAGI, it is valuable to note the homogeneity of physiotherapist intervention. Education, assessment, exercise, movement training, appropriate mobility intervention, optimal dosing of intervention, and continued monitoring have all been commonly recommended in the comprehensive management of various hip joint, osseous and soft-tissue related injuries.63 (Figure 3) Similarly, mobility, hip strength, and motor control are constructs that can be defined respectively as risk factors, injury impairments and rehabilitation goals.43,56 (Figure 4) The authors recommend that these same constructs be appropriately implemented into future focused risk reduction programs (Figures 5 and 6). As these trainable constructs have been consistently identified across the HAGI spectrum,43 targeting them appropriately could have a mediating effect on past and/or future injury.35,56 By focusing on these factors and treating each individual with respect to their sporting demands and body’s specific natural adaptations,64 it may be possible to develop clinical guidelines for HAGI reduction similar to what has been done regarding ACL prevention.65 As evidence-informed recommendations have been globally applied to comprehensive knee injury reduction,65 with further development, the same could be done for HAGI. The nature of global training principles may result in significant similarities between these programs, which is to the benefit of their application.
Of course, the remedy is not as simple or as straight forward as it may seem. Similar to the discussion of highlighted risk factors above, the efficacy and effectiveness of these programs remains limited to the sports in which they have been trialed via the scientific process, integrated, individualized, and accepted as common practice. For example, detailed general programs have been trialed in sports such as European football but few other team based sports.15–17,52 This has been most recently identified in a systematic review detailing the challenges of finding level 1 evidence in elite sport and then applying strategies of lower levels of evidence with high levels of bias.16,17 Transference troubles have been seen clinically in recognized pathology-based prevention programs such as neuromuscular training to reduce knee injuries. Many such programs have been established related to a specific gender and age population (adolescent females) and mechanism of injury may be dissimilar when comparing across sports, gender, and sporting maneuvers65,66 (i.e dynamic valgus produced by jump landing vs change of direction task).
Conclusions
Identification of injuries with high incidence and prevalence within sport is common practice and leads to investigation of prevention, and more practically, risk reduction. In the case of HAGI, practitioners continue to rely on generalized risk factors and select populations to provide current best practice despite the growing number of identified HAGI cases. Athletes across sports possess inherent characteristics that predispose them to specific sporting success, and may require a diverse set of risk modifying interventions to increase the odds of prolonged health and sports participation. In order to further improve these programs, the authors extend a call to action to refine important clinical questions and extensively test them in order to advance the practical evidence-base which may improve athlete health. This requires creating integrated institutions and avenues within all levels (youth, collegiate, semi-professional, professional) and geographical locations (including the United States) of sporting populations. This call to action can begin by proactively implementing current evidence-informed interventions, such as global exercise programs with injury-specific construct modifications, within diverse sporting populations. Assessing the residual outcomes and modifying programs accordingly could reverse trends of increasing HAGI in understudied populations. Until then, recommendations and practice will rely on clinical experience and at times liberal interpretations of practice across sporting populations.
Conflict of Interests
Authors declare no conflicts of interest