Introduction
The single leg squat test (SLST) is a functional performance test that is used by clinicians and researchers to assess neuromuscular performance of the trunk and lower extremity. The SLST is commonly used for injury prevention screening and physical rehabilitation evaluation. The test has been applied to individuals with non-arthritic hip pain,1 patellofemoral pain syndrome,2–6 knee osteoarthritis,7 and anterior cruciate ligament (ACL) reconstruction.8,9 Excessive medial knee deviation (MKD) during the eccentric phase of the squat is a common finding10,11 and is used as a marker of aberrant movement patterns in both visual rating scales12–16 and kinematic measurements.13,17–19 The presence of increased MKD has been related to common lower extremity dysfunctions such as non-arthritic hip pain,20 anterior knee pain,21–23 and increased risk of noncontact ACL injury.24,25
Clinicians26–28 and reseachers29,30 commonly associate excessive MKD with poor motor control of the muscular structures proximal to the knee joint. It has been determined that individuals who display excessive MKD during single limb standing activities utilize different activation patterns of the hip abductors31 and adductors, 31,32 and demonstrate differences in strength measures of the hip extensors,33,34 lateral rotators,33–35 and abductors.29,34 This “top-down” rationale for MKD leads clinicians to implement treatment programs that emphasize hip-focused neuromuscular control and strength training.26–28
Another possible explanation for MKD, however, is that it could occur as a result of impairments at the foot and ankle. This “bottom-up” approach to explaining MKD may be associated with abnormal foot posture,36 such as increased/decreased medial arch height, excessive calcaneal inversion/eversion, or differences in talonavicular bulge. Abnormal foot posture has been reported to influence the biomechanics of the lower extremity during weightbearing37,38 and has been related to proximal musculoskeletal dysfunction such as low back pain,39 knee pain,40,41 and hip pain.42,43 Given the associations between foot posture, weightbearing biomechanics, and proximal musculoskeletal dysfunction, it is possible that foot posture may be a factor in performance of the SLST.
Ankle range of motion (ROM) may also influence proximal movement patterns in the closed kinetic chain.31,44 Sagittal plane ROM restrictions of the lower extremity joints have been associated with the presence of increased MKD during weight-bearing functional performance tests.45,46 Decreased passive ROM into ankle dorsiflexion with the knee flexed31 and extended31,44 has been reported in individuals that perform the overhead squat44 and the single leg squat31 with excessive MKD. However, the evidence regarding the association between ankle dorsiflexion and MKD is not definitive. Both Bell et al.33 and Dill et al.47 found no relationship between MKD during functional tests and ankle dorsiflexion ROM. This conflicting evidence suggests that more study is needed to understand the association between ankle dorsiflexion ROM and MKD during weightbearing functional tests.
The lack of evidence relating ankle dorsiflexion ROM and foot posture to MKD during weightbearing functional tests may impact clinical practice. Individuals who have normal strength and activation of muscles of the hip and who do not improve in their ability to perform a SLST with a “top-down” focused rehabilitation program may have contributing foot and ankle impairments, such as restricted ankle dorsiflexion ROM or abnormal foot posture. Therefore, the purpose of this study was to compare ankle dorsiflexion ROM and foot posture in subjects that perform the SLST with MKD (fail) versus without MKD (pass). The primary hypothesis was that subjects that failed the SLST for MKD would have different foot posture and/or a different amount of active ankle dorsiflexion ROM than those that did not fail for MKD.
Methods
Study design
This was a cross-sectional, laboratory-based investigation that compared ankle dorsiflexion ROM (non-weight bearing with the knee extended (DF-NWB-ext), non-weight bearing with the knee flexed (DF-NWB-flx), and weight bearing using the weight-bearing lunge (WBL)) and foot posture between those that perform the SLST with and without MKD. Based on previous work on the association of ankle dorsiflexion range of motion with MKD during the SLST, power was calculated to be 80% with 26 subjects per group, at an alpha level of 0.05, with an effect size of 0.70.31 Subject recruitment and data collection took place from August 2019 to December 2019. This study was undertaken with approval from Duquesne University’s institutional review board.
Subjects
Healthy, active volunteers were recruited for this study. To be included, subjects had to be between the ages of 18 and 45 years, report an activity level of 3 on the Tegner Activity Scale, be able to: 1) perform a vertical drop jump; 2) complete the screening protocol; and 3) read and communicate in English. Subjects were excluded if they had inadequate hip muscle function as measured by the following criteria: 1) unable to maintain single leg stance for 30 seconds without a Trendelenburg or compensated Trendelenburg posture; 2) <4/5 hip abductor strength on the test extremity by manual muscle test. Subjects were also excluded if they: 3) were pregnant; 4) experienced a lower extremity injury on the side being tested within the prior six months that limited activity for 2 days; or 5) underwent lower extremity surgery on the side being tested in the prior year. (Table 1)
Procedures
After providing informed consent, subjects reported their age, sex, height, and weight and then completed the Tegner Activity Scale and the Lower Extremity Functional Scale (LEFS). Subjects then completed the dominant extremity test and screening protocol. To determine dominant extremity, subjects performed five unilateral drop jump landings using a previously published protocol.48 The lower extremity that was chosen for landing in 3 of 5 landings was determined to be the dominant extremity and used for testing.
After this, each subject participated in a screening protocol to determine whether they had grossly sufficient balance, neuromuscular control, and hip abductor strength to perform the SLST. The screening protocol consisted of three tasks: (1) 30 seconds of single leg stance on the test extremity; (2) five squats performed in a bilateral fashion; (3) manual muscle test of the hip abductors. During the single leg stance test, subjects’ balance and ability to maintain a level pelvis and neutral trunk were assessed so that balance and gross strength deficits of the hip abductors could be clinically ruled out as contributors to MKD on the SLST. Subjects failed this portion of the screening test if they touched the floor with the non-dominant extremity or if a Trendelenburg/compensated Trendelenburg position49 (Figure 1A-B) was identified by the investigator (LC).
If subjects failed this portion of the testing due to loss of balance, they were given a second opportunity to pass. If subjects failed on the second trial, they were excluded from the study. The second portion of the screening protocol consisted of subjects performing five bilateral bodyweight squats to approximately 90o of knee flexion in order to determine whether the subject was physically capable of performing the SLST.50 The investigator (LC), a practicing physical therapist with over nine years of clinical experience and board certification in orthopedic physical therapy, excluded subjects if the squats were performed with gross asymmetry, poor control, or aberrant movement patterns that would preclude them from being able to perform the clinical SLST protocol. If subjects passed the bodyweight squat test, a manual muscle test of the hip abductors51 was performed to ensure that included subjects had at least 4/5 strength. (Figure 2)
After passing the screening process, subjects were instructed in the evidence-based SLST protocol.12 This SLST protocol was developed in a systematic review of 42 peer-reviewed and published manuscripts12 and was chosen for this study because it is reflective of how the SLST is commonly performed clinically. This protocol does not require equipment or time-consuming set-up and visual assessment of subject performance has been shown to be reliable.20 To perform the SLST, a “T” (6" horizontal, 10" vertical) is taped on the floor using 1.5" wide athletic tape. The subject stands on the vertical tape on their barefoot test extremity and flexes the other knee to 90o. The subjects are then instructed to squat until they can no longer see the horizontal tape in front of their toes and then return to the starting position. (Figure 3A-B) Subjects were permitted to practice the SLST protocol until they felt comfortable with the instructions.
Subjects were then asked to stand barefoot in their usual posture so that the investigator (LC) could perform the Foot Posture Index (FPI-6) on the test extremity. The FPI-6 is a validated, systematic clinical examination of 6 aspects of static, bilateral weight-bearing foot posture: observation of calcaneal position, arch height, number of visible toes, talonavicular bulge, supra- and infra- malleolar concavity; and palpation of the talar head.38,52 Foot posture is scored from -12 (very supinated foot) to +12 (very pronated foot), and a score of 0 is a neutral foot. The FPI-6 has shown acceptable intra- and inter- rater reliability (ICC = 0.81 – 0.86).37,53
Ankle dorsiflexion ROM measurements were then taken using three different techniques: (1) active, non-weight bearing, subtalar neutral, with the knee positioned in 0o of extension (DF-NWB-ext), (2) active, non-weight-bearing, subtalar neutral, with the knee flexed to 90o (DF-NWB-flx), and (3) weight-bearing lunge test (WBL). These measurements were chosen based on their clinical relevance and their use in previous studies.31,33,44,47 Non-weight bearing measurements were taken using a 12-inch universal goniometer (Sammons Preston Rolyan, Bolingbrook, IL) and the weight-bearing measurement was taken with a digital inclinometer (Baseline, Fabrication Enterprises Inc., New York, NY). DF-NWB-ext was measured in long sitting with the knee extended to 0o and DF-NWB-flx was measured in prone with the knee flexed to 90o. For both DF-NWB-ext and DF-NWB-flx, subjects were asked to perform maximal active ankle dorsiflexion, were positioned in subtalar neutral by the investigator, and then range of motion was measured with a goniometer.54,55 (Figure 4A-B) For the WBL, participants placed their test extremity on a piece of athletic tape that was placed perpendicular to a wall. Subjects were instructed to keep their toes and heel on the tape in order to prevent toe-out or toe-in positioning during the measurement. The digital inclinometer was placed 15cm below the tibial tuberosity56 and subjects were instructed to lunge forward on the test extremity until their heel began to lift off the floor. Participants informed the investigator when the heel began to lift off the floor and the amount of dorsiflexion present at this time was recorded. (Figure 4C) All dorsiflexion measurements were performed by one investigator (LC), who took three measurements in each position. The average of the three measurements was used for analysis. Intra-rater reliability was excellent for all of the dorsiflexion measures (DF-NWB-ext: intraclass correlation coefficient (ICC(3,3)) = .909, standard error of measurement (SEM) = 1.043o; DF-NWB-flx: ICC(3,3) = .967, SEM = .984o; WBL: ICC(3,3) = .885, SEM = 2.535o).
Subjects then performed five repetitions of the single leg squat while being video recorded using an iPad Pro 11" (Apple, Cupertino, CA). The iPad Pro was held two meters in front of the subject and 0.9 meters from the floor. Videos were analyzed for group assignment by two independent physical therapists (one with 20 years of clinical experience in outpatient orthopedics and board certification in orthopedic and sports physical therapy (BK); and another with five years of clinical experience in outpatient orthopedics and board certification in orthopedic physical therapy (AD)). These researchers were blinded to subjects’ other data points. Subjects whose patella deviated medial to the second toe on 3 of their five squat attempts were placed in the fail group. All other subjects were placed into the pass group. Raters met to review discrepancies and together determined subjects’ final group assignment so that there was complete agreement for final group assignment.
Statistical methods
Statistical analysis was completed using SPSS Statistics version 26 (IBM Corporation, Armonk, NY). The pass and fail groups were compared using independent samples t-tests for age, BMI, and Tegner Activity Scale score. LEFS scores were compared using a Mann-Whitney U test and a Chi-square analysis was used to compare the distribution of sexes between groups. The three measures of dorsiflexion ROM (DF-NWB-ext, DF-NWB-flx, WBL) were expected to be correlated and were analyzed using a MANOVA. FPI-6 scores were analyzed separately using an independent samples T-test, as FPI-6 scores were not expected to correlate with the ROM scores. All statistical assumptions for data on the variables of FPI-6, DF-NWB-ext, DF-NWB-flx, and WBL were met.
Results
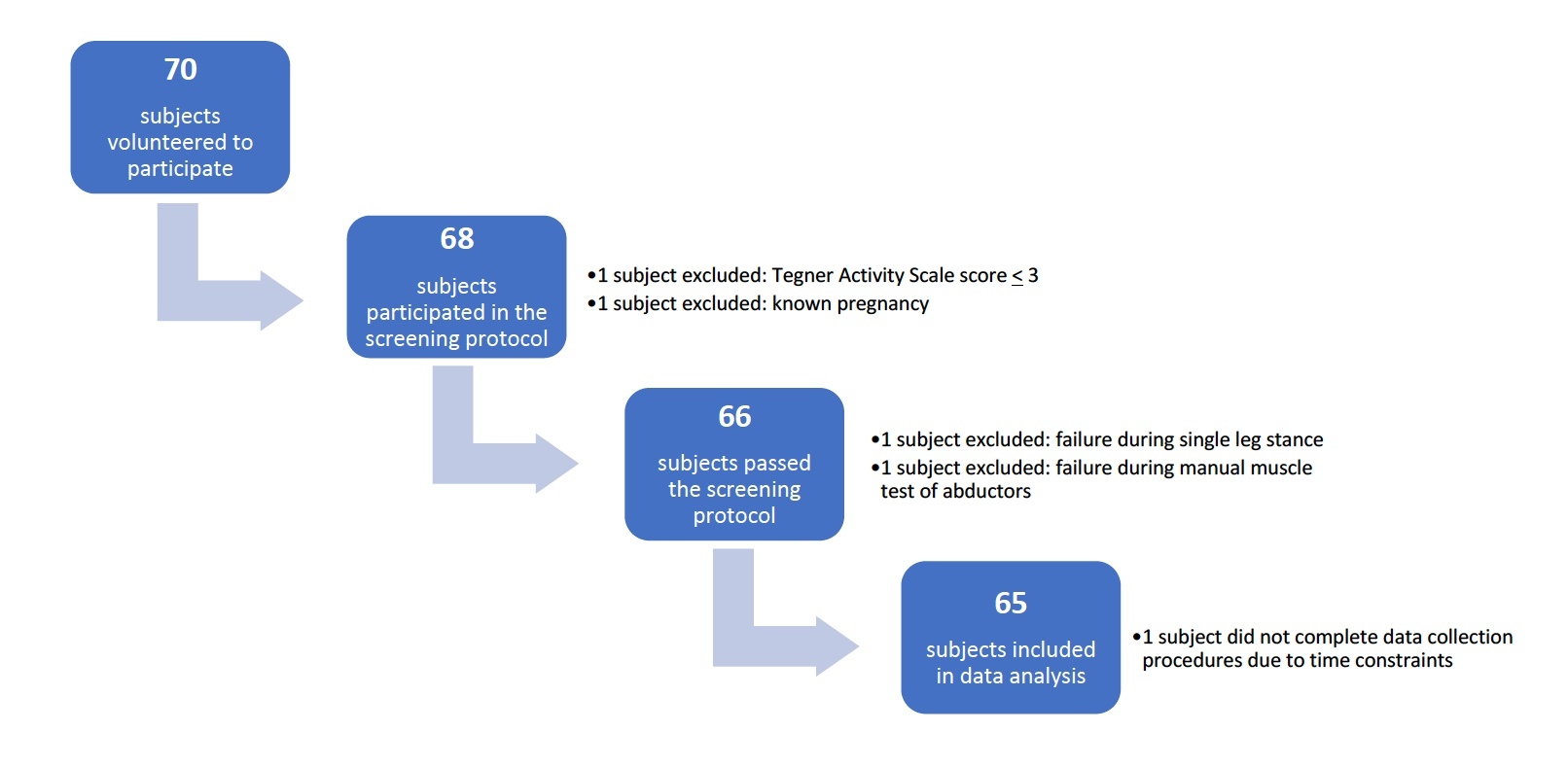
Seventy subjects were recruited for the study and data from 65 subjects was used for the analysis. One subject was excluded due to pregnancy, one was excluded because they did not score 3 on the Tegner Activity Scale, two subjects were excluded due to failure during the screening protocol, and one subject was excluded because they were unable to complete data collection due to time constraints. (Figure 5)
There were 32 subjects in the fail group and 33 subjects in the pass group. According to independent samples T-tests, the pass and the fail groups were similar in age (p = .899), sex (p = .341), BMI (p = .818), and Tegner Activity Scale score (p = .456). There was a statistically significant difference between the groups on LEFS score (p = .002). However, this result is not likely clinically meaningful, as median scores for the LEFS were 80 in each group and 100% of subjects in the study scored within the same range of minimal clinically important difference (9 points).57 Means, standard deviations, and levels of statistical significance for these variables are summarized in Table 2.
The dorsiflexion ROM measures (DF-NWB-ext, DF-NWB-flx, WBL) were found to correlate moderately (r = .497 - .764) and were analyzed using a MANOVA. The MANOVA revealed that there were no differences in ankle dorsiflexion ROM between the groups (p = .611). The FPI-6 did not correlate with the dorsiflexion ROM measures (r = .012) and was analyzed separately using an independent samples T-test. Foot posture was also not different between those that failed and passed the SLST for MKD (p = .599). Means, standard deviations, and significance levels for the clinical characteristics of the foot and ankle are summarized in Table 3.
Discussion
The most important finding of this study was that there were not significant differences in clinical measures of ankle dorsiflexion ROM or foot posture between subjects that passed versus failed the SLST for MKD. The hypothesis of this study was therefore not supported. These results are supported by previous work that has shown that ankle dorsiflexion was not a factor in MKD during other forms of weight bearing functional testing.33,44,47 The current findings indicate that MKD on the SLST may not be attributed to differences in dorsiflexion ROM or foot posture and support the continued use of the SLST to assess neuromuscular performance of the trunk, hip, and knee.
The key findings of this study that ankle dorsiflexion ROM measures are not different in subjects that perform a functional test with and without MKD are supported by published evidence. Previous work has shown that measures of non-weight bearing/knee extended ankle dorsiflexion,33,47 non-weight bearing/knee flexed ankle dorsiflexion,33 and weight-bearing ankle dorsiflexion47 ROM were not significantly different in individuals that performed the overhead squat with MKD versus those that performed the overhead squat without MKD. Additionally, Dill et al47 found no differences in MKD during a double-legged jump landing task or during the SLST between subjects with limited versus normal non-weight bearing/knee extended ankle dorsiflexion or weight-bearing ankle dorsiflexion measures.
The evidence-based SLST protocol that was used in this study is reflective of typical clinical use of the SLST: subjects’ performance was assessed visually and squat depth was not formally measured. Previous research that reported a difference in ankle dorsiflexion ROM in subjects that failed the SLST utilized varying SLST protocols that required measurement of squat depth to 60o of knee flexion.31,44,46 It is possible that performing the SLST to 60o of knee flexion may engage near end range ankle dorsiflexion and may result in frontal and transverse plane compensations that have been reported to occur with restricted sagittal plane motion.45,46 Without squatting to a depth that reaches near end range ankle dorsiflexion, increased MKD is unlikely to be impacted by restricted ankle dorsiflexion ROM. Although kinematic data was not gathered during this study, Ageberg et al.58 utilized a similar SLST protocol and reported squat depth to be less than 45o of peak knee flexion. Ankle dorsiflexion kinematics and ROM measures were not reported in Ageberg et al.'s study, so it is unclear whether patients reached end-range of dorsiflexion.58 However, a separate study by Whatman et al.59 reported an average peak knee flexion angle of 65o when subjects were asked to perform a unilateral squat until they reached end-range dorsiflexion. The summary of these findings suggests that, in the current study, subjects likely did not squat to a depth that engaged end-range ankle dorsiflexion and that the observed increase in frontal and transverse plane movement may not be attributed to sagittal plane ROM restrictions of the ankle.
Although an attempt to control for neuromuscular deficits at the hip was implemented for the current study, increased MKD during the SLST is likely related to proximal dysfunction that was undetected by the utilized screening protocol. The use of surface electromyography or handheld dynamometry with normalization to body mass may have better elucidated the proximal neuromuscular deficits contributing to MKD during the SLST. Proximal impairments, such as differences in maximum force production,34,35 isokinetic torque,29 and activation patterns13,16,31 of muscles of the hip have been reported in individuals that fail the SLST. Further support of this “top-down” approach to assessing SLST performance can be seen in intervention studies in which treatments targeting proximal muscle function have been shown to improve SLST performance.1,60,61 These factors indicate that the evidence-based SLST protocol used in the current study and commonly implemented in the clinic may best be used to assess proximal, rather than distal, contributors to functional movement of the lower extremity kinetic chain. Furthermore, the results suggest that clinical screening of hip abductor strength by manual muscle test and Trendelenberg test is not adequate to detect a dysfunction that may result in MKD during the SLST. The results of the current study support the continued use of the evidence-based SLST to assess neuromuscular performance of the trunk, hip, and knee not otherwise detected by manual muscle test and Trendelenberg stance without dorsiflexion ROM and foot posture impacting results.
There are limitations to this investigation. First, this study was performed using young, healthy subjects (mean age = 25.2 +/- 5.6 years, range = 19 – 45 years), so results may not be generalizable to populations with musculoskeletal dysfunction or of older or younger age. This study was also limited because the sample was 77% percent female. Although the distribution of sexes between the pass and fail groups was not statistically different, utilizing a sample that is predominantly female could have impacted the study’s results, as there have been reports that females and males may perform the SLST differently.17,35,62 Additionally, this study was designed to be clinically applicable through the use of common clinical tests and measures, such as goniometry and the FPI-6. The error in some of these measurement techniques and tools is high63 and could have impacted the results of the study. A 6o - 8o change in lower extremity goniometric measurements is needed in order to consider the differences clinically meaningful.54,64 Given the relatively small range of physiologic motion available into ankle dorsiflexion (20 degrees65), it is possible that goniometry is not precise enough to detect differences that may exist between groups. Furthermore, the measurement of active non-weight bearing dorsiflexion and passive weight-bearing ankle dorsiflexion resulted in a wide range of ROM measurements being recorded. The use of the bilateral FPI-6 is another limitation to this study. The FPI-6 measures foot posture in static, bilateral weight-bearing and an individual’s score on the FPI-6 may not be reflective of their foot posture or function in unilateral stance or during a dynamic unilateral task, such as the SLST. Motion capture data showing triplanar foot and ankle kinematics may offer more information regarding foot and ankle movement during the SLST. Another limitation to this study is that, although the authors attempted to control for factors such as hip muscle strength and balance through the screening protocol, proprioception, muscle performance, or muscle activation was not directly compared between the pass and fail groups. It is possible that the demands of the SLST are greater than those of the screening protocol used in this study and that differences between the pass and fail groups could be due to these factors.
Recommendations for future research
This study showed that ankle dorsiflexion ROM and foot posture were not different between healthy subjects that perform the SLST with and without MKD. Future work should investigate SLST performance in individuals with foot and ankle dysfunction, as it has been reported that MKD during the SLST is a risk factor for ankle injuries.11 Additionally, because the ease of use of the evidence-based SLST protocol makes it attractive to clinicians and researchers alike, further investigation into its kinematics, associated muscle activation patterns, and related muscle performance is warranted.
Conclusion
Among healthy individuals that passed and failed the SLST for MKD, there were no significant differences in clinical measures of weight bearing and non-weight bearing ankle dorsiflexion ROM or foot posture. These findings refute the possibility of a “bottom-up” approach to explaining increased MKD during the SLST in healthy individuals. Based on the results of this study, clinicians should not use the clinical SLST protocol to detect differences in the clinical characteristics of the foot and ankle. However, clinicians may continue using the clinical SLST protocol to assess function in individuals with non-arthritic hip pain regardless of their ankle dorsiflexion ROM or foot posture.
Conflicts of interest
The authors declare that there is no conflict of interest.


_protocol._a._starting_position.png)

_and_a_digital_incl.jpeg)


_protocol._a._starting_position.png)

_and_a_digital_incl.jpeg)