INTRODUCTION
A key goal within sports medicine is to improve the outcomes of patients after major injury. It appears that many patients fail to return-to-sport (RTS) and/or previous sporting performance levels after anterior cruciate ligament reconstruction (ACLR).1–4 Those who RTS, do so often at much elevated risk of re-injury, with typically around nearly one in three young athletes experiencing a knee re-injury,5,6 generally within the first two years after RTS.7 Current opinion is that in order to improve athlete outcomes after ACLR, there is a need to optimize the processes and practices of rehabilitation.8,9 Key areas suggested in need of improvement are the restoration of neuromuscular performance (e.g., strength and power) and movement quality of patients prior to RTS after ACLR.8–11 Following ACLR, at the time of RTS, patients often present with deficits in knee extensor maximal strength12–14 and rate of force development (RFD),15,16 as well as lower limb/closed chain strength15 and power.17 Furthermore, patients often RTS with movement asymmetries during an array of functional tasks18–23 thought to predispose them to increased risk of injury.7,24–26
One highly valued element of rehabilitation after ACLR is the use of plyometric training.8 Plyometric exercises involve a stretch-shortening cycle, which is a commonly observed phenomenon involving a rapid lengthening of a muscle tendon unit, immediately followed by a rapid shortening (for a review see Davies et al.).27 Plyometric training has long been used to optimize explosive sporting performance (e.g., speed, jump height) of athletes and is regarded as an excellent training method, due to the wide ranging neuromuscular and motor control benefits.28–32 In particular, plyometric training has been reported to be superior to more traditional resistance training for development of explosive lower limb performance (power/RFD),30,31,33 as well as effective at eliciting gains in maximal strength,32 and sports performance variables, such as linear34 and multiple directional29 movement speeds.
Ebert et al.35 reported that only 30% of patients completed a plyometric program prior to RTS after ACLR.35 A key issue with implementing plyometric training into the functional recovery process of ACLR patients is a lack of guidance within the literature on how and when to do it. Plyometric tasks vary in their intensity and specificity, with typical peak ground reaction forces (GRF) ranging from 1.5-7 times body mass.36–40 Inappropriate plyometric task choice could thus be expected to cause adverse reactions on an unprepared person after major lower limb injury. There is a need to support practitioners on how to effectively use plyometrics after major lower limb injury, such as ACLR. To do this, there is a need to understand the types of plyometrics available, their relative loading/intensity and understand how to systematically incorporate plyometric training as part of the ACL functional recovery pathway. Therefore, the aim of this paper is to provide recommendations to clinicians on how to design and implement plyometric training programs for the ACLR patient, as part of the functional recovery process. This will hopefully aid a reduction in the barriers between research and effective implementation into practice.
PLYOMETRIC TRAINING AFTER ACL RECONSTRUCTION – KEY CONSIDERATIONS IN PROGRAM DESIGN
Designing a plyometric training program to develop neuromuscular performance and movement quality, while respecting tissue healing, is an important consideration for the rehabilitation specialist.9,41 In planning effective plyometric use and progressions, it is important to have consideration of optimal loading (defined as the load applied to structures that maximizes physiological adaptation)41 to bring about specific neural, morphological and mechanical adaptations.41 Optimal plyometric program design entails an understanding of the specific loading demands of the various plyometric tasks, so a series of optimal progressions can be planned. It is important to consider the intensity of movement or the specific external and internal loading of the task(s). External forces are the result of equal and opposite forces acting on the body according to the laws of motion (e.g., Newton’s laws), while the internal joint loads will depend on how the GFR loads are distributed throughout the body. Load is actively accepted/dissipated via the neuromuscular system and absorbed passively via the tendons, ligaments and joints during movements. Internal hip-, knee-, and ankle-extension (plantarflexion) moments must be produced via eccentric, isometric and concentric muscle contractions to control joint motion, absorb the kinetic energy of the body at impact and produce force and power to propel the body ballistically during plyometric tasks.42 Inability to accept load either due to deficits in strength, would mean a greater reliance on joint complexes (tendon, ligament and joint structures) for passive force absorption.43 It is important to understand the specific loading demands of the various tasks, the patients capacity to tolerate these loading demands (e.g., strength and movement quality) and understand how the patient has responded to the specific loads on an individual level (e.g., monitoring loading response).
Plyometric task intensity and complexity
In terms of plyometric loading, it is important to consider the peak external loads of the tasks, the joint specific internal moments, the neuromuscular activation/muscle forces as well as the neuromuscular control challenge. In addition, consideration of volume load is important.
During movement, an individual must produce and accept force via its application to the ground according Newtons laws of motion. Newtons third law dictates that there will be an equal and opposite reaction, whilst Newtons second law, the law of acceleration, dictates movement acceleration will be a product of force application relative to body mass (Force = mass x acceleration). Intensity of plyometric tasks can be considered on the basis of peak GRFs, which typically occur during the eccentric/landing phase, but also peak concentric forces (and power) are important on a performance level. In addition, the rate of force acceptance and development is important. This is essentially the rate of change in force during the landing and jumping phases of a plyometric task.
Peak external loading is largely dictated by task selection, the neuromuscular capacity to accept and develop force (e.g., strength), surface/environment and ground contact time (GCT)/instruction:
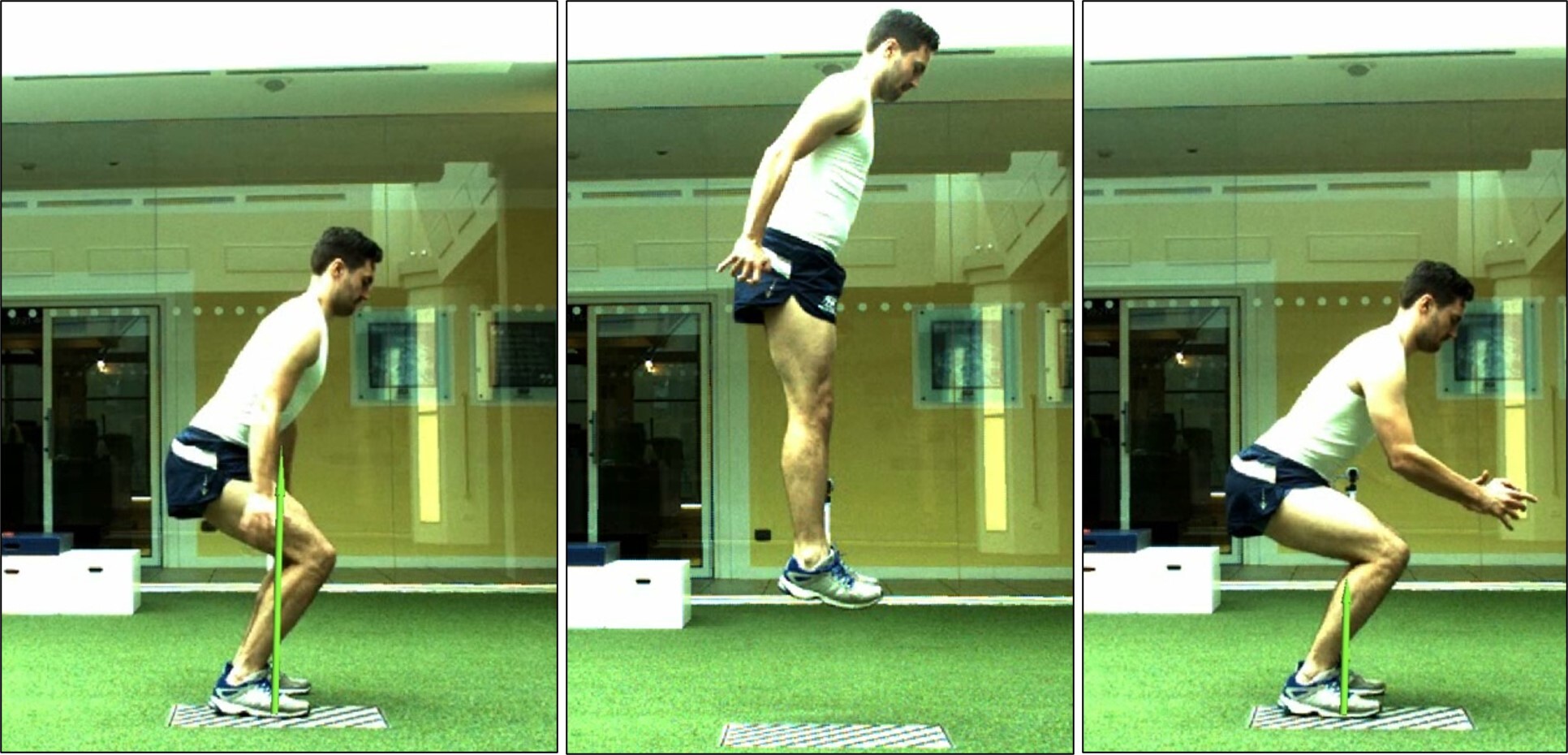
i) Task selection: Plyometric tasks can be considered based on stance and body positioning at take-off/landing, consisting of unilateral and different bilateral versions (Table 1 and Figure 1). During the eccentric phase of a plyometric task, the athlete will need to decelerate the center of mass, prior to producing force and power to ballistically propel oneself as part of the plyometric action. The peak eccentric forces will largely be dictated via the velocity or the relative momentum of the system, as a whole at impact/landing.40 The higher the momentum (mass x velocity) prior to/ at impact, the greater the eccentric work required to decelerate the body. As such, intensity of effort and height of landing and/or horizontal speed prior to deceleration are major determinants of peak loading of plyometric tasks.
ii) Strength: greater total lower extremity energy absorption in the sagittal plane has been associated with smaller vertical GRF and greater knee-flexion displacements during landing.44,45
iii) Surface: a compliant surface will deform under load and as such joint loading is influenced by the surface stiffness. Performing plyometrics in water or on sand has been shown to reduce the high impacts and results in less muscle soreness than performing plyometrics on more rigid surfaces.46 For example, at the appropriate depth of water in the pool, there appears to be a reduction of around 45-60% in peak GRFs recorded from plyometric exercise in water versus on land.39,47
iv) GCT: peak force and particularly RFD and rate of power development will also be dictated by GCT. The RFD and rate of power development will be a function of force/power produced divided by the GCT, derived as the reactive strength index. GCT and associated RFD are influenced by task choice but also instructions given for performance of the task (e.g., land and jump leaving the ground as quickly as possible).40 GCT (and associated RFD and neural activation during the task) are important considerations in terms of specificity of training adaptations. Improvements in explosive neuromuscular performance appear to be specific to the GCT,29 with longer GCT (>250-500 ms) suited to acceleration and multidirectional movement performance, whilst linear based (horizontal and vertical) fast (GCT < 200 ms) plyometrics may be better suited for developing linear peak running speeds.
As well as peak external loading, it is also important to consider the relative internal joint loading and associated neuromuscular activation and muscle forces. Internal joint loads should be considered across three planes of motion (sagittal, frontal and transverse). During functional tasks, there is a load sharing across joints and muscle groups.48 The relative ‘torque’ experienced at each joint and subsequent muscle forces will be a product of the resultant GRF and the respective distance away from the joint (torque = force x distance). The specific joint loading will be influenced by task selection,40 and kinematics during the task. For example, altering the trunk alignment during plyometric exercise would alter the center of mass and position it closer or further away from the joint.49 A more upright and stiff posture, described as a quadriceps dominant behavior,50 has been correlated with higher knee-extensor moments.51 Greater hip flexion to knee flexion ratios during plyometric type tasks has been shown to reduce knee-extensor moment and knee energy absorption52,53 and increase hip loading.49 Altered frontal- and transverse-plane knee loading has been shown to contribute to greater ACL loading.54–57 It is recommended to avoid at risk movement biomechanics, specifically a knee dominant motor strategy (e.g., upright trunk positioning) in conjunction with altered frontal (hip and tibial abduction) and transverse plane (tibial rotations and/or internal hip rotation) motions during plyometric tasks, as these will exacerbate knee and ACL loading.54–57
It is also important to consider the relative neuromuscular control challenge/loading, when prescribing plyometric progressions. It is thought that effective use of plyometrics can support improved movement quality and reduce ACL injury risk.31,32,58–60 It is known that strength training does not directly improve movement quality during sport-type movements.61 Instead, there is a need to incorporate more sport type movements to relearn and improve movement coordination during sport-type tasks.62 Plyometric drills can improve neuromuscular control in athletes, which can become a learned skill that transfers to sporting competitive movements,31 aiding in the restoration of sport-specific movement quality after injury. For optimal motor learning (defined as 'the process of an individual’s ability to acquire motor skills with a relatively permanent change in performance as a function of practice or experience),63 it is important that the tasks are performed repeatedly with good movement quality.64,65 Thus, it is important to provide the right challenge to neuromuscular control, with progressive increases in movement complexity, as well as rate and intensity of loading.66
While considering the specific loading of a singular task or repetition is important, as discussed, it is also important to consider the volume of loading. Volume load is the result of many actions during a session or over time (e.g. day/week/month). It is known that high recurrent loading of the ACL can lead to graft creeping and eventually failure.67 Furthermore, issues such as patellofemoral pain syndrome are typically the cumulation of chronic overload68 and common after ACLR.69–71 It is recommended to monitor the cumulative loading of respective tasks, which can be done through documenting the exercise sets/foot contacts alongside the task intensity.
Are they strong enough?
It is well accepted that sufficient strength of the lower limb(s) is important for implementation of plyometrics.72–75 Inability to accept load would mean a greater reliance on joint complexes (tendon, ligament and joint structures) for passive force absorption.43 Considering the various descriptors of load, it would seem appropriate to have an understanding of the patients ability for compound muscle strength, to be able to tolerate the external ground reaction forces. Assessing and tracking closed chain strength (e.g., squat and/or leg press strength) can support optimal task progressions.8,9,76 It is important that the plyometric tasks are aligned to the strength status of the athlete and that task intensity supports and tracks with improvements in strength and functionality. The assessment of closed chain strength (e.g., leg press/squat strength) has been suggested to determine the readiness for the introduction of running on treadmill (e.g., 1.25 times body mass single leg press),9,76 unilateral plyometrics (1.5 times body mass single leg press)8,76 and RTS (2 times body mass single leg press).8,76
Additionally, it is important to understand each joint’s ability to withstand loads. The ankle, knee and hip/trunk must accept and produce force in a load sharing manner,48 depending upon the task and the specific movement quality of the patient. Knee extensor strength is a major barrier to functional progressions after ACLR77 and so understanding the knee extensors strength of the ACLR athlete is important to implement and progress plyometric tasks. Patients will typically display large deficits in knee extensor strength in the early weeks after surgery (e.g., 50% deficits at four weeks post ACLR).78 Restoring knee extensor strength is essential to allow for movement based retraining and implementation of plyometrics.9,79 Assessing knee extensor strength using concentric or isometric assessment of the isokinetic dynamometer or recording knee extension loads used in rehabilitation (eg, 8 or 10 repetition maximum) can provide indication of knee extensor strength to support plyometric implementation and progressions. Knee extensor limb symmetry index (LSI) is often used to support progression through stages of an ACLR rehabilitation pathway.8,9 It can be used to support decision making of when patients are ready to perform certain functional tasks including jogging on the treadmill (LSI, 0.70),9,76,80 single leg landing and jumping drills (LSI, 0.80),8,9,76 RTS training (LSI, 0.90)8,76 and return to high level competitive sport (LSI, 1.0).8,80
Do they move well enough?
As well as aligning plyometric loading to strength, it is also important to align plyometric task complexity to movement capabilities. So, it would appear important to know if an athlete is able to perform the task sufficiently well and safely prior to training prescription. Furthermore, it is important to monitor movement quality during the task. This would aid in ensuring that the athlete performs the task with appropriate kinematics before progressing to a subsequently harder task (either higher loading or greater movement complexity or both).
In assessing and training movement quality it is important to understand what movement quality is and which factors may affect performance.66 Movement quality after ACL injury has been defined as 'the ability to control the limbs and achieve sufficient balance and kinematic alignment during functional activities, not displaying movement asymmetries or risk factors linked to ACL injuries’.8,66 Importantly, the definition makes no reference to what is acceptable loss of balance or deviation of kinematics away from normal, or actually what normal or ideal is.66 In fact, it is thought there likely exists no ‘ideal’ or ‘perfect’ way to move.66 According to the dynamic systems theory,81 there are multiple factors which can influence the expression of movement quality, which should be considered when training and assessing movement quality.66 These can be summarized as a complex interaction between individual (organistic constraints), task constraints and the environment or context in which the task is been performed (environmental constraints).
Despite the ambiguity in assessing movement quality, it is here and elsewhere8,9,76 proposed to utilize a relatively simple qualitative movement analysis method to support progression through tasks and through ACL rehabilitation stages as part of criterion based rehabilitation. This can provide information on movement quality during the tasks at hand, and to be able to provide feedback to the patient, to create a continuous learning environment to solve the task and optimally progress.76 It is suggested to monitor the patient’s ability to maintain control of the body utilizing teaching and training of optimal frontal plane (pelvis, trunk and lower limb, Figure 2a) and sagittal plane control (Figure 2b), depending upon the specific task.76 If the tasks cannot be performed at a minimum task competency, then the tasks should be simplified.8 Qualitatively assessing movement quality (frontal and sagittal plane) as part of the ACL functional recovery process during foundation, landing, plyometric and sport-specific tasks is also recommended. This can provide some objective guidance to support criterion driven ACL functional recovery.8,9,82
Can they tolerate the level of loading?
A key part of optimal load management is adjusting the training according to the response to exercise. Any functional based progression has to be in line with the biological healing and ability of the joint to withstand the loading demands. Pain and swelling can be used to determine exercise based progressions as these factors will relate to the loading stress experienced by the knee.9,83 Progression to more intense or complex tasks should only be allowed when there is no or minimal pain (e.g., 0-2 on the numeric rating scale)83 or swelling (stroke test) increase in response to previous tasks.83 Pain and/or swelling response would indicate excessive previous loading levels to the knee joint and an adverse reactions, which may then limit optimal adaptation. Furthermore, after unaccustomed exercise, there may be an exercise induced muscle reaction, resulting in delayed onset muscle soreness.84 The degree of muscle reaction depends on many factors including exercise type, duration, intensity and habituation to the exercise.85,86 Tasks that are too strenuous will result in significant muscle reaction, which may take substantial time to recover and may limit the ability to train in the subsequent days. Monitoring the muscle soreness can provide an indication of the muscle specific loading and required recovery time, which can then support subsequent training modifications.
Plyometric progressions after ACLR- A Four-staged program aligned to the rehabilitation pathway after ACLR
For effective design of plyometric programs for the ACLR patient, it is imperative that any such program be aligned to the functional recovery approach and overall goals as a whole. These goals include restoring knee specific factors, neuromuscular function of many muscle groups and types of function (e.g., maximal isolated and functional strength and explosive neuromuscular performance), movement quality and sport-specific fitness.8,9 Although, there is still not an international consensus on ACL rehabilitation, there has been considerable research recently published toward standardizing the ACL rehabilitation journey. Current best practice for ACL rehabilitation appears to involve criterion-based rehabilitation through a series of stages.8,9,87 The functional recovery process can be broadly separated into pre-operative, early, mid and late stage rehabilitation and RTS training.8,9
Below is presented a four-staged plyometric program aligned to the ACL functional recovery process. This considers i) the plyometric tasks and associated intensity and complexity, ii) the required movement quality and strength to perform these tasks and iii) monitoring considerations, specifically daily monitoring (e.g., pain and swelling, soreness rules) but also monitoring as part of criterion-based ACL functional recovery. In general, the program has some rules or themes which include progressions in intensity and specificity of the movements with progressive increases in entry speeds (vertical loading height/ horizontal velocity), a gradual reduction in GCT, progression from bilateral to unilateral tasks and from linear (vertical to horizontal to lateral) to multi-planar tasks. Furthermore, it is recommended to use different surfaces, beginning with more compliant surfaces and progressing to stiffer surfaces (Figure 3).
Progressions through stages and exercises within the stage is based on good quality performance of the tasks, ideally no or only minimal pain (e.g., <2/10 on numeric rating scale)83 and/or swelling of the joint to the specific loading demands83 and continued improvement in lower limb strength. Each stage should be completed in sequence and an athlete cannot perform any task in the stage without meeting the specific stage criteria (Table 2). As it aligns to the rehabilitation process after ACLR, meeting specific criteria as part of criterion based rehabilitation is recommended. The four-stage program compliments and aligns to the authors published ACL functional recovery programs.8,9 These involve comprehensive overviews of the mid-stage,8 late-stage and RTS training stages.9 The plyometric program begins in the mid-stage of rehabilitation (Stage 1), with Stages 2 and 3 aligned to the late-stage and Stage 4 to the RTS training stage.
Stage 1 of the program uses low intensity plyometrics, characterized as bilateral off-set and bilateral asymmetrical, but also with sub-maximal bilateral symmetrical tasks (to support movement re-training). The rise in height of the center of mass above neutral position is typically minimal. GCTs should be long (> 1-2s) and the main theme is to support movement retraining, primarily with a focus to support treadmill gait re-education.9 Estimated GRFs are less than two-times body mass per limb. The program is completed alongside foundation movement re-education, functional strengthening (e.g., squat, deadlift, single leg progressions), bilateral landing tasks and isolated strength training.7 Importantly, during this first stage, which occurs during the mid-stage of rehabilitation after ACLR, the patient will have significant knee extensor strength deficits. Knee extensor weakness is a significant barrier to been able to perform functional tasks.77 Furthermore, significant strength deficits result in biomechanical compensatory strategies. This may include compensatory use of the hip extensors instead of the knee extensors during unilateral tasks or compensatory loading of the un-injured limb during bilateral tasks.88–90 Even when achieving the optimal kinematics (e.g. correcting the compensatory movement pattern of greater hip to knee flexion), there is still typically inhibition of the quadriceps, resulting in lower neuromuscular recruitment, which may result in insufficient stimulus for adaptation.89 As such, the benefits of plyometric training for strength development is likely minimal in this stage. It is essential to ensure optimal technique during the movements,64,65 ideally using real-time biofeedback,64 to support appropriate motor learning. Poor task selection may result in movement compensations,49,64 which could interfere with optimal motor repatterning.65 Thus, quality over quantity and intensity is recommended. It is essential to focus on isolated strengthening techniques to overcome the quadriceps weakness and restore normal quadriceps strength during this stage.7 In terms of recommended plyometric tasks for this stage, these can be seen in figures 4 to 6 and within Table 2.
Stage 2 of the program commences when the athlete can achieve the necessary late-stage rehabilitation criteria (Table 2). This means they must have a good single leg squat (defined as good control of the movement with no presence of excessive dynamic knee valgus, altered motor strategy or trunk and pelvis deviations),8 sufficient closed kinetic chain (single leg loads > 1.25 times body mass) and knee extensor limb symmetric index (>80%, LSI) and able to run on the treadmill with good kinematics.8,9 Key themes of late-stage ACL rehabilitation are developing single limb eccentric control (deceleration/landing) and restoring power and maximal eccentric strength.9 However, there is a strong use of bilateral plyometric tasks for developing explosive lower limb strength and high load mechanics. The stage now allows for maximal effort bilateral plyometrics for automatization of the motor pattern, but more specifically for improving kinetics in explosive movement tasks. Consideration though of landing height is needed. A key aim of the stage is to achieve a good bilateral drop jump (kinetics and kinematics) (30 cm) and single leg landing/deceleration control. Example tasks can be seen in Figures 7 to 10 and within Table 2.
Stage 3 transitions to a greater use of unilateral plyometrics and is performed in conjunction with a multi-directional on-field coordination program (pre-planned coordination tasks). It transitions from forward and vertical unilateral plyometric to lateral and then multidirectional unilateral plyometric tasks. The key aim by the end of the stage is to have good kinematics during high speed change of direction and good single leg drop jump and hop performance (multiplanar). Ideally movement quality would be confirmed using qualitative analysis of sagittal and frontal plane kinematics, using high speed (e.g., 240Hz) camera systems.9,66 Unilateral plyometrics play a key role in supporting movement progressions and unilateral control, whilst bilateral plyometrics are used to support enhancements in neuromuscular function (strength, power and RFD) in this stage. Key aspects of the unilateral exercises are to support enhanced motor control with gradually reducing GCT to mimic sport-type tasks (e.g., progressing from 1-2 s GCT to 0.25-0.4 s GCT). Example tasks can be seen in figures 11 to 14 and within Table 2.
Stage 4 builds on Stage 3 and focuses on the use of maximal unilateral plyometric tasks for motor pattern automatization as well as enhancement in neuromuscular performance. Furthermore, in terms of motor patterning, a key aim of the stage as a whole is to progress to re-active movements and prepare for sport-specific training (Table 2). Creating perturbations during plyometric tasks to challenge neuromuscular control is recommended (Figure 15). A key aim of the stage is to achieve good re-active movement performance under sporting type tasks to prepare for sport-specific practice. To RTS, it is recommended to possess good movement quality during sport-type tasks and under sport-specific situations.8 It is recommended to visually assess and use video recordings of sport-specific movements (e.g., reactive cutting or change of direction at an obstacle) during on-field sessions and/or specific field based assessments.66 Patients should also have completed an on-field rehabilitation process,91 corrected muscle strength imbalances8,12,80 and restored their physical fitness.9 This of course is typically after medical clearance from sports medicine physician and/or surgeon has been allowed.8
SUMMARY
This clinical commentary presents a four-stage plyometric program for the ACLR athlete, which can be undertaken as part of criterion-based rehabilitation. Plyometric training should form a key component of the functional recovery process after ACLR. Used effectively, plyometrics can support enhancements in strength, movement quality, explosive neuromuscular function and athletic performance.27–30,33,34,59,60 Plyometric intensity is based on the intensity of efforts, the vertical and or horizontal momentums/velocities prior to impact, the ability of the neuromuscular system to accept those loads, the GCT, the surface compliance/environment (e.g., land or pool) and movement quality during the task. It is important to align the plyometric program to the overall ACL functional recovery program and overall functional recovery status of the athlete. There should be a gradual increase in task intensity and specificity and all tasks should be used for neuromuscular and/or motor control re-conditioning.
Conflict of interest
The authors report no conflict of interests relevant to the content of this review.
_bilateral_off-set_(alternating_box_jump)__b)_bilateral_asymm.jpg)


_and_then_deceler.jpg)
_with_controlled_landing_with_a_foc.jpg)



_and_immediately_jumps_again_(b)_rai.jpg)
_with_controlled_landing_and_stabilization_(b).jpg)

_with_landing_(b)_and_immediate_jump_back_to_th.jpg)


_a_rope_and_b)_medicine_ball_to_create_perturbation_and_.jpg)
_bilateral_off-set_(alternating_box_jump)__b)_bilateral_asymm.jpg)


_and_then_deceler.jpg)
_with_controlled_landing_with_a_foc.jpg)


_and_immediately_jumps_again_(b)_rai.jpg)
_with_controlled_landing_and_stabilization_(b).jpg)

_with_landing_(b)_and_immediate_jump_back_to_th.jpg)


_a_rope_and_b)_medicine_ball_to_create_perturbation_and_.jpg)