The Problem
The Anterior Cruciate Ligament (ACL) is an important stabilizing structure in the knee for individuals that wish to perform regular cutting activity. ACL injury rates vary among different populations, but there are an estimated 200,000 ACL injuries annually with 75% of those undergoing reconstruction within the first year.1,2 Further complicating the assessment of the overall cost of ACL injury is the high rate of re-injury that occurs after an individual has returned to their desired level of activity, with estimates on average at 20%3 across all populations and as high as 29% in a young, active population.4 These data tend to come from larger studies with heterogeneous populations, making it difficult for clinicians to apply the information to a specific patient. Insurance limitations can place a burden on clinicians by limiting them to a small number of visits over an almost year-long recovery process. Even when clinicians do have regular contact with the patients, the heterogeneity of physical therapy interventions across clinicians creates further confusion within outcome data.
ACL rehabilitation is not a new phenomenon, with the first published cases coming at the turn of the 20th century.5,6 Despite thorough research conducted over the last fifty years, several variables remain at play that make it difficult to determine best practice for both surgical and rehabilitation techniques. Graft selection, patient compliance, and insurance limitations are just some of the confounding variables that relate to the success of a primary ACL reconstruction (ACLR). As the understanding of biomechanics, tissue healing timelines, and neuromuscular control mechanisms has improved, so too have the rehabilitation protocols. Over the last decade there have been several attempts to identify the underlying causes behind high re-injury rates, and each piece of research evidence adds to the depth of clinical understanding of the problem.
Return to sport testing is one of the efforts made to decrease the risk for secondary injuries following an ACL rupture, but there is still considerable debate on what comprises the best battery of tests. Clinicians typically utilize a combination of strength testing, hop testing, and patient-reported outcome measures to inform a return to sport decision, but Losciale et al. recently published a systematic review that demonstrated the lack of a significant association between passing these tests and a second injury.7 There is evidence to support the use of several different components within a return to sport cluster, but there is no consensus in the evidence on which combination of components to utilize.7 Several authors have examined quadriceps strength between limbs and found persistent asymmetries after ACLR.8–11 The uninjured leg gets weaker in the post-operative phase, however, and using it as a comparative standard could lead to an overestimation of individuals’ symmetry and knee function. Normative values compared to bodyweight may therefore be a better measure.8,12 Another promising component of the return to sport cluster is psychological readiness following injury. Factors such as not trusting the knee or fear of new injury contribute to poor outcomes following ACLR,13,14 and outcomes assessing emotions, confidence, and risk appraisal have shown predictive ability to determine likelihood of return to sport.15–17
In addition to modifiable factors like strength and psychological readiness, other factors have also been studied. Time has been shown to be an especially important consideration. When return to sport is delayed from six to nine months, the re-injury rate can be reduced by more than 50% for each month of delay.11 Beischer et al. recently found that young athletes who return to sport before nine months have a re-injury rate seven times that of their counterparts who delay return to after nine months.18 There are many possible explanations for why time is an important component; however, it likely is a factor of an increased opportunity to build strength and gain confidence.
The problem with looking at any single variable is that it inherently leads to a linear model for explaining injury risk by taking that variable and drawing a conclusion directly from it. Bittencourt et al. suggest that a complex systems approach is more appropriate for injury prediction because of its reliance on probability rather than direct causality.19 The authors discussed the importance of recognizing that relationships exist among many different determinants, and that the interplay of those relationships is constantly changing based on how the variables interact with each other. Ultimately, a pattern will emerge from the determinants, and that, too, will provide recursive feedback into the system, which will continue to react and adapt to the changing environment. When taking the complex systems model into consideration, the fact that psychological variables, isolated quadriceps strength, and time from surgery can all be components in re-injury risk starts to become clearer.
Time from injury seems to have the most promise for reducing injury risk, but by itself time is a confounding variable in this sense. There needs to be a better explanation for why time from injury matters. One likely explanation for the importance of time from injury is the concept of variability of movement. Traditional views on variability of movement have suggested that there was “one correct movement pattern” and that any alterations from that should be adjusted. Dynamical systems theory suggests, however, that variability is inherent in human movement, and both necessary and ideal for normal function.20 Expert-level performance in several different athletic events, for instance, has been shown to have high levels of variability within the body part, leading to low variability for output and very consistent outcomes.20 Bartlett et al. believe that the variety of potential movement patterns is important because of the flexibility it provides to account for unanticipated changes in the environment.20 Several authors have demonstrated that when attending to a ball during a cutting task, subjects exhibit changes in knee, hip and trunk biomechanics.21,22 Regardless of the implications that these findings have on injury risk, it certainly suggests that there is not one single way that patients will move to perform a cutting maneuver, and that attentional resources play a role in movement performance. Training variable movements in a variety of settings is imperative to safely prepare a patient for return to a dynamic environment. Harbourne et al. advanced the dynamic systems approach by providing guidelines for physical therapists to use to promote motor learning utilizing movement variability.23 By increasing task and environmental complexity, the patient can practice and ultimately can learn how their efforts create an effect on their surroundings. Initial performance will be erratically variable and poor as they attempt to acquire control over the novel skill. That performance will transition to relatively low variability as they focus on their efforts and demonstrate improvements. Finally, they will transition to a consistent level of variability as the patient’s skill can be translated to increasingly complex situations. Does time as a decision factor merely allow for the higher likelihood that the patient transitions out of that middle phase and into the advanced phase? If time is truly just allowing the patient to learn more movement strategies and increase their variability, is there some way to accelerate that process? Current ACL rehabilitation methods fail to efficiently address movement variability, movement pattern acquisition, and long-term motor pattern retention. The purpose of this clinical commentary is to describe the Neuroplastic Adaptation Trident Model and provide examples for clinical implementation.
The Solution
In order to best understand rehabilitation and return to play considerations, one must first understand the pathological process that occurs as a result of the injury. Surgical management for an ACL tear aims to correct the biomechanical function of the ligament, but it is unable to address the neurosensory component. The ACL contains afferent nerve fibers connecting via the articular branch of the posterior tibial nerve.24 Those nerve fibers are primarily located near the femoral attachment of the ligament and provide important joint position sense through Pacinian, Ruffinian and Golgi-like mechanoreceptors.24 Without the mechanoreceptors a noticeable gap develops in the afferent information regarding joint position and movement that the brain receives. In addition to the lost afferent feedback, the reflexive muscular splinting mechanism that comes with ACL quick stretch is also lost.25 After ACL rupture, when the connection to the articular branch of the posterior tibial nerve has been lost, the brain enters a neuroplastic state in order to compensate for the loss. Neuroplasticity is a state of cortical adaptability and refers to the broad idea that the brain can adapt and change based on internal and external stimuli. Some of the potential mechanisms include synaptogenesis, neurogenesis and neurochemical changes, although specifics remain the subject of considerable debate.26 It is generally accepted that the brain is a plastic organ and, when input changes occur, the brain will adapt to those changes.
Functional magnetic resonance imaging (fMRI) studies conducted on individuals following ACL reconstruction demonstrate changes in cortical and cerebellar activation patterns.27,28 Specifically, increased activation in the primary motor cortex, secondary somatosensory area, and lingual gyrus suggests that ACL injury and subsequent recovery change how the brain functions.27 Additionally, decreased activation in the cerebellum suggests a loss of automaticity in movement and an increased need for attentional awareness.27 In addition to those changes in activation, Zarzycki et al. measured resting motor thresholds (RMT) of the motor cortex using transcranial magnetic stimulation (TMS) and demonstrated decreased corticospinal excitability as soon as two weeks following ACL reconstruction.29,30 To date there have been no intervention-specific studies looking at the effect that rehabilitation can have on this parameter, but multiple studies have shown that corticospinal excitability changes occur after ACL reconstruction, and that they persist for years.31–34 This breadth of research supports the postulation of Kapreli et al. that ACL injuries cause dynamic changes to the central nervous system, and that these injuries should be considered “neurophysiologic dysfunction, not a simple peripheral musculoskeletal injury”.28 The brain clearly enters a neuroplastic state following ACL injury, but neuroplasticity is not inherently goal-oriented or directional. Plasticity changes can be influenced by behavior and rehabilitation methods, or a lack thereof. Grooms et al. proposed that an increased reliance on visual feedback and internal locus of control during rehabilitation could potentially explain negative changes that occur after injury.35
In order to best understand rehabilitation goals for sensory interaction, it is important to first examine a normal state. Extensive research and modeling has been completed on the process by which the central nervous system processes and utilizes sensory input to maintain static balance, known as sensory reweighting.36,37 Peterka describes a closed feedback loop system, where information from the proprioceptive, visual, and vestibular systems are dynamically interpreted, weighted, and acted upon, with the resulting system output being fed back in as a new systemic input.38 The brain adjusts, or reweights, the relative contribution of each of the sensory systems based on the demands of the environment. In a relatively stable environment, where changes to the visual and proprioceptive system are occurring slowly, around .5 deg/sec, the brain relies heavily on the proprioceptive (50% relative contribution) and visual (33%) systems, with relatively minor influence from the vestibular system (17%).38 However, when the dynamic changes to the environment increase, as is expected in athletic participation, to a faster speed, 8 deg/sec, the brain reweights the relative contributions to rely almost exclusively on the vestibular system (82% relative contribution) with the proprioceptive (15%) and visual (3%) systems developing a diminished role.38 Although there may be limited validity in extrapolating from this data to a chaotic athletic environment, understanding how the brain reweights sensory contributions to balance is very important for rehabilitation purposes.
In an attempt to maximize the neuroplastic state of the brain and contribute to positive changes, clinicians need to take into account the principles of motor control and motor learning. Motor learning is the process of acquiring or altering motor skills to create a permanent change in performance.39 There are several different models that have been developed to explain motor learning, but they include common factors or variables such as feedback, cueing, focus of attention, rehearsal schedule, contextual interference, task relevance, and amount of practice. Fitts and Posner developed a model of motor learning based on a continuum of cognitive, associative, and autonomous stages.40 In the cognitive stage the patient must develop an awareness of the desired task and how to control the movement. They will transition to the associative phase when they begin to utilize the trained movement pattern in other tasks or environments to which they devote attentional resources. Ultimately, the patient needs to transition to the autonomous stage, where they unconsciously select that movement pattern during the appropriate tasks. An individual’s relative stage of learning dictates what other factors can be utilized to influence motor learning. For example, if the individual is in the cognitive stage of learning, a clinician may only be able to alter one variable at a time, (e.g. practice schedule), whereas an individual in the autonomous stage may need to have multiple variables altered at a single time (e.g. contextual interference, feedback, and attentional focus). To best address the various stages of learning, a clinician must have strong understanding of the various tools or strategies available to influence motor learning.
An easy starting point for motor learning discussion is the use of rehearsal schedule, which can be divided into blocked, serial, or random practice. Blocked practice utilizes high repetitions of a single task and should be dedicated to novel movements or movements with high complexity. It leads to improved performance quicker than other rehearsal schedules, but it displays limited retention of the specific skill. Serial practice incorporates several tasks in a repeated pattern and should be utilized as the individual progresses into the associative stage of motor learning. To maximize retention and transition to the autonomous stage, random practice, or, multiple movements performed in an undetermined order, is necessary. Random rehearsal will result in an initial decrease in performance, but an increased ability for the individual to perform the skill at a later point in time.41 Randomized rehearsal is superior to blocked practice in terms of retention of a specific motor skill due to contextual interference.41
Gokeler et al. outlined the principles of motor learning as they can be utilized for ACL rehabilitation, and identified four key concepts to consider: external focus of attention, implicit learning, differential learning, and self-controlled learning and contextual interference.42 Internal focus is when one’s attention is on the movement of a body part, whereas external focus directs the individual’s attention to the effects of the movement on an interaction with the environment.43 Providing an external focus of attention accelerates the learning process, and a higher level of skill is achieved sooner due to the utilization of unconscious processes.44,45 In coordination with external focus of attention is the use of implicit learning, which emphasizes cueing related to how the movement feels, rather than a specific set of instructions. Implicit cues like “land softly” or “explode off the ground” assist in developing anticipatory skills and decrease the cost of attentional resources needed to complete a task.42
Differential learning takes the concept of rehearsal schedule and incorporates variability of movement skills. Differential learning relates to the dynamical systems approach discussed by Bartlett et al. by randomizing the performance of several tasks that all address the same general movement pattern.20 Contextual interference bridges a gap between cognition and skill acquisition in which interference by cognitive or physical means leads to higher levels of learning and retention of a specific skill, despite an initial decrease of performance.41,46 By shifting attentional resources to a secondary focus, the individual learns to execute the primary task automatically, instead of with conscious control. Initially the decreased ability to focus cognitive resources on the task will hinder performance, but as the brain adapts to the new challenges and inputs, it will develop new movement strategies and increase the variability of available movement patterns. Self-controlled learning is an important motivation tool to keep the individual committed to the rehabilitation process. Patients who are in control of the situation, even in simple ways, are more likely to become invested in the process.
Wulf et al. dove deeper into the concepts of motivation and attention in developing the OPTIMAL theory of motor learning.44 OPTIMAL is an acronym for Optimizing Performance through Intrinsic Motivation and Attention for Learning, and the authors emphasize self-efficacy and control. According to the OPTIMAL theory of learning, an individual with no autonomy and low expectations will inherently have a more internal focus and decreased performance. That decreased performance will feed back into the system, further decreasing expectancy for performance and harming future attempts. However, an individual who has higher autonomy and enhanced expectations will focus more externally on the task, leading to improved motor performance.44
The theoretical frameworks developed by Gokeler et al. and Wulf et al. are excellent resources to work from but fall short of providing a practical structure to rehabilitation. One consideration that is noticeably absent is dosage volume. In orthopedic injury, research assessing adequate dosage for motor learning is sparse, but stroke research suggests that larger amounts of repetitions result in better outcomes.47 The physical act of a repetition is only part of the process of motor learning, however, and the cognitive processes of problem solving and movement selection also need to be considered.48 When learning new motor patterns, individuals should not simply repeat the result of a solution over and over (blocked practice), but rather should practice the act of problem solving.49 Individual variability for movement pattern acquisition mandates that optimal dosing will not likely be a single value for each patient, but needs to be individualized.47
Another prominent motor learning method for neurophysiologic dysfunction is constraint-induced movement therapy (CIMT), developed by Taub et al.50 CIMT was designed to treat functional loss as a result of stroke, but it is based on the concept of neuroplasticity. The main principles of CIMT are repetitive, task-oriented training for several hours a day, a transfer package to employ new skills from the clinic into the real world, and constraining the patient to utilize the affected body part.51 Major takeaways from this model are the concept of the transfer package and the regular utilization of the new skills in real-life situations.
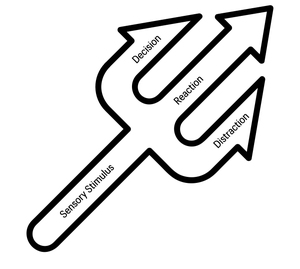
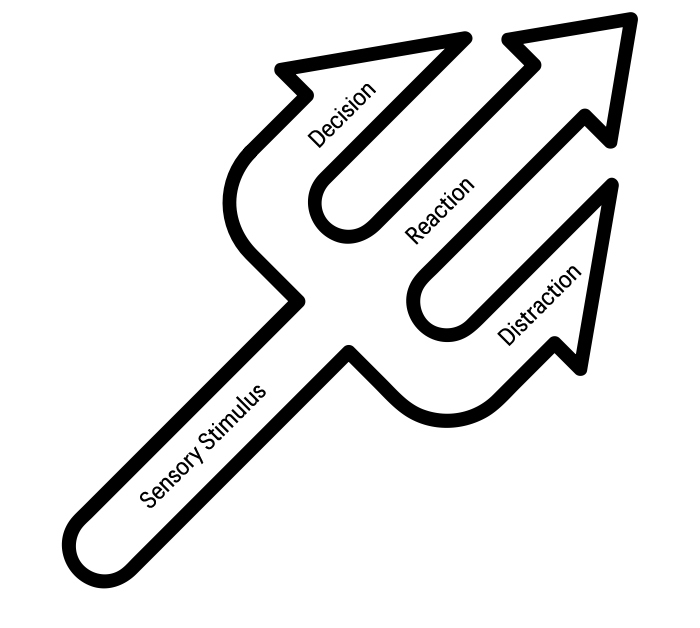
The combination of these models and systems led to the development of a novel framework for structuring the prescription of exercises to maximize positive neuroplastic adaptations following ACL reconstruction. The primary goals for the model are to accelerate the motor learning process in order to maximize movement variability and prepare athletes for safe return to a chaotic athletic environment. This framework (outlined below) demonstrates utilization of a staged approach to ACL rehabilitation. The Neuroplastic Adaptation Trident Model is a treatment framework developed to practically implement motor learning principles into orthopedic rehabilitation. It is based on a “trident” of neuroplastic exercise in which the base of the trident represents sensory stimulus, and each prong represents decision-, reaction-, and distraction-based tasks, respectively. Complexity of tasks can be increased by incorporation of one or multiple prongs of the trident (Figure 1).
Sensory stimulus is the base-level component that clinicians need to consider in all interventions to maximize sensory re-weighting during exercise. Rapidly changing environments require more vestibular and proprioceptive input, and so rehabilitation methods should minimize reliance on the visual system. There are two methods to challenge sensory stimulus, through isolation (targeting a single system) or combination (targeting two systems simultaneously). In order to train the sensory systems, a clinician can control information in three ways: decreased input, absent input, and incorrect input. Clinicians can choose to challenge each of the sensory systems in a variety of ways, in order to decrease reliance on that particular system during the tasks (Table 1).
The somatosensory system is challenged with decreased or incorrect input through changing the surface-to-limb interface, or by changing body position for the task. The visual system is the easiest to manipulate and can be challenged in any of the three methods mentioned. Clinicians can decrease visual input through the use of stroboscopic glasses or pinhole glasses, forcing the brain to de-prioritize the visual input it is receiving. Additionally, visual input can be removed by closing or blocking the eyes. And finally, the clinician can provide incorrect visual information through the use of virtual reality (VR) goggles. This technique forces the patient to continue utilizing their visual system, but only for cognitive tasks and not for relevant balance information. The vestibular system is challenged by dynamically changing the head and eye position and movements. By isolating and combining the sensory systems clinicians can address differential learning and contextual interference to maximize motor learning, as well as induce constraints on the systems being utilized to isolate deficits. The therapist may choose not to manipulate sensory stimuli during an intervention, but it should always be the first consideration due to the known importance of decreasing reliance on visual information. See Table 2 for examples.
The first prong of the trident builds upon the foundation of sensory stimulus considerations and adds complexity. Any rehabilitation exercise can be considered a primary task, and decision-based tasks are defined as altering a primary task based on an external cue. Decision-based tasks introduce randomization into task performance and emphasize the process of problem solving as an exercise itself (Table 3).
The first component is the number of options available. A simple task involves an either/or option that includes an option of left vs right or even “go” vs “stop”. More complex tasks will include multiple options and a variety of tasks. Additionally, clinicians can increase complexity by changing the mode of stimulus for the cue. Simple cues can be auditory or visual with a direct connection between the cue and the tasks, so that the patient can respond without additional cognitive processing. Complex cues can also be auditory or visual, but they are arbitrary and not related directly to the tasks. Colors or random words/numbers are utilized, and the patient must add a cognitive processing component to determine what particular task the cue correlates to. The clinician will need to decide whether to cue before the movement in order to simply randomize the task, or cue after the task has been initiated to challenge real-time problem-solving ability. Decision-based tasks emphasize external focus and implicit learning as the patient interacts with their environment. The randomization of practice facilitates improved problem solving, and picking appropriate tasks will force the patient to utilize the affected body part. Table 4 provides examples.
As the patient becomes more proficient in the primary skill, the clinician needs methods to challenge the performance of that movement with secondary tasks. The second prong of the trident is reaction-based tasks, which are secondary tasks that a patient must complete while still performing the primary movement (Table 5).
The addition of a new challenge will decrease the attentional resources available for the primary task and force the patient to interact with a stimulus in their environment. Reaction tasks are either perturbation based, where the clinician provides a stimulus to body position, or motor skill based, where the patient must complete a hand/eye skill. Simple perturbation reaction tasks are typically uniplanar with a single known push or pull stimulus. Complex perturbation reaction tasks can become multiplanar and incorporate the addition of unknown stimuli (Table 6).
Simple motor skill reaction tasks include a secondary task with a known outcome, such as catching a ball. Complex motor skill reaction tasks incorporate a decision-based component into the secondary task, requiring the patient to process information and change performance of the secondary task based on the environment (Table 7).
Reaction-based tasks continue to build on an external focus of control and add contextual interference through randomizing practice. Like decision-based tasks, reaction tasks force the patient to practice problem solving and lead to an acquisition of more motor patterns, contributing to greater movement variability.
The final prong of the Trident builds on complexity by utilizing cognitive resources to complete an additional challenge and/or tertiary task. Distraction-based tasks increase the cognitive load for something that is unrelated to the primary tasks and can be accomplished by utilizing the principles of decision and reaction-based tasks (Table 8).
Simple distraction tasks utilize a primary motor task that the patient is working to develop and incorporate a secondary task that changes the attentional focus. This can include questions based on semantic knowledge and progress to questions based on problem solving. Complex distraction tasks will include a reaction and/or distraction secondary task and incorporate a tertiary level component to the exercise. Distraction-based tasks have a strong emphasis in contextual interference and external focus of control. They challenge the problem-solving process, and utilize attentional resources, increasing the automaticity and autonomy for the primary task. Table 9 provides examples.
There are several considerations regarding dosing that need to be addressed. The first consideration is deciding when to implement neuroplastic interventions and how often they should be utilized. Based on the CIMT research, our model recommends implementing sensory stimuli and decision-based tasks immediately as part of the rehabilitation process. These methods should be utilized repetitively throughout the day as part of the home exercise program, and it is imperative that clinicians target the transfer package through patient education on incorporating these daily movement skills. There are simple phone applications that can create a random yes/no stimulus that patients can use for either/or decision-based tasks. Not only can the patient change sensory input through foot placement on a pillow/blanket/towel, eyes open vs closed states, and head turns horizontal or vertical, but they can at least introduce a serial practice schedule by cycling through different combinations of those states during exercises like weight shifts, squats, lunges, etc. Stroke research on neurophysiological dysfunction tends to recommend high dosage for motor learning, but there is no clear consensus on exactly what that volume should be; additionally, there are recommendations to individualize dosing.52 Hauptmann et al. found that for healthy individuals, improvement between sessions for a motor task was based on their proximity to saturation, defined as a plateau in performance that is individually-determined.53 With these findings in mind, the authors recommend that the majority of a rehabilitation session be conducted using this framework, but that each exercise be assessed individually for qualitative saturation. The important thing for the clinician to watch for is a plateau in performance, which will not necessarily come at ideal performance within the session. If the patient completes 5-10 repetitions consecutively without any improvement in performance, the clinician should move on to a new task. Based on the authors’ experience, patients tend to demonstrate improvement with at least one in-person session per week, as long as the patient is motivated and committed to continuing to practice these principles as part of a home exercise program. Additionally, autonomy of the patient must be considered in order to enhance motivation. The patient should be an active participant in selecting exercises and given options to choose from throughout the session.
STAGE 1
The primary goals during the acute phase of rehab are managing joint effusion, restoring full knee joint range of motion (ROM), and facilitating active quadriceps contraction. It is important for the clinician to find ways to transfer these principles to the home exercise program for repeated practice. While the patient performs quadriceps setting exercises with neuro-muscular electrical stimulation (NMES), they can wear virtual reality (VR) goggles to provide incorrect visual stimuli to decrease or eliminate internal focus on the quadriceps contraction. External cueing should be utilized during this intervention by having the patient “push into the table” or “think about kicking a ball.” Sensory stimulus can also be manipulated during weight bearing and balance interventions by changing footwear, surface, orientation (i.e. double leg vs. tandem stance), or visual input (decreased, absent, incorrect) in isolation.
Decision-based tasks should be initiated to promote random practice early in the rehabilitation process. Simple decision-based tasks can utilize “either/or” options such as weight shifts with visual pointing of left or right, or bodyweight squats with verbal cues of “stop” and “go.” Decision-based tasks are advanced by adding more than two options (i.e. weight shifts to the right, left, or forward with auditory or visual cueing) and by introducing complex cueing. Color cues add complexity by correlating different colors with different directions, forcing the patient to problem solve before executing a task. A simple tool for randomization of color stimuli is the Vector Ball (Eye on Ball Inc., Oviedo, FL), which randomly lights up red, green or blue on impact. To incorporate differential learning into the complex cues, some colors can correlate with a different task altogether, or a change in cueing rules. Other complex cueing methods can include verbal numbers, initially as “either/or,” in which even numbers correspond with weight shifts to the right and odd numbers correspond with weight shifts to the left.
Once the patient displays competence with a variety of cueing options, decision-based tasks should be further progressed with increased complexity of sensory stimulation. Introduction of stroboscopic glasses to decrease visual input and initiation of head turns or eye movements to challenge the vestibular system in isolation are good initial steps. Further advancement includes a combination of interventions to challenge multiple sensory systems while the patient performs decision-based exercises.
Simple reaction-based tasks should also be initiated in this phase, with an easy version of a secondary motor control task, such as catching a ball. These tasks can be performed while performing exercises such as squats, wall sits, or bridges in order to emphasize an external focus of attention on the secondary task. As with decision-based tasks, sensory stimulus can be manipulated during this task to increase complexity once competence is demonstrated.
In addition to decision and reaction tasks, distraction-based tasks should also be incorporated during this phase in order to further challenge attentional resources. Simple, semantic based questions or math problems added during exercises distract the patient from primary and/or secondary task performance. An example of a challenging task would be utilizing the VR goggles and 360-degree interactive pictures taken with an iPhone application. The pictures include nine people wearing various colored jerseys with the numbers 1-9 and standing in various positions. For this intervention, the rehab specialist asks questions of varying difficulty that the patient needs to answer. Simple versions of VR questions include “where is number 5?” or “what color is number 2 wearing?” requiring the patient to scan the visual environment by dynamically moving the head. More complex questions such as “what color is 15 divided by 5?” or “what numbers are not standing?” force more cognitive processing and problem solving. Appendix A provides examples of interventions during this phase.
STAGE 2
Primary emphasis for the post-acute stage of rehabilitation should include motor patterning, light loading, resistance training, and improving the ability to load dynamically. With an emphasis on promoting proper motor patterning and low-intensity resistance training, decision-based tasks can be incorporated to promote randomization. An example of a decision-based intervention is lateral band walks using the Vector Ball for complex cueing to determine which direction the patient should step. Once the patient demonstrates competence, sensory stimulus can be further limited by use of stroboscopic glasses.
Reaction-based tasks are progressed in this stage of rehabilitation to include simple perturbation tasks with a known stimulus to initiate the movement. Lateral lunges with a therapist delivered push or pull perturbation, alters task initiation, promotes differential learning, and increases movement variability. These reaction-based perturbation lunges can be advanced by progressing the perturbations to include both forward and lateral lunges, or by altering the sensory input of the patient. Complex reaction-based tasks are also utilized in this stage. Progressing from the simple reaction-based task used in Stage 1 for single leg balance, the patient can be instructed to catch a ball with the right, left or both hands based on verbal instruction from the therapist. The cueing could be advanced to arbitrary cues by utilizing the number system mentioned above in Stage 1 (i.e. even number for left hand and odd number for right hand) or by bouncing the Vector Ball to the patient with the completion of the secondary task dictated by the color on impact (e.g. red catch right hand, green catch left hand, blue catch with both hands).
A major component of rehabilitation during this phase is the emphasis placed on muscle strength and hypertrophy. The scope of this paper is to focus on neuroplasticity interventions, but for additional resources regarding strengthening parameters the work of Reiman et al. and Welling et al. should be consulted for programming considerations.54,55 It cannot be emphasized strongly enough that strength training is of the utmost importance during rehabilitation and should not be sacrificed.
While the patient is working on developing strength, they must also learn shock absorption and load dissipation to prepare for the demands of linear running. This training must begin at an intensity less than bodyweight until strength capacity is able to meet the demands of jumping and landing. An aquatic environment and a sled-based training system like the MVP Shuttle (Shuttle Systems, Bellingham, WA) are both excellent ways to train impact mechanics with a decreased load. Initially, the patient would perform blocked practice for double-leg jumps, continuous single-leg jumps, and alternating single-leg jumps to develop competence for the desired triple flexion to triple extension movement. The therapist should use external cues such as “soft” or “land on egg shells” to teach the patient to feel how their movement causes an interaction with the environment. Implicit learning can be accomplished by having the patient look straight ahead to discourage visual input of the landing, forcing them to utilize other senses to increase awareness of body position and anticipate landing. In order to transition from blocked or serial practice to random practice, the therapist should incorporate simple decision-based tasks by utilizing verbal cueing of “stop” and “go” as well as “right” or “left” to determine which leg the patient would land on and initiate the next jump. To advance the complexity of decision-based tasks, the therapist can increase the number of options (e.g. “right,” “left,” “both”), utilizing arbitrary cueing (e.g. numbers or colors that correlate which leg to land), and sensory manipulation (e.g. stroboscopic or pinhole glasses, closed eyes, or landing on an Airex pad (Airex, Sins, Switzerland) for a known and unknown landing surface).
Distraction-based tasks will increase contextual interference when completing the primary task. While the patient performs a squat exercise with an emphasis on avoiding a lateral shift, the therapist asks simple questions or poses cognitive tasks (e.g. What is your phone number? What is your jersey number? Spell a certain word, count up from three starting from zero, list as many colors as possible, etc.). To incorporate a tertiary task the patient performs a primary decision-based task of lunging or squatting based on the visual color cue; the patient also completes a secondary task of catching a ball; and the patient is given a tertiary task to answer simple math problems. These complex versions of interventions in which the therapist incorporates elements from all aspects of the Trident should only be utilized when the patient demonstrates competency with the primary and secondary tasks. In the later stages of rehab, further combination of the different prongs of the Trident are introduced. See Appendix A for examples of interventions during this phase.
STAGE 3
The advanced stage of rehabilitation emphasizes the progression of plyometrics and power activities, running and cutting mechanics, and sport/position-specific activities. Athletes should only begin interventions in this stage when they have restored an adequate amount of quadriceps strength to complete bodyweight impact exercises. The progression of plyometric activities proceeds with incorporation of each prong in isolation, followed by a combination of all three prongs to increase complexity of the primary task. It should be acknowledged that the interventions described should be done in addition to traditional high intensity plyometric training. These interventions are designed to challenge movement variability, but traditional plyometric prescription will do a better job of increasing power and explosive muscle qualities.
Body-weight plyometrics are a foundational component during this stage of rehabilitation. By this stage, the patient should be well prepared to handle higher-level manipulation of sensory input with stroboscopic glasses, jumping and landing on an unstable surface (e.g. Airex pad or BOSU ball (Bosu, Ashland, OH)), and altering head movements (e.g. nodding or shaking head while executing plyometric task). To incorporate decision-based tasks, the patient, while jumping, is provided a verbal or visual cue to determine which leg to land on and initiate the next jump. To incorporate reaction-based tasks, perturbations can be included initially as a known stimulus then progressed to unknown stimuli. Additionally, motor tasks such as catching a Vector Ball based on the color emitted while landing from the jump can be utilized. Lastly, in order to incorporate distraction-based tasks, inclusion of cognitive tasks (same list in Stage 2) should be utilized while the patient performs plyometric activities.
When prescribing exercise, the therapist should continuously be considering the base of the trident, sensory stimuli and how to integrate a single prong of the trident with sensory manipulation. First, the therapist should incorporate a decision-, reaction-, or distraction-based emphasis with a single form of sensory manipulation. This could include a decision-based plyometric to land on a certain leg based on a cue combined with sensory manipulation of landing on an Airex pad. The therapist could also utilize a reaction-based plyometric such as landing from a jump after a perturbation in the air, with the sensory manipulation of closed eyes.
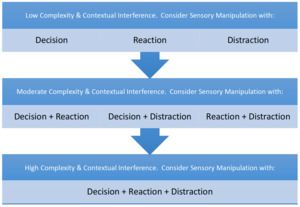
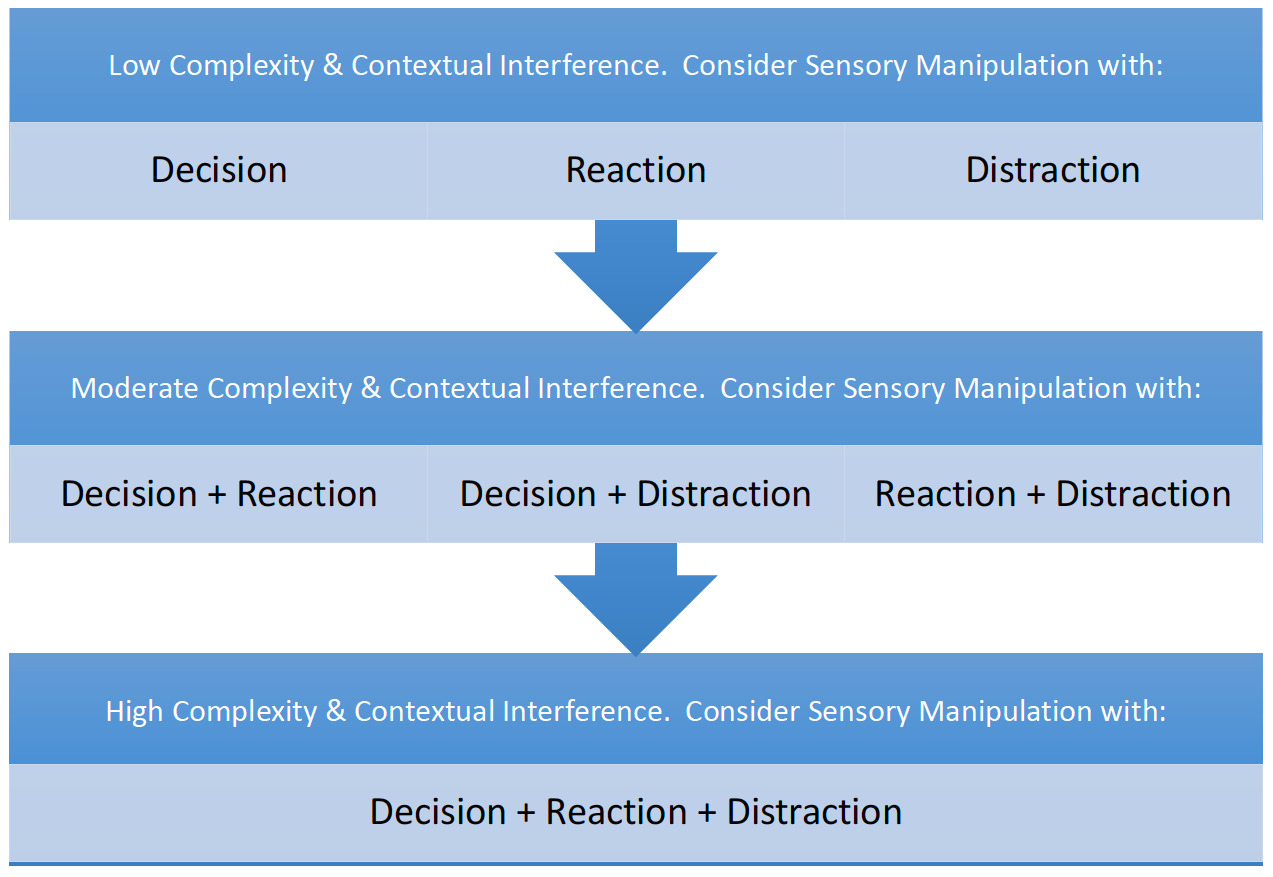
After utilizing a single prong with sensory manipulation, a combination of two or more prongs should be performed (i.e. decision with reaction, decision with distraction, reaction with distraction or all three). These exercises with increasing complexity are designed to mimic the dynamic demands of an athletic environment and to improve movement variability. Decision with reaction tasks can include landing on a specific leg in response to a verbal cue while receiving a known in-air perturbation. A decision with distraction could be the patient performing a 90-degree rotational jumps in response to a visual cue while the patient lists as many prime numbers as possible. A reaction and distraction task could involve the patient performing continuous lateral line hops while catching a Vector Ball with the appropriate hand based on the color emitted and spelling specific words listed by the therapist. As always, the therapist should consider the underlying base of the trident, sensory stimulation, with all tasks. Once the therapist becomes comfortable with the different prongs of the trident and how to manipulate them, exercise selection becomes limitless. Refer to Figure 2 for a progression flow chart of increasing complexity.
Another method to increase difficulty is to utilize the prongs in sequence, either the same prong repeated (e.g. decision-based task followed by another decision-based task) or using different prongs (e.g. decision-based task followed by a reaction-based task). Due to the dynamic nature of sport, with a constantly evolving environment, incorporating sequenced tasks is a necessity. Sequenced decision-based tasks could be as simple as a verbal right or left 45-degree angle change of direction, followed shortly by a second verbal cue. Sequencing a decision-based task into a reaction-based task could involve the patient performing a depth jump followed by a cut in a given direction based on a verbal cue, and then followed by catching a football. See Appendix A for examples of interventions during this phase.
STAGE 4
In order to progress to the final stage before returning to sport, the patient must have developed an adequate amount of strength, power and explosiveness in controlled environments. Emphasis for the return to sport stage of rehabilitation must include high-intensity running and cutting with the addition of open-decision sport and position-specific activities. The key during this stage of rehabilitation, and the main difference between Stage 3 and Stage 4, is the attempt to emulate the demands of the sport as closely as possible. This should include a continuation of the components of the trident with increasing difficulty for preparation for the chaotic environment of competition. See Appendix A for examples of interventions during this phase.
Discussion
ACL injuries are a common phenomenon and continue to remain prevalent, and clinicians and researchers are continuously searching for the best way to decide when a patient is appropriate to return to activity. Quadriceps strength has shown promise as a valuable return to play criterion, and the logical explanation that asymmetrical strength can lead to compensations makes sense. Human movement is a complex and dynamic system, and variability of movement provides an individual with redundant strategies to execute desired tasks. Strength is important, but isolated strengthening fails to account for the motor learning that must take place after a neurophysiologic injury.
Psychological parameters and specifically the concepts of emotion about the injury, fear of re-injury, and risk assessment are also important considerations for a return to sport activity. Patients who are apprehensive about activity are likely to shift attentional resources to task execution and away from interacting with the environment, which can increase injury risk in a crowded athletic field that is constantly changing. Like human movement, the human psyche is exceedingly complex, and many factors contribute to the confidence that goes into effective athletic competition. In the absence of the physical parameters required to execute desired tasks, excessive confidence can be just as problematic as insufficient confidence. As with strength, psychological readiness is an important factor in return to play, but it needs to be included in a cluster of several factors that comprise a complex system view of injury risk. As strength increases and movement patterns become more complex and variable, it follows that psychological readiness should improve, but in the cases where it does not, further intervention may be necessary.
Delaying return to sports timelines has repeatedly demonstrated a decrease in the risk for re-injury. The parsimonious explanation for this suggests that time allows for a better return of strength and an improved psychological readiness. Functional return to sport tests successfully assess the movement variability that occurs during this delay, but testing specific tasks (e.g. single leg hop, triple hop, etc.) does not measure the patient’s ability to respond to a changing environment using different motor strategies. Further time from injury provides the opportunity to add more motor strategies and more experiences into the complex system of injury risk. A key component of time from injury is the acquisition of motor strategies to increase the amount of movement variability, and rehab should focus on accelerating that process.
Neuroplasticity, or the ability for the brain to adapt and change, is a burgeoning field with several known parameters on how to affect motor control and motor learning. The loss of mechanoreceptor input from the native ACL and traditional rehabilitation methods have combined to show changes in motor cortex activation and sensory processing within the brain. It is the author’s preference to manipulate visual input initially due to the high reliance on vision following injury, but any sensory manipulation provides neuroplastic stimulation. If rehabilitation specialists acknowledge neurophysiological dysfunction, and implement the known parameters to affect positive neuroplastic changes, the logic follows that outcomes will improve. Regardless of improvement, this procedure will further the understanding of best rehabilitation practices for a common yet complicated injury.
There are limitations in what the current evidence support. First, the majority of motor learning research, particularly in regard to dosage has been conducted on individuals after a stroke. While it is accepted that an ACL tear results in neurophysiological dysfunction, there may be something about the magnitude of changes in the brain after a stroke that impacts rate of learning. Further studies should be conducted on ACL-injured patients specifically to identify adequate dosage for retention of movement pattern changes. The second limitation is that while fMRI and TMS studies have shown neural changes after ACLR, some or all of those changes may be necessary compensatory adaptations to the injury, such as the increased activity of the secondary somatosensory area to accommodate for the decreased volume of afferent information following the loss of mechanoreceptors. Further research should first evaluate the effect that those findings have on injury rates and whether there truly is something that needs an intervention. Researchers should then study the Trident Model, or at least components of it, and elucidate how these interventions impact fMRI and TMS measures. The most important future for rehabilitation is for surrogate clinic-based tests that therapists can utilize practically, rather than depend on fMRI and TMS. VR technology has a lot of promise as a method to challenge cognitive processing and vestibular function. The addition of force plates to assess loading and response to perturbation should also be explored.
The Trident Model serves as a framework compiling current best evidence into a practical system for rehabilitation specialists and researchers to address a missing component in ACL rehabilitation. One of the strengths of the Trident Model is the deep-rooted basis in well-established and understood concepts. Built upon the basic science of neuroanatomy and instituted through the incorporation of strength and conditioning principles along with the inclusion of OPTIMAL theory and other methods of motor learning, this model includes a current best understanding of how to address these impairments. Equally as important, the model takes complex concepts and creates a practical framework that clinicians can adapt in practice. Further, by outlining the concepts and general dosage recommendations, this model provides researchers with something that can be objectively studied in randomized controlled trials.
Conflicts of Interest
The authors have no conflicts of interest to disclose.