Background and Purpose
American football generates the most sports-related injuries in the United States, with tackling as the leading injury mechanism.1 Overall injury rate at the collegiate level has been reported as 8.61 per 1,000 athlete exposures (AEs) – twice the rate of high school levels;1 competition injury rates are reported as high as 36.94/1000 AEs.2 These injuries can be difficult to manage secondary to potential uncommon diagnoses, multiple concurrent diagnoses, and the paucity of literature describing management, especially regarding later phases of rehabilitation and return to sport criteria.
Traumatic hip dislocation is an uncommon injury typically arising from high-energy axial impact.3,4 The most common cause is motor vehicle accident accounting for between 70-84% of such injuries,4,5 followed by falls,4 with only 2-5.5% occurring during sports activities.5 Posterior dislocations have been reported to represent 85-92% of these injuries,3,5 generally occurring with the hip in a flexed and adducted position.4 Associated local compounding injuries may include acetabular, femoral, or pelvic fractures, femoral head cartilage damage, vascular or ligamentous injury, soft-tissue disruption, and neural involvement,3–6 all of which may negatively impact prognosis. Sequelae of posterior dislocations of particular concern are avascular necrosis (AVN) and post-traumatic arthritis, which have reported incidences as high as 40% and 55%, respectively. Higher rates are associated with increased severity of injury and delayed joint reduction (over 12 hours from injury).6,7
Multiple classification systems exist for posterior hip dislocation. Two common systems are the Thompson-Epstein and Milford and Stewart classifications, based on radiologic and functional stability findings respectively (Appendix).4
Upon suspected hip dislocation, acquisition of anterior to posterior radiographic plain films is indicated to confirm the diagnosis.4,8,9 Some debate exists on whether oblique or Judet films are routine, however they help elucidate the presence of a posterior acetabular wall fracture which is the most common acetabular fracture in posterior dislocations.8,9
In the absence of femoral neck and acetabular fractures, closed reduction is immediately indicated.3,8 If closed reduction is not possible, then open reduction is indicated.3 Following relocation, confirmatory repeat radiographs should be performed in conjunction with computed tomography to assess for femoral head integrity and intra-articular loose bodies.8–10 Magnetic resonance imaging (MRI) may be warranted to further assess for soft-tissue involvement.8–10 MRI has demonstrated limited ability to identify onset of avascular necrosis acutely, but may be effective and appropriate to be repeated at 6-12 weeks after injury.8,9 Arthroscopic intervention may be warranted pending severity of findings for capsular or labral involvement, intra-articular loose bodies, or chondral lesions.10,11
Minimal description of conservative management and rehabilitation for football athletes following traumatic hip dislocation exists in the literature. Cooper et al.12 reported the case of a professional running back who experienced a hip subluxation with posterior acetabular fracture with onset of aseptic necrosis identified by MRI six weeks after injury. He was able to return to play after after eight months of conservative management, however there is minimal detail presented in the report of said conservative care. Yates et al.5 described a single case of a high school football player that experienced a posterior hip dislocation who completed conservative care in five months and successfully completed the following football season. Philippon et al.13 reported on 14 cases of professional athletes that required arthroscopic intervention after hip dislocation (12 posterior), all of whom returned to full play. Of those cases, five were football players, and three of them did not undergo surgery until greater than 90 days after injury, implying failed conservative management. However, their conservative care course was not described. While a number of post-surgical hip dislocation rehabilitation protocols exist,14,15 the authors were unable to find any other published detailed rehabilitation progressions for football players post closed reduction hip dislocation.
Case Description
The subject of this case is a 22-year-old NCAA Division I football defensive back who experienced extreme left hip pain following contact with another player with his hip flexed during an early season game. The subject was informed that data collected regarding the case would be submitted for publication.
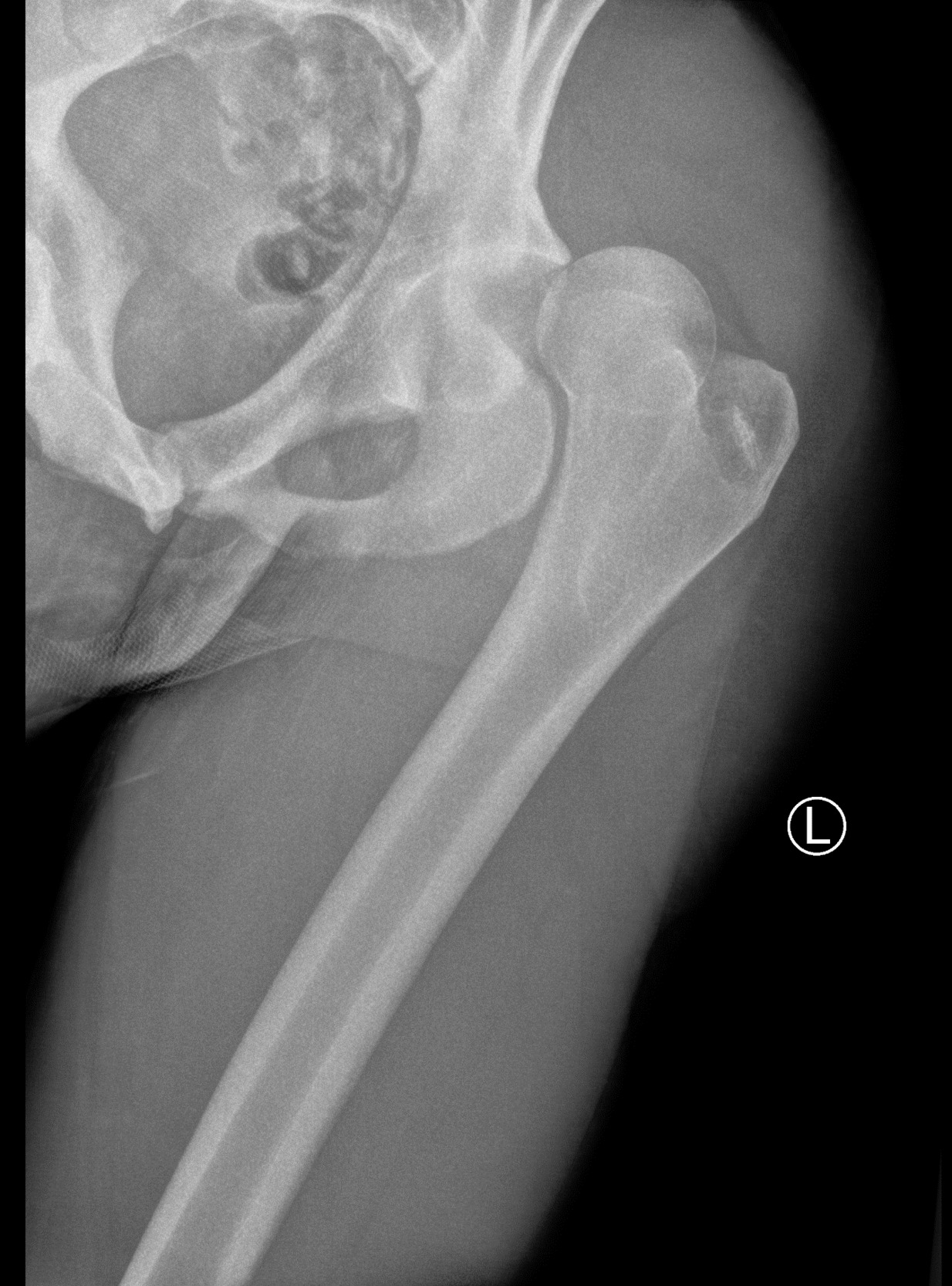
The on-field medical team transported the subject to a nearby emergency room where plain film radiographs revealed a posterior left hip dislocation (Figures 1A-B), negative for fracture, along with mild pre-existing femoral head CAM deformities bilaterally, thus, the diagnosis was consistent with a type 1 dislocation.
The left hip was reduced (Figures 2A-B) and the subject was instructed to be non-weight-bearing on the left lower extremity with bilateral axillary crutches for two weeks, followed by adding 25% weightbearing each week thereafter to weight bearing as tolerated while maintaining standard posterior hip precautions (no hip flexion greater than 90°, no hip adduction, no hip internal rotation) for a total of six weeks. Magnetic resonance imaging was also performed of the left knee and findings indicated a “low grade” left medial collateral ligament sprain.
Three weeks after injury the subject had a chief complaint of ongoing limited function and left hip, knee, and posterior thigh pain. Primary personal goals were full return to sport without fear of repeated dislocation.
Examination
The subject presented to the clinic approximately three weeks after the injury ambulating with bilateral axillary crutches and apparently weight-bearing at approximately 75% on the left lower extremity (LLE), although he had been instructed to be no greater than 25% weight-bearing at that time. He reported 2/10 on the numeric pain rating scale (NPRS) at rest, located in the anterior left hip region, and 5/10 at worst with mild rotational movements in the left hip, knee, and posterior thigh. The subject demonstrated limited left lower extremity range of motion (ROM) and motor performance detailed in Tables 1 & 2.
The subject reported medial left knee pain with active end range left knee flexion, and had an empty endfeel secondary to pain with gentle left hip internal rotation, flexion, and extension. The subject presented with positive grade 1 left knee valgus stress test (mild pain, no gapping apparent), and tenderness to palpation in the left psoas, distal biceps femoris, and medial collateral ligament. Resisted left knee flexion reproduced the subject’s posterior mid-thigh complaint. The subject’s static right lower extremity balance was within normal limits, however the left was not tested in consideration of precautions. He presented with a positive trace left knee effusion as assessed by sweep test and recorded a 51/80 on the Lower Extremity Functional Scale. Dermatomal light touch was intact and deep tendon reflexes were 1+ throughout bilateral lower extremities.
Clinical Impression
The subject presented with impaired left lower extremity motor performance, range of motion deficits, pain, and diminished function and weight-bearing ability consistent with status post traumatic posterior dislocation of the left hip, with secondary soft tissue injury around the hip joint, a grade 1 left MCL sprain, and a grade 1 hamstring strain.
Intervention
The subject was progressed through a phased formal physical therapy program, averaging two visits per week over 14 weeks with multi-modal care including weekly consults with the team physician and the athletic department. Following the 14 weeks, full return to sport was facilitated by the athletic program’s athletic training and strength and conditioning staff. Loading of the left hip and lower extremity was carefully controlled throughout the course of care utilizing rating of perceived exertion,16,17 percentage of pre-injury 1-repetition-maximum (1RM), and a rolling 1.1-1.2 acute to chronic workload ratio18–20 (ACWR) for prescribed resistance exercise, return to run, and plyometric activities.
Acute Phase (0-6 weeks) (Table 3)
This phase emphasized pain reduction, appropriate healing of affected tissues, strengthening of LLE in protected ranges, and re-introduction of weight-bearing (WB) activity with normalization of gait. The subject was instructed by his physician to be non-weightbearing (NWB) on the LLE until two weeks post-reduction, and then to progress to weightbearing as tolerated (WBAT) at six weeks. The subject demonstrated poor adherence to WB precautions in non-clinical areas and was educated at evaluation and thereafter about appropriate percentage of WB. Posterior hip precautions were placed until six weeks post-reduction. Initial treatment included instrument-assisted soft tissue mobilization (IASTM) to the left hamstrings and medial knee region, and manual techniques to reduce left psoas spasm. Progressive resistance exercise (PRE) was prescribed in NWB positions emphasizing left hip external rotators and extensors while avoiding hip ROM precautions, and eccentric training of left knee flexor musculature. As precautions allowed, the subject was encouraged to begin WB with lateral shifting in standing and protected leg press activity, progressing to partial squatting on stable and unstable surfaces. Gait training was performed to normalize gait and progress from bilateral axillary crutch use to single crutch, and then no assistive device. Aerobic and upper extremity conditioning were achieved with progressive moderate intensity upright cycling and seated UE resistance exercise supervised by strength and conditioning staff. After six weeks the subject demonstrated normalized gait, normalized left hip ROM (hip flexion 0-115°, IR 30° at 90° flexion), reported minimal pain at rest and with prescribed activities, and demonstrated improved left hip motor performance, exhibited by hand-held dynamometer and manual muscle tests.
Intermediate Phase 1 (6-10 Weeks) (Table 4)
This phase emphasized progressive loading of the left lower extremity and reintroduction of non-contact impact activity. The subject performed progressive unilateral leg press beginning at 50% pre-injury 1-repetition-max (1RM), elevated conventional barbell deadlift of 50% pre-injury 1RM, and kettlebell goblet squats beginning at 20lb progressing up to 100lb by 10 weeks post-injury. He was prescribed progressive elliptical and pool running aerobic activity for two weeks, followed by initiation of a gradual return to run program beginning with two bouts of 2 minutes of running on the treadmill. Core and hip strengthening interventions included various planks, bridging with physioball, half-kneeling cable column chops, and sidestepping and kickbacks with elastic bands at the ankles. Gentle stretching was prescribed for the left hip flexors and knee flexors. Balance training was performed with single leg stance on unstable surfaces and multi-directional rebounder ball toss on stable surfaces. The subject was barred from performing plyometrics, Olympic lifts, and any agility activities. After 10 weeks the subject was able to asymptomatically perform multiple bouts of five minutes of easy pace running on treadmill and artificial turf, 60% preinjury 1RM elevated conventional deadlift and left single leg press, and single leg stance on stable surfaces with external perturbation.
Intermediate Phase 2 (10-14 Weeks) (Table 5)
This phase emphasized return to plyometric impact activity, agilities, and non-contact sport-specific movement. The subject was prescribed low-intensity single plane agilities without cutting movements, progressing to multiplanar tasks with greater intensity, such as T- and pro-agility style drills with integration of non-contact sport-specific movements. Low-intensity double leg plyometrics were initiated progressing to single leg plyometrics with an emphasis on left hip external rotation control. He initiated a progressive sprinting program during this phase, and performed varied single leg static balance exercises on unstable surfaces with external perturbations. At the end of this phase the subject was able to asymptomatically perform lateral single leg jumps into alternate direction sprint starts, 36-inch double leg box jumps, single leg stance on unstable surfaces with perturbation, 70% of pre-injury 1RM resistance exercise on all non-Olympic lifts (e.g., trap-bar deadlift, elevated conventional deadlift, barbell squat, kettlebell squat), sets of 8 x 40 yard sprints, and all non-contact drills prescribed.
Return to Sport Phase
The subject completed the return to sport phase with the athletic training and strength and conditioning staff. Formal physical therapy care was ended since he had asymptomatically performed the majority of non-contact sport activity and his athletic program staff provided extensive monitoring and care to continue guiding his return to full participation. He successfully returned to a normal training schedule without restrictions for that point in the off-season.
Outcome
Three months following initial injury the subject was asymptomatically performing the majority of non-contact sport activity and training. He was restricted from contact, >80%1RM lower extremity PRE, and Olympic lifts (e.g., clean variations, snatch, jerk). Following a one to two week visit to home the subject returned and continued care with athletic training and strength and conditioning staff. He reintegrated into typical defensive back off-season training approximately four to five months post injury without restrictions.
At seven months post injury, the subject returned to his team physician with report of “pinching” in his anterior left hip with rotational agilities and movements. The physician noted normal strength and range of motion of the left hip, but positive clinical tests for acetabular or labral involvement. A magnetic resonance arthrogram was ordered, which revealed an osteochondral lesion of the superomedial femoral head with underlying intense subchondral marrow signal abnormality and overlying near-full to full thickness cartilage defect of 12x5 mm. There was additional full thickness cartilage delamination with chondral flap posterior and inferior to the osteochondral lesion of 6x6 mm along with a partial thickness, non-detached tear of the anterior labrum, which extended superiorly to the anterosuperior labrum (Figures 3A-B). Mild incipient subclinical avascular necrosis was identified in weightbearing regions of the femoral head.
In consideration of imaging results the subject was recommended the options of a trial of intra-articular corticosteroid injection with prescribed rest or surgical intervention including cartilaginous debridement. The subject selected the surgical option and underwent the surgical procedure almost immediately, which consisted of 10 to 2 o’clock left labral repair with cam osteoplasty and acetabular chondroplasty including; femoral head chondral debridement, iliofemoral capsular thermal plication, loose body removal with anterior inferior iliac spine decompression, and injection of plasma rich platelets and Supartz™ (synthetic joint lubrication).
The subject successfully completed the initial post-surgical protocol at a third-party facility, passed the Vail Hip Sports Test,21 completed a transitional period of physical therapy at the collegiate facility, and was cleared for reintegration into sport approximately four months post operatively. He was able to return to full play in the following football season. Figure 4 details the full course from injury to return to sport the next season.
Discussion
This case report describes the successful return to sport of a Division I football player who sustained a traumatic posterior hip dislocation and complicated course secondary to associated sequelae. Avascular necrosis, chondral lesions, and local soft tissue injury are common sequelae following posterior dislocation,3–6 while AVN is often asymptomatic in its early stages. This subject denied pain symptoms throughout the rehabilitative process and may have experienced an asymptomatic onset. He was closely monitored by a multidisciplinary team including the Chief of Sports Medicine for the school’s associated medical system; two experienced, board-certified physical therapists; the athletic training and strength and conditioning staff; along with coaches, teammates, and family. Thus, it would be surprising if the subject was experiencing symptoms without detection from this team. However, the subject was in a position of team leadership with inherent pressures to perform, demonstrated a consistently positive overall affect and strong work ethic, and was highly motivated. The subject did not report symptoms until they limited his activity – typical of elite athletes – and these psychosocial aspects speculatively may have contributed to a delayed report of onset.
Interestingly, the subject had idiopathic, pre-existing bilateral femoral cam deformities, with alpha angles of 60 degrees. Cam deformities have been noted to potentially contribute to likelihood of posterior dislocation,22 and may predispose an individual to a greater incidence of femoral acetabular impingement and labral tears that was later diagnosed in this subject.10 As such, the cam deformity was reduced during surgery via cam osteochondroplasty.
Magnetic Resonance Arthrogram is an appropriate imaging choice for this subject’s presentation after return of symptoms.10 Similar patients should be referred to their physician upon recurrence or worsening of apparent intra-articular hip pain following posterior dislocation. In consideration of potential occult processes intermittent repeat imaging to examine for potential osteochondral and soft tissue pathology may be warranted in later stages of rehabilitation.
There is almost no published guidance available for conservative rehabilitation of football athletes following posterior hip dislocation. However, the authors were relatively confident that this subject was appropriately progressed using an algorithmic approach to loading based upon pre-injury 1RM’s with observance of consensus safe acute to chronic workload ratios18–20 for PRE and impact activity, in conjunction with consideration of expected tissue healing time and monitoring of subject symptom irritability. A case presented by Yates et al5 included a five-month rehabilitation progression initiated with primarily non-weightbearing progressive resistance exercise (PRE) followed by pool activity to protected squat and leg press training in the second month. That subject was progressed to functional training and low intensity plyometrics in the third month after injury. Running, sprinting, and agility activities were added the following month after demonstrating normalized hop testing. Criteria for release from formal care and return to sport included no pain or difficulty with exercise program and an 80 out of 80 on the Lower Extremity Functional Scale (LEFS). The conceptual progression described in this case report was in agreement with the case study by Yates et al,5 but certain aspects were at a higher level due to the nature of this subject’s ability. A rolling acute to chronic workload ratio of 1.1-1.220,23 was used for progression of PRE and impact activity. Impact was reintroduced using less than body-weight aquatic therapy activities before double to single leg plyometric progressions.
Additionally, patients presenting with type 1 injuries4 without fracture with expedient closed reduction – as in this case – have a better prognosis.4,6,7 Dumont et al10 recommend a structured physical therapy rehabilitation program and that general return to play after 10 weeks is “reasonable” if the patient is asymptomatic. The subject in this case was cleared for return to sport more conservatively at greater than 14 weeks after injury. However, despite the optimistic initial prognosis, cautious and meticulously progressed management, and close multidisciplinary monitoring, the subject experienced common sequelae upon full return to activity requiring surgical intervention.
This report was limited by several factors. Minimal information was available regarding the subject’s training during the approximately four-month period between ending the initial physical therapy course of care and discovery of occult sequelae leading to surgery. The subject’s activity level outside of the clinical and athletic training environments is relatively unknown except based on subject report. Minimal information regarding post-operative care is available. The outcome of this report may not be generalizable to others secondary to the individual characteristics of this subject.
Conclusion
This case highlights the plan of care for a 22-year-old NCAA Division I football defensive back who sustained a traumatic posterior hip dislocation and required surgery to address occult sequelae discovered seven months after the injury. The subject was able to return to full play the following season demonstrating that return to play for an elite contact-sport athlete following traumatic posterior hip dislocation is possible.
Conflicts of Interest
None



__fem.png)




__fem.png)

