INTRODUCTION
Upper extremity injuries in youth and adolescent baseball pitchers remain common, ranging from self-limited, growth-related disturbances including Little League Shoulder to career-threatening injuries such as ulnar collateral ligament (UCL) tears.1–8 Risk factors for injury are multifactorial and include overuse, fatigue, player demographics, throwing volume and velocity, improper biomechanics, and kinetic chain imbalances pertaining to strength, range of motion, and flexibility.3,5,9–11 Technological advances in 3-dimensional (3D) motion analysis and high-speed videography in the past few decades have contributed to a better understanding of pitching biomechanics in pitchers of all ages and levels.12,13 While the preponderance of research has focused on the collegiate and professional pitcher, recent investigations of youth and adolescent pitching mechanics have led to a refined comprehension of critical relationships between functional strength, mobility, and stability as they relate to mechanical efficiency, injury risk, and performance.14–18 Despite these technological advances, pitching-related youth and adolescent upper extremity injuries have reached epidemic proportions.5,19,20 Ulnar collateral ligament reconstruction (the “Tommy John surgery”) now has a higher incidence in 15 to 19 year-old throwing athletes than any other group, including professional athletes.19
The gold standard for assessing pitching biomechanics in all age groups is 3D motion analysis, which provides valuable quantitative measures of pitching kinetics and kinematics; however, it is costly, time- and resource-intensive, typically limited to a single-episode analysis in a laboratory setting, and not accessible to all socioeconomic levels.12–18,21 Consequently, there is a critical need to develop an evidence-based screening tool that can be utilized by a diverse group of users, including coaches, instructors, and sports medicine providers to identify youth and adolescent pitchers with at-risk mechanics and strength/flexibility deficits early in their development. Qualitative 2-dimensional (2D) video analysis, in conjunction with observational measurements, has the potential to be a practical, cost-effective clinical assessment.21 The “Assessment of biomeChanical Efficiency System” (ACES) is an observational measurement tool that was designed by the authors to evaluate pitching mechanics in young baseball pitchers. The ACES consists of 20 scoring items that are rated by 2D video analysis. Although the ACES is an evidence-based scoring system (Appendix I), its reliability has not been assessed; therefore, the purpose of this study was to evaluate the reliability of the ACES screening tool using 2D video analysis to identify common biomechanical errors in adolescent pitchers. We hypothesized that the ACES tool would demonstrate good intra-rater and inter-rater reliability for identifying biomechanical errors in adolescent pitchers.
METHODS
Participants
Middle school and high school male pitchers with a minimum of two years’ pitching experience were recruited from local high schools and from the study institutions’ sports medicine clinics. Pitchers were males between the ages of 12 and 18 years old. Pitchers with any current injury that affected normal mechanics were excluded. Sidearm or submarine pitchers, defined as pitchers who maintain their pitching arm in a low, approximately horizontal plane (eg, at or below the 9 o’clock position for right-handed pitchers, 3 o’clock position for left-handed pitchers as illustrated in Appendix II), were also excluded from the study.
Instrumentation/Data Collection
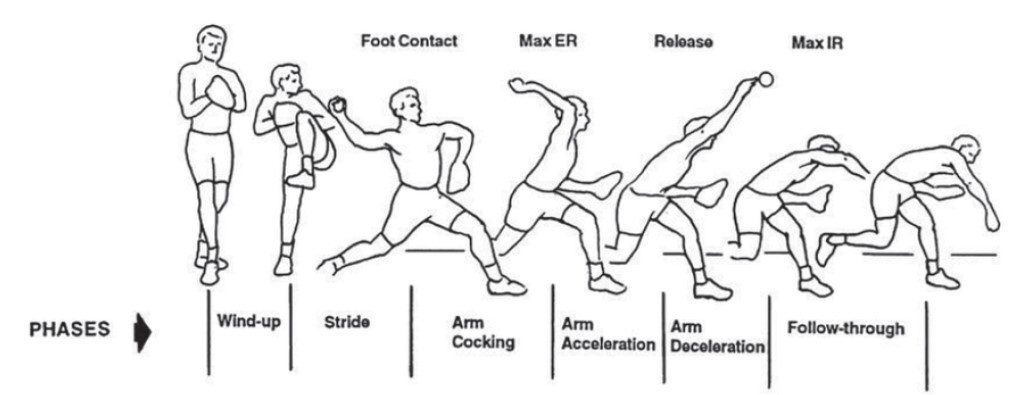
Testing occurred at two different locations (Rhode Island Hospital and Boston Children’s Hospital.) Following a proper warm-up, all participants performed 10 to 25 fastball pitches using high-speed 2D video analysis. The primary investigator (PKK) reviewed all participants’ videos and selected the one pitch that represented their best effort and fastball mechanics for analysis; kinematic variables were then assessed using 2D motion analysis software (Dartfish Inc.; Alpharetta, GA) with commercially available high-resolution video cameras (GoPro Hero 3, 120 frames per second, San Mateo, CA; Casio Exilim Pro EX-F1, 300 frames per second, Tokyo, Japan) recording from frontal and lateral views. Pitchers threw off an indoor mound (ProMounds; Chatsworth, GA) to a catcher (at Rhode Island Hospital) or to a strike zone target (at Boston Children’s Hospital) at a distance commensurate with their level of play. Visual assessment of the upper extremities, lower extremities, trunk, and pelvis was collected and computed through each phase of the pitching cycle (Figure 1).
Raters used a scoring system (ACES) to assess 20 kinematic variables and observational measurements that were identified by biomechanics researchers to be key features of the pitching cycle13 (Appendices I-III), as well as an overall impression of the thrower’s mechanics. Observational measurements were recorded by each rater for the 20 kinematic variables in a binary fashion (1=error; 0=no error). One point was given for each error in the throwing sequence, with a perfect score being 0 and the worst possible score is 21.
Pitchers’ videos were examined by three raters from different clinical sports medicine specialties (orthopedic surgery resident, physical therapist, and athletic trainer) with varying experience analyzing youth pitching mechanics. All raters participated in a 30-minute training webinar and completed five reviews together prior to study assessments. The ACES tool was used to assess the videos twice, with a washout period of two weeks between rater assessments. The research team intentionally chose raters with different career backgrounds because the scoring system was developed for use by a heterogenous group of evaluators (eg, coaches, instructors, and healthcare providers). This cross-sectional study was approved by the Institutional Review Boards of Rhode Island Hospital and Boston Children’s Hospital.
Statistical Analysis
Data on individual items were summarized as frequencies and percentages across all ratings of pitchers by the three raters. Total scores for each rater were summarized as mean and standard deviation and range. Absolute agreement (%) and Fleiss’ kappa (κ) coefficient were calculated to determine intra- and inter-rater reliability of pitching errors for the individual binary items. Intraclass correlation coefficients (ICC) were calculated to determine intra- and inter-rater agreement on total scores. The ICC values were calculated using two-way random effects modeling (Stata Statistical Software: Release 16; College Station, TX) because the same set of raters scored all the pitchers. Agreement was determined based on established interpretations criteria:22,23 poor agreement (< 0.4), fair to good agreement (0.4 to 0.75), and excellent agreement (≥ 0.75).
RESULTS
Twenty asymptomatic male pitchers (mean age 15.1 ± 3.1 years old) participated in the study. The ACES total scores ranged from 1 to 13 and were normally distributed with mean scores across raters of 7.5 ± 3.0; 6.7± 2.3; and 5.5 ± 2.6, respectively. The ACES total score demonstrated excellent intra-rater reliability within each rater (ICC for rater 1 = 0.99 (95% CI; 0.98, 0.99); ICC for rater 2 = 0.94; 95% CI: 0.84, 0.97); ICC for rater 3 = 0.98 (95% CI: 0.96, 0.99)). There was excellent inter-rater reliability across the trials and raters (ICC = 0.91; 95% CI: 0.82, 0.96). For individual items, absolute inter-rater agreement across the three raters ranged from 50% to 100% (Table 1). Intra-rater consistency of individual items was strong, with absolute agreement ranging from 70% to 100%, and kappa values from 0.38 to 1 (Table 1).
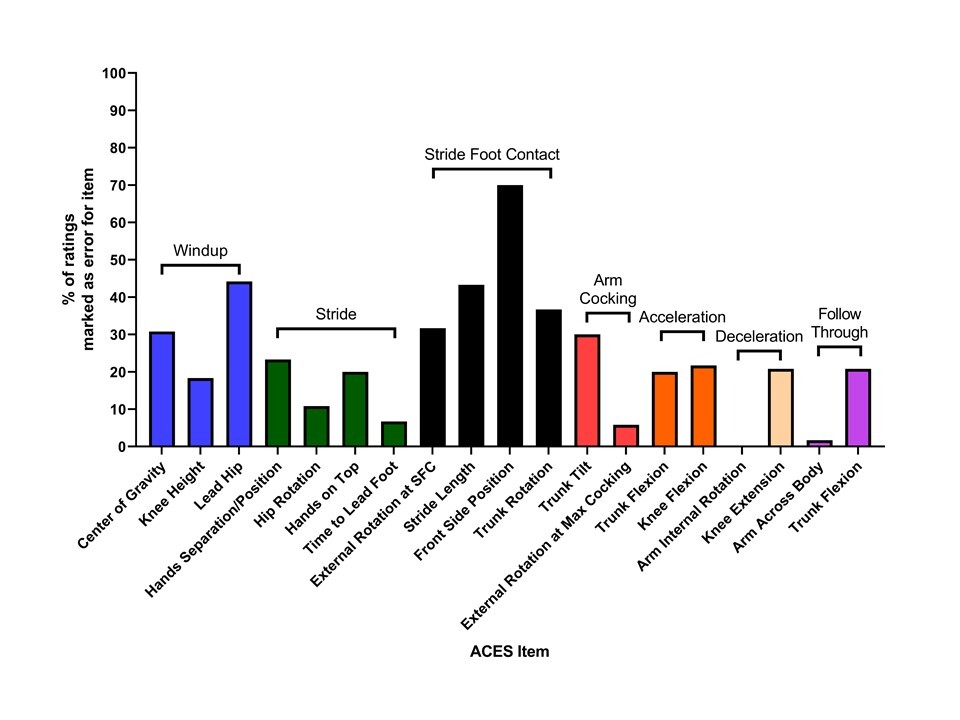
Various items were most often recorded as erroneous by the three raters. Specifically, ACES item 10 (Appendix III) which is designated “front side position” in Table 1 and Figure 2, was rated erroneous in 84 of 120 ratings (70%).
ACES item 9, stride length, was rated erroneous in 52 of 120 ratings (43.3%). Lead hip position, ACES item 3 during the windup phase, also accounted for many errors (53 in 120 ratings, or 44.2%).
DISCUSSION
The purpose of this study was to determine the reliability of a practical, affordable clinical assessment tool utilizing 2D video analysis for coaches, instructors, and sports medicine providers to screen adolescent pitchers for common biomechanical errors. The ACES scoring tool demonstrated excellent reliability for identifying biomechanical errors in adolescent pitchers when administered by raters of different musculoskeletal disciplines. Regarding each ACES item, there was a diverse range of scores; however, acceptable values were found by weighted kappa analysis overall.
Previous authors have analyzed qualitative kinematic variables during the pitching cycle in adolescent baseball players. Nicholls et al.24 evaluated 20 adolescent baseball pitchers using qualitative 2D and 3D motion analysis to validate kinematic variables from the stride, arm cocking, and arm acceleration/ball release phases. Two raters (an internationally recognized coach and a trained biomechanist) conducted an analysis using a 24-item qualitative analysis protocol of ideal pitching techniques. Intra-rater reliability across two trials was fair to excellent, with all 24 items in the checklist producing kappa between 0.400 and 0.900 (in 22 items, p < 0.05). Inter-rater reliability for the qualitative analysis protocol was fair to good (kappa = 0.468 to 0.694, p < 0.05) on 8/24 (33%) qualitative kinematic variables: four stride phase variables (stride offset, foot angle, shoulder external rotation, shoulder abduction), two arm cocking phase variables (glove arm, maximum shoulder external rotation), and two ball release variables (lateral trunk tilt, shoulder abduction).
In an unpublished study (E. Quatromoni, unpublished data, 2015), Quatromoni evaluated 34 adolescent baseball pitchers using high-speed 2D video to assess the intra- and inter-rater reliability of six biomechanical errors [forearm position at stride foot contact (SFC), stride foot position, backward lean at SFC, shoulder position at SFC, trunk to elbow angle at SFC, and contralateral trunk lean at maximal humeral external rotation] of three pitches (trials) analyzed independently by three raters (one former collegiate pitcher and two certified athletic trainers). Regarding intra-rater reliability across the three trials, five of the six biomechanical error items had fair to excellent agreement, producing kappa values between 0.459 and 0.872, p < 0.05. Only open shoulder position at SFC (specifically trial 2 vs. 3) had poor agreement (kappa = 0.242, p > 0.05). Inter-rater reliability of the six biomechanical errors demonstrated mixed results, with three out of six (50%) variables having fair to good agreement (kappa = 0.518 to 0.580, p ≤ 0.001). In the current study involving 20 adolescent baseball pitchers, intra-rater reliability across the two trials was fair to excellent, with all 20 items in the checklist producing kappa between 0.47 and 1. Inter-rater reliability for the ACES scoring tool was fair to excellent (kappa = 0.44 to 1) on 10 out of 20 (50%) variables: three windup phase variables (center of gravity, knee height, lead hip), three stride foot contact variables (external rotation at SFC, stride length, and trunk rotation), two acceleration variables (trunk flexion, knee flexion) and two deceleration variables (arm internal rotation, knee extension). Because these 10 variables had acceptable intra- and inter-rater reliability, these 10 items may be considered key components of a scoring system that can be utilized for identifying impaired pitching mechanics.
Davis et al.14 evaluated 169 baseball pitchers aged 9 to 18 years using 2D video analysis and 3D motion analysis to determine if correct performance of five biomechanical pitching parameters considered to be key elements in youth pitching (leading with the hips, hand-on-top position, arm in throwing position, closed-shoulder position, and stride foot toward home plate) were associated with decreased joint forces at the shoulder and elbow (humeral internal rotation torque [HIRT] and elbow valgus load [EVL]). Interestingly, pitchers that performed both the hand-on-top and closed-shoulder positions correctly were considered to be more efficient than those pitchers who performed these parameters incorrectly. Several ACES items (items 3, 6, 10) were modeled after the parameters of this study.
Regarding individual ACES items (Figure 2), the authors found that one windup phase variable (leading with the hips) and four stride foot contact phase variables (semi-cocked flexed elbow, abducted and externally rotated shoulder—represented as External Rotation at SFC in Table 1 and Figure 2; stride length; front side position; and trunk rotation) were responsible for 271 out of 548 (49.5%) total errors identified by raters (Table 1). Fifty-three of 120 (44.2%) ratings in the current study identified adolescent pitchers leading with the hips (premature forward momentum). In a descriptive laboratory study, Davis et al.14 found that 77 of 83 (92.8%) adolescent pitchers demonstrated “leading with the hips” as well. Surprisingly, “leading with the hips” was associated with higher HIRT, higher elbow EVL, and lower pitching efficiency (efficiency defined as normalized HIRT/velocity and normalized EVL/velocity. These ratios indicate the amount of stress the shoulder and elbow are subjected to for a given pitch velocity generated; the higher the value, the lower the efficiency). While increased forces (↑HIRT, ↑EVL) cannot be considered causal to increased risk of injury,14 several authors have suggested that increased HIRT is a contributor to a physiological condition of proximal humeral epiphysiolysis (Little League Shoulder), as well as humeral retrotorsion, a physiologic adaptation to the proximal humerus that can contribute to increased external rotation and increased velocity.25 While “leading with the hips” may be necessary for generating ball velocity in youth and adolescent pitchers,25–27 it remains unclear whether this parameter should be promoted by pitching coaches since the potential long-term risks (cumulative microtrauma due to increased kinetic forces at the shoulder and elbow) may outweigh transient performance benefits (velocity) in skeletally and physiologically immature pitchers. Consequently, “leading with the hips” was categorized as a biomechanical error rather than a correct parameter in this study.
The culminating event that ends the stride phase (Appendix III), stride foot contact (eg., when the lead foot contacts the ground), has significant biomechanical implications that optimally allow transfer of energy to the distal segments of the kinetic chain. Aberrations in stride length, lead shoulder position (eg, “open” vs. “closed” shoulder position), and stride foot contact position have been associated with increased shoulder and elbow forces28 as well as decreases in ball velocity, which can result in greater demands on the distal kinetic chain to maintain throwing accuracy and velocity.22,29 Stride errors in direction and length can affect trunk rotation velocity and inclination (contralateral trunk tilt) and can lead to the throwing arm lagging behind the scapular plane, which is a known contributor to increased stress on the shoulder and elbow.30 The results of this study demonstrate that ACES items categorized as stride foot contact variables collectively accounted for the largest percentage of erroneous ratings, perhaps identifying stride foot contact as the most important biomechanical event to objectively assess in adolescent pitchers.
Limitations
This study had several limitations. While the ACES tool was constructed by those with backgrounds in researching baseball biomechanics, the contribution of each variable to pitching, the kinetic chain, and overall injury risk remains unclear. Additionally, some components of the ACES tool required that several conditions be met to be graded as “correct,” such as item 10 that consisted of three variables for a correct score; this may have increased error in grading the throwing motion.
This small sample of adolescent pitchers likely represented more frequent pitching inefficiencies compared to higher level pitchers; however, adolescents are the largest subset of pitchers in organized baseball, with more than 6 million adolescents participating in organized baseball in the United States.18 Compared to elite-level pitchers, adolescent pitcher biomechanical studies have been under-represented in the literature. Single-episode study design12,14,16,18,24,25 and studies using only one pitch for 2D video analysis15 (including this study) limit the ability to assess for trends, including correction of biomechanical errors and development of mechanical inefficiency with fatigue in pitchers’ biomechanics. Additionally, the ACES tool may not be generalizable to pitchers with different throwing mechanics which are widely regarded as “non-traditional” (ie, side-arm, or submarine pitchers).
As this study was conducted at two clinical research centers, cameras with different speeds (300 and 120 frames per second) were utilized. While not uniform, these frame rates are within the range of commercial equipment available to the consumer, including coaches, parents, and players. Additionally, the use of a catcher or target was not uniform at the two clinical research centers, as one center standardly used a staff member experienced with catching pitchers during 2D video analysis, while the other center utilized a strike zone target. Lastly, non-healthcare providers were not utilized (eg, youth baseball coach) as a rater in this study, limiting the ability to determine the usefulness of the ACES scoring system for a layperson without specialized training in interpretation of adolescent pitching biomechanics.
CONCLUSION
The results of this study indicate that 2D video analysis and an observational screening tool (ACES) to assess pitching kinematics can be used reliably, due to excellent intra- and inter-rater reliability demonstrated by raters of different musculoskeletal disciplines (orthopedic surgeon, physical therapist, certified athletic trainer). Future studies validating 2D video analysis methodology with 3D motion analysis are warranted before the ACES screening tool is disseminated and employed by coaches and instructors of adolescent pitchers.
Financial Disclosure
The authors have no applicable financial disclosures.
Conflicts of Interest
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.