Introduction
In 2013, the American Physical Therapy Association adopted the vision of “Transforming society by optimizing movement to improve the human experience”.1 Associated guiding principle language (pg. 1) includes “As independent practitioners, doctors of physical therapy in clinical practice will embrace best practice standards in examination, diagnosis/classification, intervention, and outcome measurement.” “The physical therapy profession will demonstrate the value of collaboration with other health care providers, consumers, community organizations, and other disciplines to solve the health-related challenges that society faces”.1
In this collaborative spirit, we must ask ourselves how do we continue to advance the “best practice standards in examination, diagnosis/classification, intervention, and outcome measurement”? Diagnostic classification is a foundational underpinning of providing care of the highest quality and value. As noted by Zimny in 2004 (pg. 106),2
“the basic advantage of, and therefore rationale for, classifying and diagnosing clinical problems in medicine is to impose order on information from clinical and laboratory findings that otherwise would remain chaotic and unconnected. Classification and labeling allow generalizations to be made that can then be used to identify and treat similar problems so that each new patient need not be treated de novo. Furthermore, diagnostic classification and labeling provide a structure which allows clinicians to better predict and compare outcomes of interventions for given categories of disease.”2
Despite the critical importance of diagnostic classification across all of medicine, many pragmatic challenges exist. Zimny2 succinctly summarized primary concerns to include subjectivity in classification, the lack of mutually exclusive and jointly exhaustive categorizations as relates to clinical problems, and difficulty determining the appropriate level of specificity at which to classify. Despite our 100-year history as a profession, and extensive existing diagnostic labels in medicine, limited diagnostic consistency is present in orthopaedic physical therapy.3 An ongoing concern with a lack of diagnostic consistency or specificity in the profession, and in fact across medicine itself, is variation in practice.4,5 Practice variation limits our ability to define, educate, and provide best practice.
In a 2017 International Journal of Sports Physical Therapy article, we introduced a broad framework for shoulder movement system diagnostic classification as an alternative to traditional pathoanatomic diagnoses.6 The purpose of this current manuscript is to provide an update and further illustration of the framework.
Moving Away from Pathoanatomic Labels
Since 2017, there have been growing calls from varied perspectives to move away from medicine’s reliance on pathoanatomic labels.7,8 Rationale for such a change includes considerations of lack of connection between presence of tissue pathology and symptoms such as pain,9 increased understanding of pain processing,10 the presence of comorbid tissue pathologies,11 the high cost and uncertain value of diagnostic imaging,9 the limited value of clinical “special tests”,12 and the influence a diagnostic label may have on patient expected outcomes and perceived need for invasive treatments such as surgery.8,13,14 A recent investigation of over 100 patients with unilateral shoulder pain demonstrated a nearly equivalent prevalence of tissue pathology on the asymptomatic versus the symptomatic side.9 Importantly however, tissue pathology should not be uniformly dismissed either. More advanced pathology such as glenohumeral arthritis or full thickness rotator cuff tears were significantly more prevalent on the symptomatic side as compared to the asymptomatic side.9
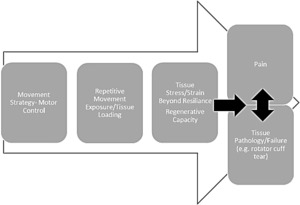
In addition to the above mentioned limitations to pathoanatomic diagnostic labels, it is important to keep in mind that tissue pathology is the “end stage” of multifactorial cumulative trauma injuries common to musculoskeletal conditions15 (Figure 1). There is evidence that malalignment16 or specific repetitive movement joint loading patterns17 can be risk factors for development of musculoskeletal disease such as osteoarthritis. If we strive as health care providers to provide risk mitigation interventions aiming to prevent pain and pathology, we need to be able to intervene before excess tissue stress or strain leads to tissue pathology. This approach has been used successfully with programs designed to reduce dynamic knee valgus to prevent anterior cruciate ligament injury, as an example.18
In musculoskeletal health and disease, numerous diagnostic labels exist and are employed in clinical practice guidelines, as well as coding and reimbursement. There are advocates of moving from pathoanatomic labels to non-specific regional labels as preferred terms.8,19 Examples include diagnostic labels for non-specific low-back pain or shoulder pain of unknown origin.19 We agree with previous advocates8,14,19 that these non-specific labels may reduce unnecessary surgery or over reliance on expensive imaging modalities in cases where specific tissue pathologies are being labeled that do not relate to a patient’s symptoms or function.14 However, the lack of specificity of regional pain labels brings us back to the concern of how do such labels go beyond a restating of the patient’s chief complaint and move toward directing best practice? For example, recent changes in Medicare approved ICD-10 codes occurred in an attempt to require increased specificity regarding low back pain diagnoses.20
Movement System Diagnostic Classification
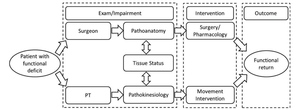
Advocacy has occurred for the use and development of movement system diagnostic labels and classifications as well.21,22 Several labels already exist within traditional musculoskeletal diagnoses that are compatible with movement system labels, for example - instability. A movement system diagnostic classification identifies characteristic movement system impairments, activity, or functional limitations that presumably cause, contribute to, or are caused by the patient’s pain or dysfunction. This classification leads directly to movement focused interventions (treating these impairments or functional limitations). Physical therapist practice already focuses on treating movement impairments. Diagnostic classifications within the movement system can subsequently further direct treatment. Figure 2 demonstrates how for the same patient problem, a physical therapist will focus on a movement system classification to maximize functional outcome for a patient, while an orthopaedic surgeon will focus on tissue status. Both professionals need to understand the other’s area of expertise (pathoanatomy versus pathokinesiology), and how these components interact to impact function and dysfunction for the client.6
It is important to recognize that a diagnostic classification within the movement system would not and should not require new physical therapy “profession specific” diagnostic labels used and understood only by physical therapists.23,24 Rather the classification is specific to the health of a system – the movement system, rather than specific to the health of musculoskeletal tissue (e.g. rotator cuff). The American Physical Therapy Association (APTA) has endorsed the following criteria for use with a movement system diagnostic classification25: 1) Use recognized movement-related terms to describe the condition or syndrome of the movement system. 2) Include, if deemed necessary, the name of the pathology, disease, disorder, anatomical or physiological terms, and stage of recovery associated with the diagnosis. 3) Be as succinct and direct as possible to improve clinical usefulness. 4) Strive for movement system diagnoses that span all populations, health conditions, and the lifespan. Whenever possible, use similar movement-related terms to describe similar movements, regardless of pathology or other characteristics of the patient or client.25
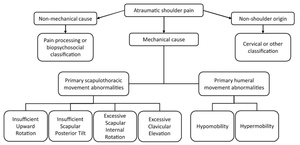
Historically for atraumatic shoulder pain, the most common diagnoses have been shoulder instability, frozen shoulder/adhesive capsulitis, and shoulder impingement/rotator cuff disease.6 These conditions can be easily adapted to a movement system framework (Figure 3) by reframing diagnoses broadly as hypermobility/stability deficit, hypomobility/mobility deficit, or aberrant motion/movement coordination deficit. This classification is not highly specific, but advances specificity beyond regional pain categorizations such as subacromial pain syndrome or shoulder pain of unknown origin. These general movement categories could be easily understood by other health professionals and patients alike, while also beginning to direct physical therapy interventions, since changing movement patterns can alter loading profiles.26,27 Physical therapists can manipulate environmental, individual, or task constraints to allow the patient to attain desired movement patterns through the principles of motor learning.28
Even at this stage of rethinking a classification (three main groups), there are a number of advantages to the movement system based framework, as noted in our previous manuscript.6 First, “the overall treatment goals are derived directly from the diagnostic category: improve functional stability in clients in the hypermobility category; improve functional mobility in clients in the hypomobility category; and improve functional movement coordination or balance of mobility and stability in clients in the aberrant motion category. We would not apply treatments to gain mobility with a client with hypermobility and so forth. This framework further prioritizes the movement in the classification system, and also in the diagnostic process”.6(p888) A movement examination assessing both quality and quantity of movement follows directly after the patient history (Appendix A). Special tests to identify tissue pathology are best used more selectively to potentially modify the intervention approach and inform prognosis and/or coordination of care after identifying a movement classification. Because the movement system is the focus of the diagnosis, there are no issues with scope of practice,29,30 and no over reliance on costly medical imaging. There is also not an assumed connection to immediate surgical intervention (e.g. tissue torn and not repairable without surgery), as opposed to an evidence-based consideration of all factors with surgical referral when needed.
Increased Specificity
Moving to a greater level of specificity in shoulder movement classification is illustrated in Figure 4. For shoulder conditions for example, based on the history (Appendix A), a qualitative movement examination is performed that includes alignment and repeated shoulder movement assessment. The serratus anterior inferior and trapezius muscles play a critical role in both moving and stabilizing the scapula, but have differential contributions in flexion versus abduction.31 Therefore, evaluation of arm elevation into both flexion and abduction overhead reaching is recommended, along with an evaluation of the “problem” movement as reported by the client history. The history and movement examination provide the ability to formulate hypotheses regarding what movement impairments are contributing to or resulting from the patient’s symptoms or dysfunction. The remaining examination can subsequently be directed to confirming/refuting these hypotheses, and reducing reliance on special tests.
In our proposed framework, non-mechanical or unrelated causes (cervicogenic, cardiac conditions) of shoulder pain are ruled out, and primary glenohumeral impairments are distinguished from scapulothoracic impairments. Subtypes of each primary movement impairment are then considered with the understanding that movement emerges as a result of the interactions between individual, environmental, and task constraints.28 From this primary movement impairment pattern, we proceed with additional tests and measures to determine primary movement system contributors such as tissue flexibility, muscle force production, coordination, etc. (Figures 5 and 6). Finally, we assess for important pathoanatomic contributors, such as a tissue tear or nerve injury. This framework of movement system diagnostic classification is presented for shoulder conditions, however, a similar framework can be applied to an array of musculoskeletal conditions. A proposed diagnostic classification for temporomandibular disorders is presented in Figure 7. This classification integrates movement system and pathoanatomic considerations. The flowchart uses objective exam results to classify a movement dysfunction as mobility or coordination deficits with further refinement/specificity of muscle vs. joint involvement. Additional test results refine the pathoanatomic diagnosis according to the criteria outlined in the Diagnostic Criteria for TMD.32 Of note, this classification is inherently multidisciplinary, based on accepted diagnostic classification in dental practice.32,33
With regard to the shoulder, Figure 4 presents common movement patterns recognized in a number of previously described classifications.34–37 These patterns are not typically present in isolation. For instance, insufficient scapular upward rotation is often associated with glenohumeral hypermobility,38,39 and excess scapular internal rotation and insufficient scapular posterior tilt may occur in combination.40 A classification is not determined based on simply the presence of an isolated movement impairment, but instead on the collective history and physical examination, including assistance or symptom relief tests34,41,42 as well as pain provocation tests or movements. Clinical judgement is used to assimilate the collective examination findings in determining which classification is most representative of the client’s movement system dysfunction while incorporating the environmental and personal factors unique to each patient. Figure 5 illustrates that from a movement classification, a clinician can further assess for the associated movement system impairments that would be the focus of a treatment intervention. These representations are not considered all-inclusive or complete, but provide an example of a framework for further investigation. For example, the proposed scapulothoracic patterns represent movement dysfunction in each of the three planes (sagittal - scapular tilting; frontal - clavicle elevation or scapular downward rotation; transverse - scapular internal rotation). Structuring movement patterns in such a way may standardize the clinical evaluation process and the education of new clinicians.37
Case Example
A 22-year-old male presents with a chief complaint of right anterior shoulder joint pain specific to shoulder overhead motions. Pain is easily provoked with unresisted arm elevation, but is of minimal severity (2/10 on a 0-10 pain scale) and does not persist after exacerbating movements are discontinued. Thus he demonstrates a condition with low irritability. He reports aching pain in the joint without numbness, tingling, radiating pain, or substantive weakness. He reports pain began after a feeling of excessive shoulder “strain” while playing volleyball. Arm elevation into flexion is most painful, there is no pain at rest, and arm elevation into abduction is not substantively painful. He is otherwise an active, healthy individual with no confounding demographics or co-morbid conditions. No red or yellow flags are identified.
Qualitative and quantitative alignment and movement assessment demonstrates reduced clavicle elevation and reduced scapular upward rotation with his arms relaxed at his side. Cervical and thoracic posture are unremarkable. As he elevates his arm into flexion, his scapula demonstrates increased anterior tilt rather than expected posterior tilt43 (Figure 8). This individual’s posterior tilt first begins at approximately 90 degrees of arm flexion as determined visually, and shoulder pain is present in the mid to end range of shoulder flexion. Flexion and abduction range of motion are within normal limits but demonstrate reduced scapular upward rotation throughout the range. A scapular assistance test44 with manual support to scapular posterior tilt and upward rotation is positive during flexion. Repetitive motion results in slight increases in his aberrant scapular movement patterns.
Incorporation of surface electromyographic (EMG) assessment into his evaluation demonstrates a substantial delay of his serratus anterior muscle activation as compared to activation of the anterior deltoid when raising his arm into flexion (Figure 9, Participant A). This is consistent with the “reverse action” movement pattern demonstrated whereby unopposed anterior deltoid contraction results in anterior rather than posterior tilt of the scapula as flexion is initiated. Serratus anterior activation begins to noticeably increase above 90 degrees humeral flexion corresponding to the onset of scapular posterior tilt. For comparison, Figure 9 Participant B depicts EMG from another individual who demonstrated typical scapular posterior tilting during shoulder flexion. Serratus anterior muscle activity was similarly increasing along with anterior deltoid muscle activity for the first 70 degrees of flexion producing simultaneous scapular posterior tilt and humeral flexion.
Even without EMG of the muscle activation pattern, the movement examination allows us to streamline our physical examination. We still must assess joint mobility (unremarkable in his case) and overall muscle strength (within normal limits). However, integrating the movement exam and the history allows us to more efficiently complete the physical exam. In this case we need to rule out long thoracic nerve palsy and can do so through basic manual muscle testing of his serratus (within normal limits) which can be further confirmed by surface EMG in this case.
Based on our classification, a movement system diagnosis of insufficient scapular posterior tilt associated with coordination/control deficit is provided. Therefore, his treatment follows from his diagnosis and includes movement training exercises to improve serratus anterior activation45 timing including wall slides46 and scapular protraction with flexion movement training. Electromyographic biofeedback could be helpful in accelerating motor learning to improve serratus activation timing. Specific exercise or biofeedback selection based on the individual’s history and physical exam are examples of manipulating task and environmental constraints to attain a desired change in motor behavior of the movement system.
Limitations
Movement system classification is not without its limitations. First, aberrant movement does not occur in isolation. Rather, movement patterns emerge based on interactions between the individual, environment, and task.28 Thus, it is imperative that clinicians encourage the patient to demonstrate their painful activities in a context similar to that in which symptoms occur. Second, movement is inherently variable occurring on the backdrop of individual biology, anatomy, physiology, and task demands.15,47 Some variability is to be expected and can be assessed as part of the movement system’s ability to adapt to the changing constraints present in daily life, for example eccentric versus concentric loading.48–50 More research is needed to determine how to distinguish expected and potential beneficial movement variation from movement variation that alters tissue loading in detrimental ways. Third, there is potential for misinterpretation of movement systems classification as one “right way” to move. Education should be provided that there is a range of acceptable movement variation. Finally, symptom improvement as a result of interventions may not be related to permanent biomechanical change.27 Effective alterations in movement patterns will redistribute load to reduce symptoms with the goal of allowing a full return to previously aggravating activities. To achieve long-term biomechanical changes, movement system training appears to require task specificity.27
Summary
Meeting our professional vision requires us to “take a seat at the table” with regard to the development and refinement of diagnostic classifications best able to direct practice, maximize patient outcomes, and determine relative value of services. All of these goals further relate to our ability to produce effective clinical practice guidelines, educate future professionals, and achieve the recognition deserved as advanced practice providers. While effectiveness of physical therapy is well demonstrated for shoulder conditions,51 most outcomes do not demonstrate fully resolved symptoms or positive outcomes for all individuals.52 Continued development and refinement of our diagnostic framework is needed. Movement system diagnostic classification can advance and streamline practice if considered while recognizing the inherent movement variability across individuals. To transform society, we must transform, validate, and translate a movement system diagnostic practice to “solve the health related challenges that society faces”.





_collected_on_two_individuals_during_.jpg)








_collected_on_two_individuals_during_.jpg)