INTRODUCTION
Musculoskeletal (MSK) injuries are a leading cause of work disability in the United States.1,2 Over 20.1 million Americans report a disability, with low back pain (LBP) being the primary cause.1 The prevalence of low back pain in a young, athletic population is 18 to 65% compared to 7 to 33% in the general population.3 In a deployed military brigade combat team, the prevalence of low back pain was estimated at 21.2%.4
Annually, over $600 billion is spent on diagnostic imaging.1,5 Overutilization of diagnostic imaging is associated with poor outcomes and increased costs, particularly in the spine, as asymptomatic findings may lead to unnecessary interventions.6–11 Clinical practice guidelines recommend against routinely ordering imaging in patients with low back pain and the National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS) regards any imaging order in a patient with low back pain, in the absence of red flags, within 28 days of symptom onset as unnecessary.10 In 2018, the mean HEDIS score for low back pain imaging ranged from 72% to 76%, depending on the type of insurance,12 meaning that approximately 20 to 30% of patients with low back pain have unnecessary imaging ordered early in their course of care. Despite clinical guidelines recommending against routine imaging in low back pain, utilization rates are rising, with imaging ordered in 14% of encounters in 2011 compared to 16% of encounters in 2016.13
Early access to evidence-based education and clinician-directed exercise is recommended for patients with acute LBP.8,10 Physical therapists practicing in a direct-access setting can provide safe evidence-based LBP management that reduces unnecessary MSK imaging and costs, without elevated risk of harm to patients.14,15
Three recent studies of MSK imaging in physical therapy have demonstrated that physical therapists order diagnostic imaging safely and appropriately. In a five-year retrospective analysis of imaging studies, civilian physical therapists showed appropriate diagnostic imaging use, assessed according to American College of Radiology (ACR) Criteria, in 91% of cases.16 In a two-year retrospective analysis of advanced imaging (MRI) ordered by military physical therapists, 83% were considered appropriate according to ACR criteria.17 Importantly, there were no adverse events in over 1,000 imaging studies ordered by military physical therapists.15
Early access to physical therapy reduces unnecessary imaging, lowers healthcare costs, and leads to better outcomes.14,18 Advanced practice physical therapists are less likely to order radiographs and have lower associated costs than providers working in a similar practice setting.14,19,20 In one study, physical therapists ordered one diagnostic imaging study for every 37 patient encounters compared to one study for every five encounters ordered by primary care providers.15 More research is needed to quantify the value of physical therapists practicing in a direct-access or advanced practice role, determine best practices for ordering imaging for various MSK conditions, and develop educational strategies to improve physical therapist practice regarding diagnostic imaging.
The purpose of this study was to compare rates of compliance with HEDIS recommendations for diagnostic imaging in low back pain between physical therapists and primary care providers in young, athletic patients. We hypothesized that HEDIS compliance would be greater for physical therapists than primary care providers. Secondary objectives were: 1. To compare the frequency of imaging orders with abnormal findings, clinically significant abnormal findings, and findings requiring referral to physical medicine, pain management, neurosurgery, or orthopaedic spine surgery between physical therapy and primary care; and 2. To compare practice patterns for the management of low back pain between physical therapists and primary care providers. It was hypothesized that physical therapists would have similar rates of imaging ordered with abnormal findings, higher rates of clinically significant abnormal findings, and higher rates of findings requiring referral to a specialist compared to primary care providers. Additionally, it was hypothesized that physical therapists would demonstrate different practice patterns regarding the time before imaging, number of active physical treatments, and lower utilization of medication than primary care providers in the treatment of acute LBP.
MATERIALS AND METHODS
This was a retrospective cohort study conducted at the Keller Army Community Hospital (KACH) Primary Care Clinic and the Arvin Cadet Physical Therapy Clinic at the United States Military Academy (USMA) at West Point. The Arvin Cadet Physical Therapy Clinic is a direct access clinic where USMA Cadets with MSK injuries and/or pain are evaluated and treated. The KACH Primary Care Clinic utilizes physicians, physician assistants, and nurse practitioners to serve active-duty military personnel, faculty, and dependents who work and reside on West Point. All physical therapists and providers held the same clinical privileges regarding the ability to order diagnostic imaging. Physical therapists possess clinical privileges to prescribe a limited number of medications, including non-steroidal anti-inflammatory medications (NSAIDs), non-opioid analgesics, and muscle relaxers. The Regional Health Command – Atlantic Institutional Review Board approved the research design and protocol before data collection.
When searching all databases, the patient age range was restricted to 18 to 24 years of age. This patient age range was selected to allow comparison between the Physical Therapy Clinic and the Primary Care Clinic and to generalize results to young, athletic patients. The Arvin Cadet Physical Therapy Clinic is a direct-access clinic that has primary responsibility for evaluating and treating neuromusculoskeletal injuries for USMA Cadets, most of whom are between the ages of 18 and 24. The KACH Primary Care Clinic evaluates and treats medical illnesses in all individuals at West Point while evaluating and treating neuromusculoskeletal injuries in non-Cadets.
The Defense Health Agency Data Driven Decisions Portal (D3Portal) was utilized to view data from the Military Health System Data Repository (MDR) that assesses the use of imaging studies for low back pain HEDIS. Data were available from January 2019 to May 2020. The low back pain imaging HEDIS measure identifies the percentage of patients who did not have an imaging study (X-ray, MRI, CT Scan) ordered on the first encounter with a diagnosis of low back pain or in the 28 days following initial diagnosis (Figure 1).12
A higher rate reflects better performance on the HEDIS guideline, which prevents unnecessary harm and reduces costs. While the goal of the HEDIS measure is to avoid early imaging of patients with uncomplicated low back pain, imaging may be indicated in patients with a history of cancer, recent history of trauma, or significant neurologic impairment. For example, if a patient with acute low back pain and a history of cancer or trauma within the past 90 days receives imaging within 28 days of the initial diagnosis, the patient is considered to have an exclusionary diagnosis and the encounter is removed from the HEDIS calculation.
For the in-depth review of the management of patients with low back pain, the IMPAX imaging viewing software program was searched from 14 June 2014 to 14 June 2020 for patients with diagnostic imaging obtained for low back pain. For each patient identified, the Armed Forces Health Longitudinal Technology Application (AHLTA) electronic medical records (EMR) were independently reviewed by the principal and co-investigator physical therapists. All reviewing physical therapists held board-certification in orthopaedic or sports physical therapy and were fellowship-trained. Patient documentation and radiology exams were extracted, de-identified, and assessed. Demographic data included patient age and sex, duration of symptoms, and location of symptoms. If a provider’s note did not explicitly state the duration of symptoms in days/weeks/months, a period of seven days was input for acute symptoms, 30 days for subacute symptoms, and 90 days for chronic symptoms. Variables of interest included: (1) number of visits, (2) amount of time from initial physical therapy evaluation to imaging order, (3) types of interventions and medications utilized, (4) abnormal findings on diagnostic imaging, (5) clinical significance of abnormal findings. Abnormal findings were defined as any abnormality that was noted in the radiologist’s report. An abnormal finding was considered clinically significant when it altered the plan of care or affected prognosis. Abnormal findings that were considered not clinically significant included mild degenerative changes, findings due to body position, transitional anatomy, or anatomical variants. Clinically significant abnormal findings included moderate degenerative changes, disc protrusions and extrusions, and spondylolisthesis, among others (see Supplemental File Appendix A and Appendix B for full list of abnormal findings). After completion of the case reviews, the three physical therapists met to review each case individually and consensus by discussion was utilized to resolve any differences in the review of radiographic findings.
Statistical analyses were performed in SPSS version 24.0 (IBM Corp), with α = 0.05 set a priori for all analyses. Descriptive statistics were calculated for demographics, the number of imaging orders with abnormal findings, clinically significant abnormal findings, findings requiring subspecialist referral (physical medicine, pain management, neurosurgery, or orthopaedic spine surgery), and the interventions utilized by physical therapists and primary care providers. To compare physical therapists and primary care providers, Chi-square tests were used for categorical variables and t-tests were planned for all continuous variables. Prior to statistical analysis, all data were tested for parametric assumptions. A Mann-Whitney U test was used for duration of symptoms, time to imaging, and visits to imaging due to a non-normal distribution of data.
RESULTS
From January 2019 to May 2020 in patients aged 18 to 24, the MDR database identified 1,845 total visits for LBP identified in the Physical Therapy Clinic and 467 total visits for LBP in the Primary Care Clinic. Total visits encompass only initial and re-evaluations; physical therapy treatment appointments are not included. The comparison of HEDIS compliance for low back pain imaging are shown in Table 1.
In the Physical Therapy Clinic, 96.7% of encounters did not have imaging ordered within the first 28 days of onset of symptoms, compared with 82.0% in the Primary Care Clinic (Chi-Square 136.64, p < .001). Of the 24 physical therapists, 16 were board-certified (6 dual-certified in orthopaedic and sports physical therapy, nine board-certified in orthopaedic physical therapy, one board-certified in sports physical therapy). Of the 24 primary care providers, there were four nurse practitioners, five physician’s assistants, 10 physicians board-certified in family practice, two physicians board-certified in internal medicine, one physician board-certified in pediatrics, one physician board-certified in obstetrics and gynecology, and one general practitioner.
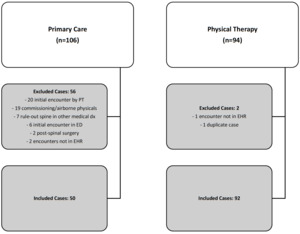
From 14 June 2014 to 14 June 2020 in patients aged 18 to 24 years, the IMPAX imaging viewing software program identified 94 cases of imaging for low back pain ordered by physical therapists and 106 cases of imaging for low back pain ordered by primary care providers. Two cases ordered by physical therapists and 56 cases ordered by primary care providers were excluded, resulting in 92 physical therapy and 50 primary care cases (Figure 2).
Of the 56 cases excluded from primary care, 20 were initially seen by a physical therapist before the primary care provider ordered imaging (six with clinically significant radiographs; four with clinically significant MRI; five referred to specialist). Demographics are shown in Table 2.
There were no significant differences in any demographics of interest between the patients evaluated in the Physical Therapy or Primary Care Clinics. Patients were young (mean age 20.3 +/- 1.3 years) and the majority were male (59%). Acute low back pain was most frequently encountered at 35% of cases, while chronic low back pain comprised 32% of cases. The mean duration of symptoms was 104.8 (226.2) days in patients presenting to the Physical Therapy clinic and 212.5 (417.8) days in patients presenting to the Primary Care Clinic.
The results of diagnostic imaging orders placed by physical therapists are shown in Table 3. Most radiographs ordered were normal.
In Physical Therapy, 55% of radiographs ordered were normal, while 51% of radiographs ordered in Primary Care were normal (p=.673). Conversely, most MRI exams ordered were abnormal. In Physical Therapy, 86% of MRI exams ordered had abnormal findings in the radiology report while 58% of MRI exams ordered by Primary Care had abnormal findings (p=0.50). Disc protrusion was the most frequent abnormal finding (38% Physical Therapy, 42% Primary Care). There were no significant differences in clinically significant findings (31% Physical Therapy, 20% Primary Care, p=.180) or orders which lead to a specialist referral (31% Physical Therapy, 16% Primary Care, p=.059) between the Physical Therapy and Primary Care Clinics.
The summary of practice patterns is shown in Table 4. There were statistically significant differences in the mean time from initial evaluation to first diagnostic imaging order (26.4 Physical Therapy, 7.6 Primary Care, p<.001) and the mean number of visits from the initial evaluation to the first imaging order (3.8 Physical Therapy, 1.1 Primary Care, p<.001).
Physical therapists primarily utilized therapeutic exercise (86%) and manual therapy (54%) in the care of patients with low back pain. Primary care providers primarily referred patients to Physical Therapy (56%) or ordered non-steroidal anti-inflammatory medications (NSAIDs) (50%). Primary care providers were more likely to prescribe NSAIDs (19% Physical Therapy, 50% Primary Care, p<.001) and muscle relaxers (4% Physical Therapy, 18% Primary Care, p=.007) than physical therapists.
DISCUSSION
The primary purpose of this study was to compare rates of compliance with HEDIS diagnostic imaging measures in low back pain between physical therapists and primary care providers in young, athletic patients. Secondary aims were to describe the number of imaging orders with abnormal findings, clinically significant abnormal findings, and findings requiring referral to physical medicine, pain management, neurosurgery, or orthopaedic spine surgery as well as to describe low back pain management and diagnostic imaging utilization by physical therapists and primary care providers. Physical therapists were significantly less likely than primary care providers to order diagnostic imaging within the first 28 days of a diagnosis of low back pain. While physical therapists and primary care providers demonstrated different practice patterns, there were similar rates of abnormal imaging findings, clinically significant findings, and findings that required referral to another medical specialty. To our knowledge, this is the first study to directly compare the performance of physical therapists in a direct-access setting with primary care providers, using a national standardized healthcare performance measure.
Routine imaging for low back pain is not associated with improved outcomes and exposes patients to potential harm in the form of radiation, unnecessary treatment, and increased cost. From 2005 to 2019, data available from the NCQA database that includes all patients aged 18 to 50 years demonstrated HEDIS compliance rates ranging from 73.1% to 78.1% for commercial health maintenance organizations (HMO), 72.1% to 76.2% for preferred provider organizations (PPO), and 71.7% to 79% for Medicaid HMOs.12 In the age-restricted sample, approximately 96.7% of low back pain encounters by physical therapists did not have imaging ordered within the first 28 days of onset of symptoms, compared with 82.0% by primary care providers. In this study, we restricted the range of available encounters to patients aged 18 to 24 to allow for a consistent comparison between the physical therapist and primary care provider groups, which may account for differing rates of HEDIS compliance between this sample and NCQA data.
There were significant differences between physical therapists and primary care providers managing patients with low back pain. Physical therapists waited for a significantly longer duration of time and number of visits prior to the initial diagnostic imaging order. While the difference in visits prior to an imaging order may simply reflect greater access to physical therapists, the length of time prior to an imaging order would be longer with primary care providers if the difference was attributed solely to access to the provider.
Physical therapists were more likely to utilize therapeutic exercise and manual therapy, while primary care providers were more likely to prescribe NSAIDs or muscle relaxers. In a review of studies assessing guideline compliance in low back pain management, physiotherapists prescribed exercise in 89% of cases and utilized spinal manipulation in 30% of cases, similar to the findings of this study.21 In the same review, physicians referred patients to physical therapy in 66% of cases, prescribed NSAIDs in 87-93% of cases, and prescribed muscle relaxants in 67-83% of cases.21 The rates of prescriptions for NSAIDs and muscle relaxers were lower in this study, possibly due to a younger patient sample.
While not statistically significant, the duration of symptoms for patients with low back pain evaluated by physical therapists was half of the duration for patients evaluated by primary care providers (105 versus 216 days). Some may contend that this difference justifies primary care providers to order diagnostic imaging. However, the HEDIS standards do not exclude patients initially evaluated for chronic low back pain and ACR criteria for low back pain does not recommend early imaging for acute or chronic low back pain unless there are red flags or persistent pain following six weeks of optimal medical management. Additionally, the similar distribution of painful body regions (i.e. presence of pain below the knee) and abnormal imaging findings implies that management of both groups of patients’ needs to follow established guidelines.
Physical therapist imaging privileges have been historically controversial. While several states have recently granted physical therapists direct access privileges, most states have not explicitly authorized imaging privileges. In this study, physical therapists practicing in a direct-access setting were significantly more likely than primary care providers to adhere to national quality of care guidelines for imaging in low back pain. These results are consistent with previous reports of appropriateness and safety in the utilization of imaging and provide additional support for physical therapists receiving imaging privileges.15,17 Widespread adoption of imaging privileges for physical therapists will ultimately enhance capabilities as a first-line provider to manage low back pain in a direct-access setting. Additional research is needed to demonstrate the impact these privileges will have on healthcare outcomes, safety, costs, and imaging utilization in other body regions.
Despite a query of radiology orders for greater than a five-year period, there were relatively few imaging orders for young patients with low back pain. While there appears to be a clinically meaningful difference in the proportion of abnormal MRI findings (86% in physical therapy vs 58% in primary care) and those who received a specialist referral (31% in physical therapy vs 16% in primary care), these results were not statistically significant and post hoc power for those two analyses were 0.50 and 0.49, respectively. Larger samples are needed to determine if there are significant differences in the results of imaging ordered by physical therapists and primary care providers and the potential effects any differences may have on overall healthcare costs.
There are several limitations to this study. The sample comprises young, physically active individuals at a single military medical facility, which may limit generalizability to other populations and age groups. Three board-certified physical therapists reviewed imaging orders and extracted results from the official radiologist’s report, which is a potential source of bias for the observational results. The HEDIS system uses visits to establish the denominator; this may skew the metric because physical therapists usually follow-up with their patients more often. Additionally, the evaluation of HEDIS and extraction of imaging information occurred with two separate data sources, although data were taken from the same time periods. As this was a retrospective review, data quality is a limitation. While the encounter documentation was thoroughly searched, providers may have made verbal recommendations to the patient that are not reflected in the electronic medical record.
CONCLUSION
Using data from a national standardized healthcare performance measure, military physical therapists practicing in a direct-access setting were significantly less likely than primary care providers to order diagnostic imaging within the first 28 days of a diagnosis of low back pain in young, athletic patients. Physical therapists and primary care providers have different practice patterns for patients with low back pain, with physical therapists primarily utilizing therapeutic exercise, while primary care providers primarily prescribe medications. Future research should attempt to replicate these findings in large civilian healthcare systems and examine outcomes in patients with low back pain managed by various primary care providers. Examining larger data sets available through electronic medical record systems may also more clearly demonstrate differences in practice between physical therapists in a direct-access setting and primary care providers.
DISCLOSURE/DISCLAIMER
The authors have no relevant or material financial interests that relate to this study. The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the United States Army or Department of Defense.
ETHICS APPROVAL
Study was approved by the U.S. Army Regional Health Command – Atlantic Institutional Review Board.
_metric_for_use_of_imaging_studie.png)
_metric_for_use_of_imaging_studie.png)
