Introduction
The scapula has been identified as a key component of effective shoulder and arm function, due to its roles in scapulohumeral rhythm and its association with a wide variety of clinical shoulder injuries. A series of investigations, consensus groups, and clinical commentaries have established: the definition of scapular dyskinesis,1,2 the relationship of dyskinesis to shoulder pain and injury,3–6 guidelines for operative and non-operative treatment,6–8 and an algorithm for the clinical evaluation process.9 However, the existence of disparate reports on how scapular function can both positively and negatively influence shoulder function has not provided clinicians with clear understanding of the clinical importance the scapula. This is likely due to 3 key characteristics related to scapular function. First, the multitude of muscles that attach to the scapula allow for simultaneous and synchronous muscle activation and stabilization to occur during arm movement. This allows for numerous degrees of freedom to exist which results in variations between individuals performing the same task.10 Second, the thorax has an ellipsoid design which does not allow for single planar movement to occur exclusively. The lack of single planar movement is due not only to the shape of the thorax but also due to the varied fiber orientation of the muscles acting upon the scapula. Scapular motion is comprised of complex rotations and translations which are necessary to allow the scapula to function as part of scapulohumeral rhythm, the integrated coupled motion of the moving arm and scapula that is the basis for effective upper extremity use. The scapular rotations (anterior/posterior tilt, upward/downward rotation, and internal/external rotation) are described as accessory arthrokinematic motions while the scapular translations (elevation/depression and medial/lateral translation) can be characterized as physiologic motions such as the voluntary gross actions of humeral flexion, abduction, or rotation.11–16 Medial translation (dynamic movement of the scapula around the thorax posteriorly towards the vertebral column) and lateral translation (dynamic movement of the scapula around the thorax anteriorly towards the chest) should be used to describe active motion while retraction and protraction should be used to described the end position of the scapula after the movement has ceased.15
Scapular roles involve almost every aspect of shoulder and arm function. It is the “G” of dynamic glenohumeral concavity/compression, the “A” of stable acromioclavicular joint articulation, and “S” of scapulohumeral rhythm.6 Finally, the scapula is a link within the kinetic chain (the coordinated, integrated proximal to distal muscle activity sequencing that allows arm tasks to occur).17 The scapula has a number of crucial roles but most importantly, it serves as the link that transfers energy from the large muscles of the trunk, lower extremity, and core to the smaller muscles of the arm during arm movements.17
Scapular Dyskinesis
When scapular motion becomes altered, the appropriate term to use would be scapular dyskinesis. “Dys” (alteration of) “kinesis” (motion) is a general term that reflects loss of control of normal scapular physiology, mechanics, and motion. Scapular “winging” has been used as a term synonymous with dyskinesis; however, “winging” is best reserved for altered scapular motion driven by neurological compromise.18 Neurologically based winging is clinically observed when any portion of the scapula excessively departs from its contact with the thorax immediately upon the initiation of arm motion and remains disconnected throughout the ascent and descent phases of the arm movement. Conversely, altered scapular positioning can be observed in the resting position of the arm but is more often seen dynamically in the descent phase of arm motion. During the dynamic arm movement, scapular dyskinesis can be clinically characterized by medial or inferior medial border prominence, early scapular elevation or shrugging upon arm elevation, and/or rapid downward rotation upon arm lowering.2 The leading theory is that arm function suffers when scapular dyskinesis is present due to an alteration in the coupled glenoid and humerus relationship.2 However, a cause versus effect relationship between scapular motion and shoulder injury has not been concretely established.6 Considering the literature has consistently noted that scapular dyskinesis, in isolation, is not an injury or a musculoskeletal diagnosis but rather a physical impairment,6 scapular dyskinesis should be viewed as an impairment with a causative origin.
Reconsidering the Clinical Examination
Eighty-three percent of patients with shoulder pain report that the reason for seeking treatment was an inability to achieve their desired function in important activities – they perceived a dysfunction that they wish to be addressed.19 Function can be modelled as anatomy acted upon by physiology to produce mechanics that facilitate accomplishment of a specific task. In this model, dysfunction results from various combinations of pathoanatomy, pathophysiology, and pathomechanics that create ineffective or inefficient decompensations or possible injury that are manifested as symptoms.9,20 This model can be a useful framework to organize the clinical evaluation process.
Systematic reviews have attempted to compile and critique the value of examination maneuvers and have concluded that there are deficiencies in clinical utility, stark contrasts in methodologies between studies, and less than optimal levels of critical appraisal results.21,22 Interestingly, the focus of clinical utility conflicts with scapular dyskinesis as an entity because clinical utility is rooted in diagnostic accuracy. Considering scapular dyskinesis is not a diagnosis but is instead an impairment, clinical utility is not attainable. The difficulty in establishing diagnostic accuracy for an impairment is that there is no consistent acceptable gold standard to compare to. Although several attempts have been made to utilize biomechanical assessments (i.e. 3-dimensional analysis) as a gold standard,23–35 the establishment of where anatomical landmarks reside in space in relation to the equipment based on surface markers are in essence surrogates for actual location. Bone pin studies that insert sterile pins directly into the bone are likely best characterized as a gold standard but their invasive nature and difficulty in utilization prevent them from being routine clinical tools.12–14,16 As such, qualitative assessments of scapular position and motion currently serve as the best clinical tools for identify alterations although there are inherent concerns with the subjective nature of the assessments.
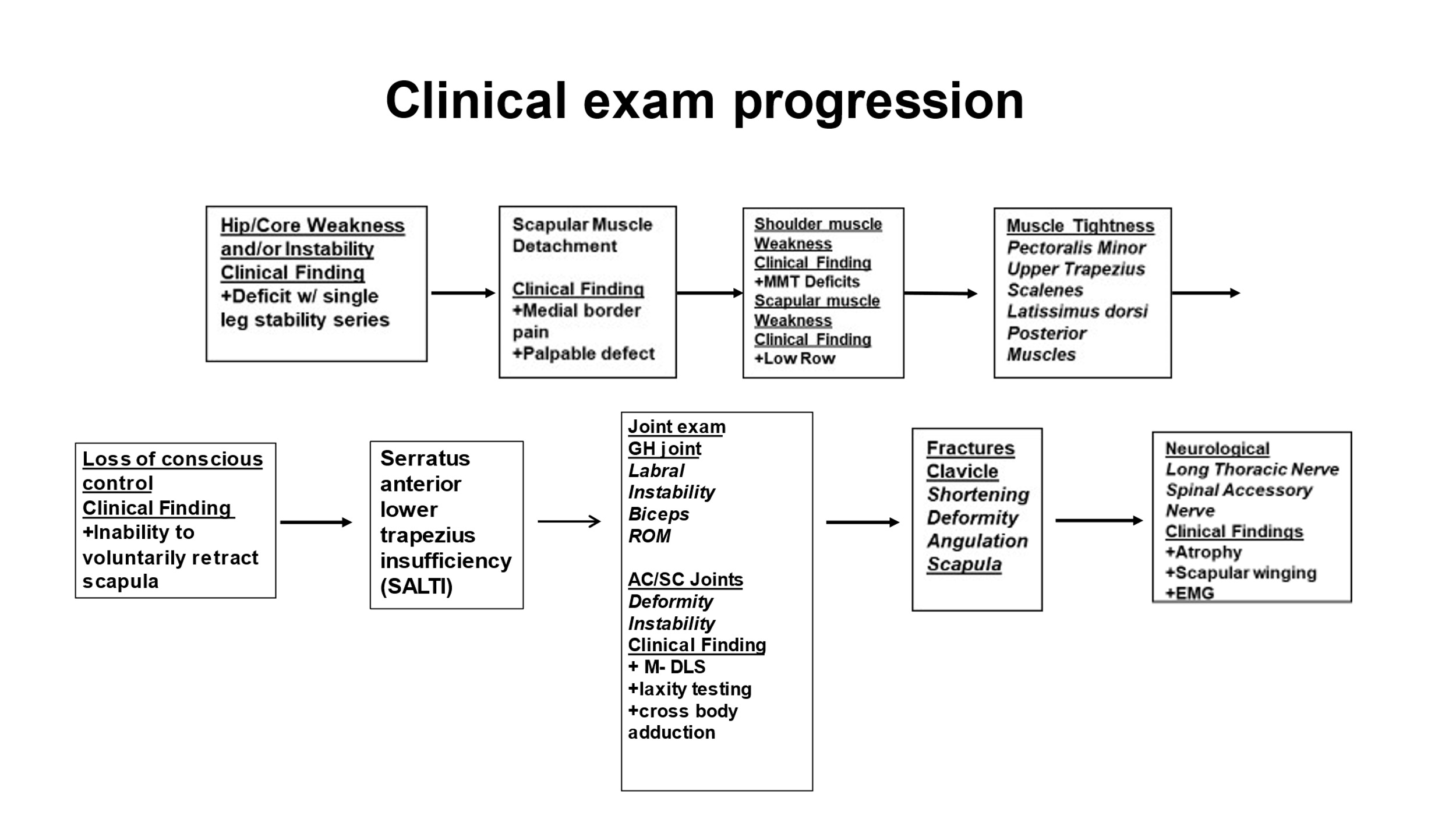
The aforementioned algorithm consists of 3 stages of this qualitative assessment (Figure 1). The first is the establishment of the presence or absence of dyskinesis, using the scapular dyskinesis test.36,37 The second is establishing the relationship between the observed dyskinesis and the clinical symptoms using the corrective maneuvers, the Scapular Assistance Test and the Scapular Retraction Test.1,2,6 The third is the evaluation of the possible causative factors, using a step wise evaluation process and standard testing (Figure 2).18
The establishment of the presence or absence of scapular dyskinesis is best accomplished with the scapular dyskinesis test.6,36,37 The exam is conducted by having the patient raise the arms in forward flexion to maximum elevation, and then lower them 3-5 times (Figure 3). If the clinician is not sure if an alteration of motion is present, the patient can be asked to repeat the scapular dyskinesis test with a 3-5 pound weights in each hand and/or by performing up to 10 repetitions of arm elevation. The added weight and additional repetitions may help accentuate any altered motion. As noted earlier, scapular dyskinesis is more easily observed in the descent phase of arm motion. Prominence of any aspect of the medial scapular border on the symptomatic side is recorded as “yes” (prominence detected) or “no” (prominence not detected).
Three muscle tests: manual resistance of the arm at 130° of flexion (targets the serratus anterior),38,39 manual resistance of the arm at 130-150° of abduction (targets the lower and middle trapezius),38 and extension of the arm at the side (targets the rhomboids)40 should be performed. The distinction between these testing maneuvers and other muscle tests for the shoulder is that the clinician attempts to “break” the patient’s arm position and observe if the scapula is visibly moving out of position. The combination of both the break in position and scapular movement are suggestive of scapular muscle weakness.
Finally, the corrective maneuvers designed to “correct” scapular motion and/or scapular positioning should be employed.6 The scapular assistance test helps evaluate scapular contributions to shoulder pain based on motion alterations, the scapular retraction test evaluates scapular contributions to rotator cuff strength, and the low row evaluates contributions to arm strength. The scapular assistance test is performed when the examiner applies pressure to the medial aspect of the inferior angle of the scapula to assist scapular upward rotation and posterior tilt as the patient elevates the arm (Figure 4). A positive result occurs when the painful arc during arm motion is relieved and the arc of motion is increased. The scapular retraction test is performed when the examiner first grades the strength in forward flexion using standard manual muscle testing procedures with the patient in their normal posture (Figure 5A). The examiner then places and manually stabilizes the medial border of the scapula in a retracted position while retesting the arm strength (Figure 5B). A positive test occurs when the demonstrated strength increases while the scapula is in the retracted position and stabilized by the clinician. In the low row test, the patient is asked to place his or her arm in slight humeral extension and then instructed to resist movement of the arm into forward flexion (Figure 6). The examiner (positioned posterior to the patient) then instructs the patient to contract the gluteal muscles while applying the same anterior force on the arm. If strength increases with the gluteal contraction, this is an indication that scapular and shoulder muscle activation may be facilitated by involving hip and core strength, which suggests lower extremity/core strengthening should be included in the treatment plan for the shoulder. A positive corrective maneuver informs the clinician that the rehabilitation should primarily focus on scapular mobility, scapular strength, or core strength rather than take a rotator cuff activation or strengthening focus.
This qualitative approach aligns well with recent proposals on applying a classification system in the clinical setting that is based on movement-impairments rather than pathoanatomy.9,20 The system begins broad but can be subclassified based on the examination findings. The focus of the system is to help identify causes of dysfunction in order for the examination to better guide the treatment. For example, if altered scapular motion is identified via the scapular dyskinesis test, the clinician should initially identify the specific observable components (i.e. medial border promienance, scapular body positioning, etc) and simultaneously consider what is the likely cause of the alteration (i.e. deficiencies in mobility, strength, and/or motor control, or overt anatomical injury). The additional examination components of the corrective maneuvers, mobility testing, strength testing, and kinetic chain testing would help the clinician better identify the contributing cause.
All these efforts have been directed towards establishing the clinical diagnosis of dyskinesis and identifying the anatomical (pathoanatomy) and physiological (pathophysiology) factors underlying the observed alterations of position and motion as a basis for developing treatment protocols. An unpublished survey from our institution of 462 consecutive patients with shoulder pain who met the algorithm stage 1 and stage 2 criteria were examined for all causative factors, using the step wise testing protocols. This survey revealed that 34.7% of the patients had a pathoanatomical basis for their dyskinesis (clavicle fractures, acromioclavicular joint disorders, glenohumeral joint internal derangements, neurological injury, periscapular muscle injury), while 65.3 % had a pathophysiological basis (muscle imbalance, inhibition, tightness/inflexibility, serratus anterior/lower trapezius insufficiency). In addition, some of those with a pathoanatomical basis also had primary or secondary pathophysiology as well.
These findings suggest a 2-part evaluation process for patients with observed scapular dyskinesis that can be linked to the clinical symptoms. One part should identify those patients whose dyskinesis is secondary to identified pathoanatomy. Treatment may include rehabilitation but frequently will require surgical means of restoration of the anatomy. Those whose dyskinesis is secondary to pathophysiology will need aa comprehensive evaluation process to understand the muscular alterations that will serve as the basis for treatment.
In summary, scapular dyskinesis associated with clinical symptoms results from pathoanatomy in roughly 1/3 of the cases. The absence of demonstrable pathoanatomy is common and should direct the evaluation process to a comprehensive evaluation of the many possible alterations of physiology.
Reconsidering Treatment Approaches
As an impairment, scapular dyskinesis has been posited to be primarily the result of soft-tissue deficiencies, thus the treatment focus has centered on mobility and strength enhancement.5–8,17,41–52 However, various reports have noted that interventions directed at correcting these deficiencies, mostly manual therapy and therapeutic exercise, have little influence on the scapular motion itself.48,49,52,53 There are several possible reasons for these findings.
First, mobility alterations are rarely acute in the scapula and/or shoulder. Although overhead athletes often experience an acute decrease in glenohumeral rotation following a throwing episode/exposure, the decrease in motion can resolve within 24-96 hours on average both with and without intervention.54–59 The chronicity of mobility deficits tends to be lengthy resulting in bony adaptations, capsular thickening, and various tendon responses.60 Although immediate gains in motion have been reported following the application of manual therapy interventions, they have not been shown to be long lasting.61–69 These interventions have positively impacted pain and self-reported function which is more likely rooted in the neurophysiological effects related to endogenous pain control.66 In other words, the immediate clinical but unsustainable result of increased motion after the application of manual therapy is not related to tissue correction but rather pain modulation that results in immediate demonstrable motion increases.
Second, therapeutic exercises designed to target specific shoulder and scapular muscles have been described but these were primarily identified with electromyographic methodologies.70–76 Although electromyography has helped identify which positions and maneuvers bias specific muscles, the oft mistaken interpretation of the results is that the muscle activity is an occurrence specific to individual muscles. This thought process conflicts with the known summation of activation phenomenon that has been consistently reported in the literature.77–85 Furthermore, the foundational work was performed on asymptomatic individuals.70–75 It is quite possible that differences exist between individuals with shoulder pathology or impairments such as scapular dyskinesis compared to those who are asymptomatic. Finally, the identified maneuvers were often performed in an isolated manner with the body in vertical or horizontal (prone or supine) stationary positions. These positions could lead to a less than optimal rehabilitation outcome likely due to the encouragement of inefficient or improper motor patterns.6,34,86–89 Taken together, these results suggests that a focus on increasing strength may not be the ideal intervention.
Finally, if strength shouldn’t be the focus, then it is possible scapular dysfunction is more likely rooted in issues related to motor control. One of the primary principles of motor control is based on the type and amount of feedback a person receives during task performance.89–92 In most upper extremity tasks, visual feedback is utilized for joint positioning and error correction. However, the scapula cannot be visualized due to its posterior location on the thorax. It is possible that the lack of visual feedback leads to the alterations in motion that manifests as scapular dyskinesis. Previous reports have shown that intentional attempts at repositioning the scapula prior to elevating and/or rotating the humerus, called conscious correction, increases scapular muscle activity and enhances scapular kinematics.34,86,89 Additionally, visual feedback,93–97 auditory feedback,93,94 and kinesthetic feedback93,94 have been shown to positively influence scapular muscle activity and positioning. Considering the scapula as a ‘link’ within the kinetic chain, the feedback approach may be better suited for re-establishing scapular control as it relates to the sequential activation within the kinetic chain. The isolated strengthening approach may not re-establish scapular mobility and control as they are single-planar by design and do not allow for the patient to intently focus on the scapula directly. Using motor control as the focus, previous reports have suggested employing an integrated approach where the patient is required to perform exercises from a sitting or standing position to perform (and learn) the necessary motor patterns that require integrated use of the majority of the kinetic chain segments (i.e., using the legs and trunk to facilitate scapular and shoulder movement and muscle activation).41,47,98–101 However, although these works have verified increased shoulder and scapular muscle activation when trunk and/or leg movements are integrated into the exercise maneuvers, there are no empirical reports or randomized control trials that have compared a motor control/kinetic chain focused program against a program that does not utilize this approach.
To date, clinical recommendations supporting motor control/kinetic chain-based rehabilitation approaches have been made via expert opinion/consensus papers.2,6–8,102,103 An example of such a program has been provided with the clinical highlights being:
-
Short lever progression
-
Sitting and standing preferred over prone or supine exercises
-
Target impairments in the order of mobility, motor control, strength (if necessary) and endurance
-
Utilize longer lever maneuvers later in the rehabilitation program
-
Advance to plyometric based maneuvers just prior to discharge
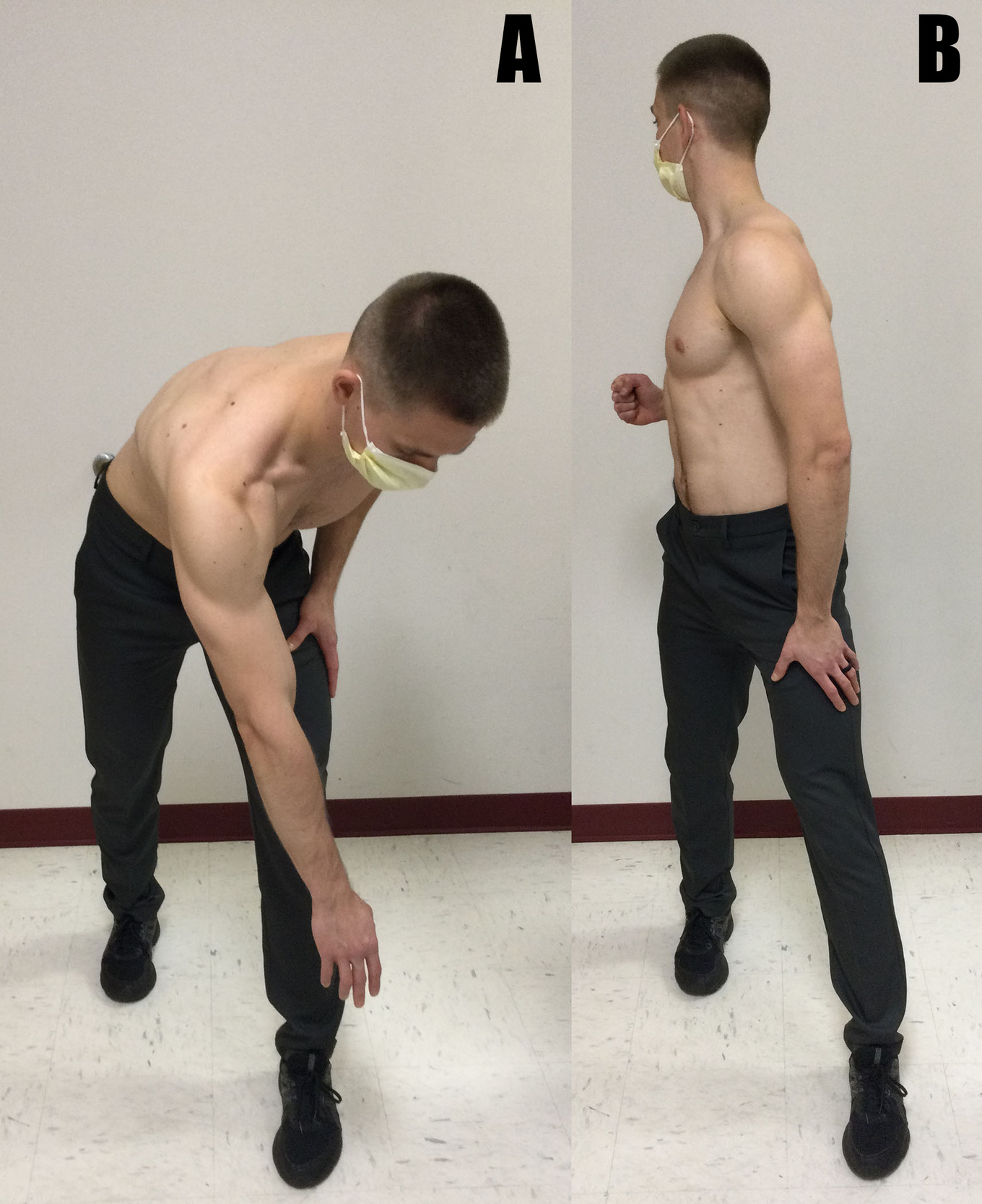
An example of short lever exercise application would be to begin with exercies that require the arms to be in an adducted position (i.e. the arms position against the thorax) rather than positions that require the arms to be elevated or abducted for exercise performance (Figure 7A-B and Figure 8). These early interventions attempt to establish proper scapular positioning early in the rehabilitation and begin to utilize the major of kinetic chain segments to create the integrated muscle activation and sequencing. Although they could be classified as short lever exercises, maneuvers such as scapular shrugging or elevation should be avoided in the first 4-6 weeks of rehabilitation. This is intentional to not overly bias the upper trapezius which could delay the restoration of balance amongst scapular muscle activation. Progression into more dynamic motions that would still be considered short lever maneuvers (Figures 9 and 10) may be added to the treatment progression once the patient has demonstrated that the initial exercises can be performed without exacerbating the previous symptoms. Progression into dynamic motions that begin to include limited amounts of arm elevation or abduction (approximately 30-45°) (Figures 11 and 12), and then culminating with traditional long lever exercises (90° of arm elevation or abduction) in the later or last stages of rehabilitation can be incorporated into the treatment program in the later phases of rehabilitation, but only when the previous maneuvers have been mastered by the patient and have demonstrated little to no symptom exacerbation. Dosage recommendations include beginning with 1-2 sets of 5-10 repetitions with no external resistance. Additional sets and repetitions can be added based on symptoms and exercise tolerance, with a goal of 5-6 sets of 10 repetitions being able to be performed without an increase in symptoms before adding resistance. Resistance may be added next beginning with light free weights (2-3 pounds maximum) and then progressing to elastic resistance. The stability of free weights allows those devices to be utilized prior to elastic resistance because elastic resistance, although effective at increasing scapular muscle activity,100 has high variability when used by patients, especially when arm position is progressed throughout a treatment program.104 If elastic resistance were to be utilized, it can be adequately monitored and progressed using perceived exertion scales.105 Feedback may be incorporated throughout the treatment program but there is not an exclusive type to recommend considering various forms of feedback have been shown to have positive clinical influence.93–97 However, it should be noted that too much feedback can be detrimental to learning as the patient becomes reliant on the knowledge of performance.90
Conclusions
Scapular dyskinesis is an impairment that has causative factors, and those factors should be discerned from a comprehensive physical examination. The examination should not exclude assessments related to identifying pathoanatomical causes but the pathoanatomical approach should not be the primary focus of the examination. Using clinician experience and the best available evidence, a qualitative examination for determining the presence or absence of a scapular contribution to shoulder dysfunction is currently the best option widely available to clinicians. Future investigations should attempt to standardize methodological approaches to perform better comparisons between studies and generate higher quality results. Finally, rehabilitation approaches should be reconsidered where enhancing motor control becomes the primary focus rather than increasing strength.





_and_being_instructed_.png)
._the_p.png)



_and_per.png)





_and_being_instructed_.png)
._the_p.png)


_and_per.png)