INTRODUCTION
Nonoperative treatment of acromioclavicular (AC) joint injuries has been reported in numerous cohorts with varying results based on the severity of injury.1–5 Nonoperative treatment of AC joint injuries has proven benefits based on the similar outcomes identified in comparative studies of nonoperative and operative treatment.3,4,6–39 The consistent summation of findings has identified that operative treatment is better suited for reducing the separated joint per 2-dimensional radiographic assessments while nonoperative approaches typically result in quicker return to activities of daily living, work, and/or sport activities. However, although a reduction of symptoms can be achieved through nonoperative treatment methods for low-grade injuries,40 residual deficits in function can remain from six months to five years following injury.41 Similarly, others have revealed that patients undergoing nonoperative care for low-grade injuries could expect symptoms to resolve by 12 months; however, patients with lingering symptoms at six months correlated with those who were symptomatic beyond one year.42
Conversely, other investigators have identified a higher incidence of unfavorable outcomes with nonoperative treatment, which led them to suggest that adverse outcomes were likely underestimated.43 A long-term follow-up study found that more than half of patients treated nonoperatively experienced symptoms and obtained noticeably lower functional scores when compared with the uninjured shoulder approximately 10 years after sustaining Rockwood Type I or II injuries (Table 1).44 While differences in joint dimensions were detected by ultrasonography, radiographic degenerative changes were not observed.44 This suggests that although joint health appeared relatively unaffected from a 2-dimensional radiographic assessment, 3-dimensional function remained negatively affected. Deficiencies in 3-dimensional function would have consequences for rehabilitation protocol design as exercise selection would need to be re-evaluated. The use of 2-dimensional alignment as an outcome overlooks the complexities of 3-dimensional shoulder function including: 1) possible alterations of scapulohumeral rhythm (SHR) defined as the coupled sequenced motion of the scapula and humerus in all phases of arm motion and 2) the re-establishment of AC and coracoclavicular (CC) load transfer.
Despite the existence of numerous case series comparing operative to nonoperative interventions,3,4,6–39 no study has identified the frequency and type of nonoperative treatment methods utilized in each study. Considering evidence-based rehabilitation would likely be based on the efficacy of the interventions examined in the literature, it would be helpful for clinicians to know which nonoperative treatments have in fact been compared against operative treatments. Therefore, as part of this clinical commentary, the authors systematically reviewed the literature to identify which nonoperative interventions for AC joint injuries have been utilized in empirical studies as well as the parameters of application. This information could serve as the foundation for developing evidence-based recommendations for clinical practice.
ACROMIOCLAVICULAR JOINT FUNCTION AND INJURY
Efficient upper limb mechanics requires coupled motions of the clavicle and acromion, with the AC joint acting as a stable articulation. The S-shaped clavicle acts as a 1) strut, maintaining length and stiffness,45,46 2) crank handle, allowing large amounts of distal rotational arcs of motion for small amounts of proximal rotation,47–49 and 3) the only bony attachment of the upper extremity to the axial skeleton. The clavicle has minimal muscular attachments with most of the clavicular long axis rotation, anterior/posterior motion, and elevation/depression occurring through the influence of scapular motion.
The AC joint is a relatively stiff structure, with strong posterior, superior, and anterior ligament components that are thicker on their acromial insertions than their clavicular insertions.50 Individual AC joint motions average 5° of acromial elevation and 8° of acromial rotation.51,52 A 3-dimensional kinematic analysis of the AC joint, demonstrated that the scapula rotated 35° on an axis (termed the ‘screw axis’) that passed through the insertions of the AC and CC ligaments, and that with abduction, the lateral clavicle translated 3.5mm in the anterior/posterior direction and 1mm in the superior direction.53 This stiffness creates a strong link that allows rotational and elevation motions produced by the scapula or clavicle to be efficiently transmitted to the other bone of the articulation.54,55 Interruptions of the normal integrity of the AC and CC ligaments change the normal linkage between the scapula and the clavicle and can result in dyskinetic motion patterns during limb movement. In addition, indirect AC joint stability and stiffness is maintained by the CC ligaments. An uncompromised clavicle and AC joint are imperative components to maintaining scapular integrity. Injury to any of the static restraints can cause the scapula to become unstable which in turn will negatively affect arm function. Thus, intact AC joint anatomy is the basis for optimal arm and shoulder mechanics as it creates the most efficient screw axis and allows efficient SHR.
INJURY MECHANISMS, PATHOMECHANICS AND INCIDENCE
The mechanism of traumatic AC injury is a progression of loading due to imposed trauma, such as a fall onto the shoulder. Studies have demonstrated the progression of the initial anatomic disruption from the posterior and superior AC ligaments to the anterior AC ligaments.49,56–58 These ligaments are avulsed off their clavicular attachments and create horizontal and rotational laxity,57,58 and the loss of the lateral tension band. Progression of the disruption can occur through the inferior capsule into the substance of the trapezoid and conoid ligaments.59 This creates the vertical instability and the loss of the optimal force and motion transfer between the scapula and clavicle.
The deformity that occurs because of AC joint subluxation or dislocation results from the dissociation of the scapula from the supporting strut of the clavicle.46,49,60 Gravity displaces the scapula downward and there is a concomitant scapular protraction and internal rotation such that the scapula is displaced medial to the AC joint.60 With displacement of the scapula there are significant functional consequences in the biomechanics of the shoulder. There is an uncoupling of the scapulohumeral complex such that the scapular stabilizing muscles are not able to maintain appropriate positioning of the glenohumeral and acromiohumeral joints.61 This uncoupling creates an alteration in SHR. There is also a subsequent loss of rotator cuff strength and function that can only be restored by retraction of the scapula and restoration of the pivot point of the AC joint.62,63 The malposition of the scapula may also lead to impingement of the rotator cuff.64,65 As the arm is elevated the orientation of the acromion remains in an anteriorly tilted position relative to the humerus. In the acute injury there may be inhibition of shoulder function due to pain initially; however, as the acute symptoms resolve there can be chronic dysfunction of the shoulder that occurs due to the anatomical disruption.50 This is due to the loss of the strut function of the clavicle and loss of appropriate scapulohumeral orientation. This results in pain at the AC joint, external impingement, and loss of function during work and recreational activities that require forward elevation. The inability to adequately retract the scapula leads to an apparent loss of rotator cuff strength and loss of cocking or the ability to appropriately position the arm for overhead athletic and work activities.
The incidence of AC joint separations or dislocations ranges from 1.7 to 9.2 per 10,000 individuals.66–69 In athletes such as collegiate and professional football players as well as military cadets, the incidence increases to 3.3 to 26 per 10,000 exposures.70–73 The literature demonstrates that males sustain anywhere from 2.2 to 8.5 more AC joint separations than females.66,72,73 Low-grade separation (Rockwood Types I and II) occur more often compared to high-grade separations (Rockwood Types III and higher), ranging from 4-11%.70–72
LITERATURE ASSESSMENT (NONOPERATIVE TREATMENT)
To provide nonoperative treatment recommendations, the literature was systematically searched for articles based on the following inclusion criteria: English language only; cohort studies that compared nonoperative to operative treatment methods or cohort studies/case series with exclusive description of nonoperative treatment only. The focus was on identifying the treatment methods employed and the results or outcomes of the treatments. Articles were excluded if the treatment methods were not described or able to be discerned based on the provided descriptions. Articles determined to be literature reviews (nonsystematic reviews), current concepts/opinion papers, or single patient case studies were also excluded due to the level of evidence being below Level 4. Additionally, abstracts published in peer-reviewed journals as special editions or supplements or any non-published data were not included.
The results of the review were compiled and tabulated through a standard frequency analysis to identify the commonly used nonoperative treatment components. Reported outcome measures and outcome results were summarized and reviewed for commonalities between reports. The Joanna Briggs Institute Critical Appraisal Checklist for Case Series was utilized to assess the quality of each article retained for the review.74 The assessment sheet was comprised of 10 questions where each question could receive an answer ranging from yes, no, unclear, or not applicable. This scoring sheet was modified to a binary (“yes” = 1 or “no/unclear/not applicable” = 0) scoring system yielding a possible 10 points, to better illustrate commonalities between retained studies. One of the authors (ADS) with over 20 years clinical and research-related experience individually reviewed and appraised each retained article.
LITERATURE RESULTS
A total of 61 articles were identified via the search strategy for possible retention (Figure 1). After applying the inclusion criteria, 33 articles were excluded, and 28 articles were retained for review. All details specific to the nonoperative treatment components of retained studies are summarized in Appendix A. Twenty-three articles (82%) compared operative to nonoperative treatment while five articles (18%) exclusively employed nonoperative treatment. The most utilized nonoperative interventions across all 28 studies were immobilization (i.e., sling) (100%), shoulder motion (61%), and general shoulder strengthening (50%). Medication was prescribed in 29% of studies. Ice and scapular strengthening were mentioned in 18% and 14% of studies, respectively. Few studies (18%) reported on rehabilitation parameters (i.e., frequency, intensity, sets/repetitions).
All outcome measures and results are summarized in Appendix B. Of the 23 studies that compared operative to nonoperative treatments, review of the outcomes revealed three commonalities: 1) nonoperative treatment permitted earlier improvements in subjective outcomes, but no differences occurred at long-term follow-up after six months,9,13,26–29,31–35 2) operative treatment resulted in better joint reduction,9,27,30,31,34,38 and 3) nonoperative treatments resulted in faster return to activities, but residual symptoms such as pain and joint instability may persist.7,25,36,37
Of the five studies that exclusively utilized nonoperative treatments, the nonoperative treatment components (Appendix A) and outcomes (Appendix B) varied between the studies. The nonoperative treatment components included: immobilization,24,42–44,75 medication,42–44 ice,43 motion,24 scapular strengthening,24,44 and shoulder strengthening.24,43,44 Exercise details were provided for one study only.24 Carbone et al.,24 reported 78% of patients had no scapular dyskinesis and improved subjective functional outcomes (Constant and Subjective Shoulder Value) at one-year follow-up. Similarly, Mouhsine et al.,43 reported 52% of patients were asymptomatic at six-year follow-up. Verstift et al.,75 reported a significant reduction in Constant score in the involved arm compared to the contralateral arm as well as substantial radiographic changes such as an increase in AC joint space, osteolysis, ligament ossification, and distal clavicle deformity at an average follow-up of seven years. However, this same group reported Simple Shoulder Test (SST) and Disabilities of the Arm, Shoulder, and Hand scores for the involved arm that were “acceptable” compared to the contralateral arm.75 Conversely, Mikek44 reported decreased Constant, SST, and University of California Los Angeles scores at long-term follow-up (average 10.3 years) while Shaw et al.,42 found significant correlation between high levels of pain/restricted movement and high levels of disability as well as significant correlation between symptoms at six months and symptoms one month prior to one-year follow-up.
Critical appraisal of the retained studies revealed an average score of 6/10 (Appendix C). While all articles reported follow-up outcomes and utilized appropriate statistical analyses, two articles did not report patient demographic information.21,22 Eight articles (30%) did not have clear inclusion criteria,12,14,24,25,28,32,35,38 nine articles (33%) did not clearly report if AC injuries were identified in a standardized way or if the methods used for identification were valid, 7,14,31,32,35,37,38,43,44 and nine articles (33%) did not provide clear reporting of the presenting site/clinical demographic information.9,14,21–26,30 The three items with the lowest reporting were consecutive inclusion of participants (30%),7,12,21,25,35,42–44 complete inclusion of participants (14%),7,13,25,42,75 and clear reporting of clinical information (39%).22,24,26,30–32,34,36,38,39,44,75
INTERPRETATION OF THE LITERATURE
Following further review of the included studies, concerns were raised regarding a large number of methodological inconsistencies between studies. First, the surgical techniques were highly variable with fixation methods including hook plates26,27,30,33; screws or pins7,12,14,29,37–39; wire, graft, tape, or suture9,13,21–23,25,28,31,32,34,36,39; and biologic allograft.35 Second, a variety of outcome measures were used in isolation or in combination such as subjective patient ratings, subjective physician ratings, radiographic assessments, and impairment measures. Finally, a lack of robust details regarding nonoperative interventions such as specific exercises, frequency, duration, intensity of exercise, number of visits, or when to progress a patient through the program were not reported by most studies.
The variation in surgical and rehabilitation technique is likely rooted in clinical philosophies and views about how the AC joint functions as part of arm function as described above. Traditional views of injury to the AC or CC ligaments was based on restoring the disrupted anatomy from a cosmetic perspective as evidenced by the seminal injury classifications systems76,77 and the variation in surgical techniques that aimed to reduce or eliminate the disarticulated joint with various materials.7,9,12–14,21–23,25–34,36–39,39 However, more recent work has identified that AC joint injury can have profound 3-dimensional functional consequences such as alterations in SHR also known as scapular dyskinesis.24,78
Scapular dyskinesis can occur as part of high-grade AC joint injuries due to the disruption of both the AC and CC ligaments and subsequent vertical and horizontal instability and loss of optimal force and motion transfer between the scapula and clavicle.79 The disrupted scapular function is a primary component of the residual impairment reported in most studies and can be clinically observed as scapular dyskinesis.
The identification of 3-dimensional scapular dysfunction as part of AC injury led to the development of an alternative AC joint injury classification system that expands and modifies the traditional 2-dimensional Rockwood system76 by allowing clinicians to consider 3-dimensional functional consequences as part of the injury.60,80 The International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine (ISAKOS) created an algorithmic classification system that discerns the type of AC joint injury by whether or not scapular dyskinesis is present.60 This was done due to the ongoing debate that has existed regarding whether or not to operatively or nonoperatively manage Rockwood Type III injuries.1,81,82 The debate has existed because many AC joint injuries that have been classified as Rockwood Type III due to visual prominence of the distal clavicle, have complete tears of the trapezoid ligament but intact conoid ligaments. Since the Type III classification encompasses both incomplete and complete CC ligament injuries, both altered or normal scapular kinematics can exist under the same injury classification.78,83 This may be why minimal correlation of imaging and symptoms with the traditional classification systems or with published outcomes occurs.2,60,84–86 As such, injuries where partial CC ligament injury exists have been re-classified in the ISAKOS system as Type IIIA, which accounts for CC ligament involvement but without functional consequence to scapulohumeral rhythm. Those injuries with complete disruption of both CC ligaments have a greater frequency of associated scapular dyskinesis.24,78 Thus, higher grades of AC joint injury (Rockwood/ISAKOS IIIB-V) create more alterations in normal scapulohumeral rhythm, with potential for larger amounts of dysfunction due to a greater disruption of the anatomy. Considering that many articles retained in this review included Rockwood Type III injuries and that surgical techniques that simply aim to realign the clavicle with the acromion do not fully account for the 3-dimensional mechanics of the upper limb, the variation in surgical technique selection and the reported outcomes found in this review is not completely unexpected.
The most concerning finding of this review is that several of the comparative studies provided a wealth of information regarding surgical treatment yet did not provide the important details that are pertinent for analyzing the effectiveness of conservative management. In most cases, the comparison to surgical stabilization was the use of a sling with no other use or standardization of rehabilitation.7,9,12–14,21–39,42–44 Occasionally, administration of “mild” analgesics9,23,25,26,30,42–44 and application of ice9,23,25,35,43 was permitted, but dosage information was not provided. As noted earlier, when additional rehabilitation interventions that could be classified as therapeutic exercise were included such as progressive motion,9,13,21,23–31,34–38 scapular strengthening,24,26,35,44 and/or shoulder strengthening9,21,24,27–29,33–36,38,43,44 details related to the exercise parameters were insufficient or not described at all. For example, when details were provided for motion, a wide range of methods including passive, active-assisted, and active shoulder range of motion were employed yet no sets and repetitions or criteria to progress were described. In some cases, time of initiation of motion or formal rehabilitation9,13,21,23,24,26,28,31,32,34–38,44 was mentioned but rarely were all necessary program details included. This included four of the five articles that exclusively utilized nonoperative treatments.42–44,75 Furthermore, quality of evidence surrounding this topic has been described as low-quality by previous authors3 as well as the current study, and as a result, it is understandable why clinical decision-making has been difficult as to how to best manage AC joint injuries conservatively.
Using the current literature as a guide, there are two nonoperative treatment case series that provide some guidance regarding therapeutic intervention programming. First, Carbone et al.,24 described a program based on the combination of mobility, scapular strengthening, shoulder strengthening, and kinetic chain-based exercises. The program was supervised and administered by a physiotherapist a minimum of three hours per week for the first six weeks, then 1.5 hours per week until the final follow-up. Second, Petri et al.,35 described a program with similar components as Carbone et al.,24 except the program was performed two to three times per week for six weeks and it was separated into three progressive phases. Although neither program provided sets and repetitions, intensity, or criteria to progress the patient, both provide specific exercises that could be attempted, thus providing some assistance to rehabilitation practitioners. An additional resource for AC joint injury treatment program development would be the guidelines developed by Reid et al.,87 which were compiled from common interventions identified in the literature. The guidelines divide treatment into categories (acute phase, recovery phase, and return-to-sport), which follow established philosophies and reports that incorporate mobility, scapular strengthening and control, and the kinetic chain into shoulder rehabilitation.88–90
CLINICAL RECOMMENDATIONS FOR NONOPERATIVE TREATMENT
Combining the above mentioned studies24,35 as well as the authors’ clinical experience, it is believed that if the focus of treatment were to shift from cosmetic reduction of the separated acromion and clavicle to strategies that restore dynamic shoulder function via the re-establishment of scapular control, post-treatment outcomes for all types of AC joint injuries may become optimized. Rehabilitation measures may not fully realign the dissociated acromion and clavicle, depending on the amount of combined ligament disruption. Although the deformity may persist, scapular control (or lack thereof) and patient feedback can serve as useful benchmarks for determining if the outcome is acceptable. Therefore, a rehabilitation program that uses scapular control as the primary metric should be employed (Table 2).91
A focused AC joint rehabilitation program should differ from traditional general glenohumeral joint strengthening programs in several key areas. First, while seminal studies have identified exercise maneuvers that can activate high amounts of electrical activity in shoulder and scapular muscles (arm elevation to shoulder height and above, prone horizontal abduction, internal/external rotation at shoulder height, etc.) the foundational work was performed on asymptomatic individuals.92–96 It is possible that the dissociated AC articulation in both low- and high-grade injuries may not tolerate such high demand maneuvers. Second, the identified maneuvers were often performed in a uniplanar manner with the body in vertical or horizontal (prone or supine) stationary positions. Considering the scapula as a ‘link’ within the kinetic chain, these isolated maneuvers may not re-establish scapular mobility and control in the necessary motor patterns that require integrated use of the majority of the kinetic chain segments (i.e., using the legs and trunk to facilitate scapular and shoulder movement and muscle activation). Failure to incorporate the kinetic chain throughout the rehabilitation process, (i.e., both early and late phases), could lead to a less than optimal rehabilitation outcome likely due to the encouragement of inefficient or improper motor patterns.65,97–101 In some instances, the scapula and arm can be overtly dysfunctional. In these instances, minimizing the degrees of freedom via the elimination of gravity dependent positions may be necessary, such as placing the patient in a seated position.91,102 However, the authors contend that most AC joint injuries with concomitant scapular dysfunction should benefit from the incorporation of sitting or standing positions in the early phases of rehabilitation as these positions most closely mimic kinetic chain function.
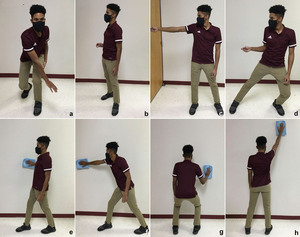
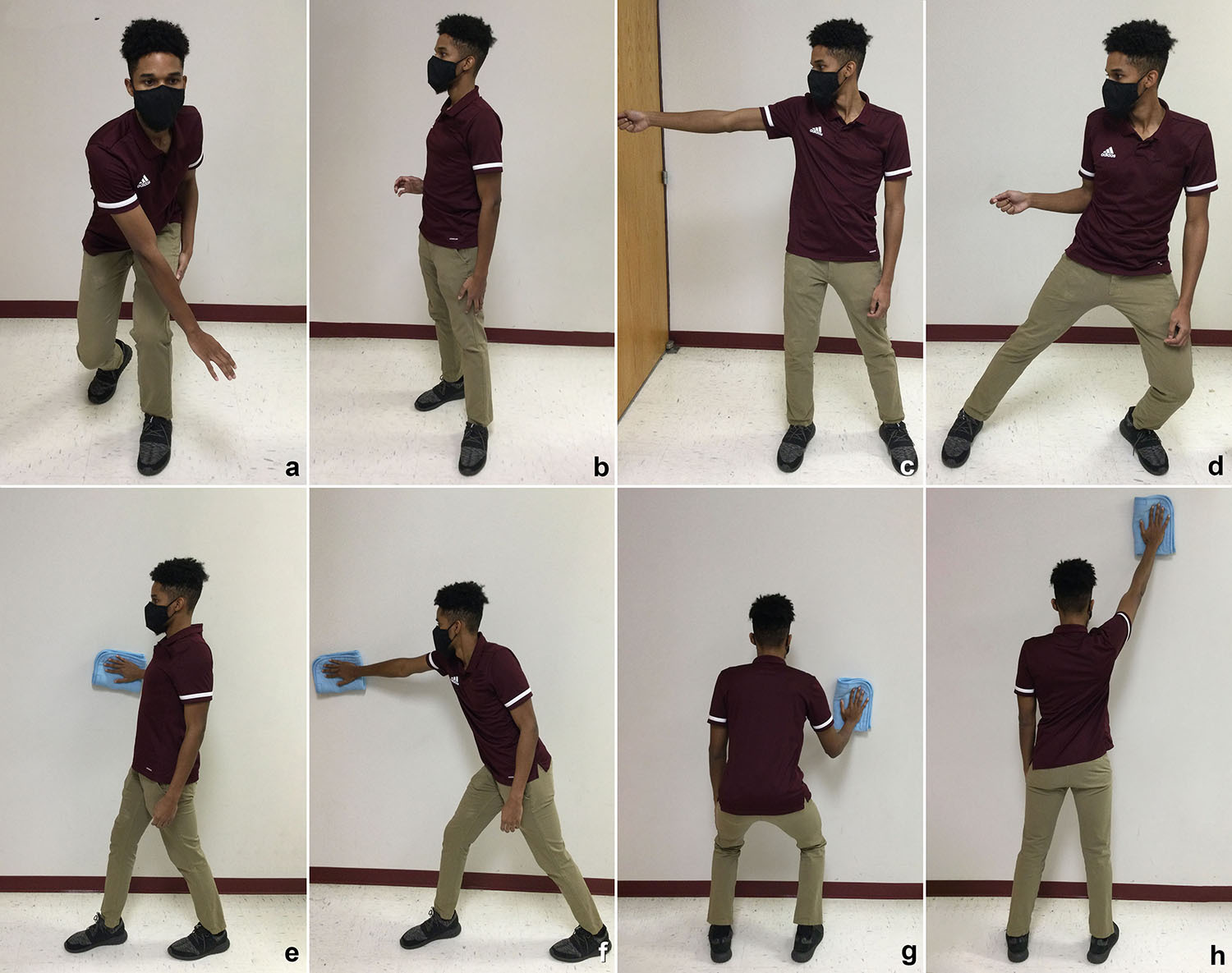
After rest and activity modification recommendations have been initiated and symptoms have been reduced (and possibly eliminated), an attempt at rehabilitation can be initiated. Physiological deficits and/or impairments (strength, flexibility, endurance, etc.) identified on physical examination may be addressed; however, a progressive program should be employed. This often begins with increasing mobility to assure the scapula and humerus move fluidly throughout arm motion (Figures 2-Figures 6). Next, avoiding maneuvers that will excessively load, stress, or move the compromised AC joint is recommended. This can be achieved using short-lever exercises that can be performed with the arms in an adducted position (i.e., the arms positioned against the thorax) (Figures 7-Figures 9) rather than positions that require the arms to be in the forward elevated or abducted positions (i.e., long-lever exercises). Examples of exercises and the rationale for their use have been provided in Table 3. Although short lever by design, maneuvers such as scapular shrugging or elevation and scapular proprioceptive neuromuscular facilitation should be avoided in the first two phases of rehabilitation (approximately the first 3-6 weeks) because of the excessive movement and stress that occurs at the AC joint during their performance. Once the patient has demonstrated that the initial exercises can be performed without exacerbating the previous symptoms, progression into more dynamic motions that require some degree of arm elevation or abduction (approximately 30-45°) may be added to the treatment progression (see short-lever and long-lever intervention examples in Table 2) (Figures 10-Figures 11). The authors suggest patients be provided an exercise regimen that begins with 1-2 sets of 5-10 repetitions with no external resistance. Additional sets and repetitions can be added based on symptoms and exercise tolerance, with a goal of 5-6 sets of 10 repetitions being able to be performed without an increase in symptoms.
Resistance may be added next beginning with light free weights (2-3 pounds maximum) and then progressing to elastic resistance. Although effective at increasing scapular muscle activity103, elastic resistance has high variability when used by patients, especially when arm position is progressed throughout a treatment program.104 Elastic resistance can be monitored and progressed when using perceived exertion scales105; however, the authors recommend beginning with free weights as those devices allow for more stability and fulfillment of isotonic contractions. Longer lever maneuvers can then be incorporated into the treatment program in the later phases of rehabilitation but only when the previous maneuvers have been mastered by the patient and have demonstrated little to no symptom exacerbation (Figures 11a-11h).
It is important to appreciate that the moderate to high degree of AC joint instability that is often associated with traumatic high-grade injuries may not achieve complete symptom resolution with rehabilitation. Muscle optimization has a ceiling effect, as the loss of skeletal stability of the scapula and clavicle and the resulting alteration of optimal SHR can be an obstacle too difficult to overcome with conservative measures. The likelihood of regaining higher degrees of function is greater in cases where only one set of ligaments has been compromised (Rockwood/ISAKOS Types I-IIIA) rather than both sets of ligaments (Rockwood/ISAKOS Types IIIB-V),1 yet it is still possible to have lingering symptoms with all types of low-grade and high-grade injuries. This confounding concern should be discussed with patients prior to initiating a conservative treatment program.
To summarize the kinetic chain-based treatment approach, the authors suggest the following as guidelines to be followed for managing AC joint injuries nonoperatively: 1) prescribe rest and activity modification as needed to decrease acute symptoms (approximately 1-2 weeks); 2) begin incorporating therapeutic exercise for addressing proximal segment control (exercises designed for leg and trunk/core strengthening); 3) employ exercises for scapular and shoulder mobility and/or lower extremity mobility as needed (mobility can be addressed simultaenously with proximal segment control interventions); 4) progress to short-lever interventions beginning with maneuvers that utilize trunk and leg motion to facilitate more optimal scapular positioning and mobility; and 5) phase out short-lever interventions and phase in long-lever maneuvers (begin with maneuvers requiring the arm to be slightly flexed or abducted then transition to maneuvers with the arm at or above shoulder height).
RETURN-TO-ACTIVITY
One of the challenges with rehabilitating the upper extremity following injury is selecting interventions that optimally prepare the patient for return-to-activity. Progression of the treatment plan for AC joint injury to higher-level/demanding exercises can be difficult due to: 1) the anatomical disruption has not been restored following supervised treatment, 2) AC joint injuries primarily occur via traumatic mechanisms and despite best efforts to prepare individuals for the risks of physical activity, traumatic events cannot be completely prevented, and 3) the literature being void of empirical studies that provide a detailed therapeutic approach and a summation of the results of that approach for its effectiveness for returning patients to activity following AC joint injury. The existing return-to-activity literature has mostly focused on the rate of return following surgical intervention with a recent meta-analysis on the topic identifying a 94% return for a variety of sports for patients who sustained a Rockwood Type III or higher injury.106 However, the authors noted that methodological heterogeneity resulted in low quality evidence for the studies retained in their review. Two recent reports centered on nonoperatively managed AC joint injury noted return-to-activity time frames ranging from three to four weeks (professional hockey players)107 and five to seven weeks (professional soccer players).108 However, the treatment details were not reported in either study and the classification of the AC injuries sustained in the soccer players was not reported.108 Due to the lack of key information surrounding treatment of the AC injuries from those works, there is a need for research aimed at identifying higher intensity sport-specific movements and exercises in athletic populations who have sustained AC joint injury.
CONCLUSIONS AND RECOMMENDATIONS
Although a number of comparative treatment studies exist for the management of AC joint injuries, the large amount of methodological differences that exist between these reports do not permit definitive nonoperative treatment recommendations to be made. Using the evidence-based medicine approach which combines the best available evidence with clinician experience and patient values, the following conclusions can be offered: 1) variation in outcomes are possibly due to using 2-dimensional AC joint alignment rather than 3-dimensional shoulder function; and 2) a treatment program that is functionally-based rather than cosmetically-based could provide nonoperative treatment guidance as it allows for dynamic scapular and shoulder motion to be addressed to optimize arm function due to the demonstrated relationship between scapular position and motion and varying amounts of AC injury. The strength of these recommendations are level B as per the Strength-of-Recommendation Taxonomy as the evidence is inconsistent in methodological design and limited in regards to treatment methods and details reported.109
Conflicts of Interest
The authors declare no conflicts of interest.

_and_the_patient_in_a_su.jpeg)
_with_the_trunk_being_actively_flexed.jpg)
_with_both_arms_.jpg)
._body_.jpg)
_and_hip_lateral_movements_to_allow_th.jpeg)
_and_being_instruct.jpeg)

_and_with_extension_of_the_hips_and_trunk_to_fa.jpg)
_with.jpg)

_and_the_patient_in_a_su.jpeg)
_with_the_trunk_being_actively_flexed.jpg)
_with_both_arms_.jpg)
._body_.jpg)
_and_hip_lateral_movements_to_allow_th.jpeg)
_and_being_instruct.jpeg)

_and_with_extension_of_the_hips_and_trunk_to_fa.jpg)
_with.jpg)