Proximal biceps pain has become increasingly prominent in the discussion of shoulder pathology and especially when associated with rotator cuff injuries and superior labrum from anterior to posterior (SLAP) lesions. Pain in the long head of the biceps (LHB) is usually inflammatory in nature and can be caused by a variety of pathologies which was well described in Sethi et al.1 LHB pathology can fall into three main categories of inflammatory, instability, and traumatic. Patients falling into any of these categories can present with debilitating anterior shoulder pain. Inflammation in the LHB can stimulate a robust sensory and sympathetic innervation in this area which contributes to the intensity of pain these patients experience. Taylor et al, have described 3 zones where the biceps can exhibit pathology and specific tests to identify these lesions called the “3 pack examination”.2
Patients that present with LHB pain fall into a bimodal distribution. Young overhead athletes and older patients with rotator cuff pathology make up the majority of the patients that present to our clinics. With an increasing number of young athletes playing year-round sports, biceps pathology is a common complaint in our clinics. In a different mechanism, our older patients suffer from subacromial impingement and rotator cuff tears that cause increased stress on the LHB. We believe the LHB becomes a significant humeral head depressor in the setting of a large rotator cuff tear which contributes to this presentation. Although controversy exists regarding the function of the long head of the biceps brachii.3
Treatment options for proximal biceps tendon pain should often start with non-operative treatment and the treatment modalities are dictated by the etiology of the biceps pathology. Wilk et al, have described six different proximal biceps lesions and specific treatment approaches for each.4 For an inflammatory process, (i.e., biceps paratendinitis) activity modification, anti-inflammatories and other modalities have all been used successfully. Laser therapy and iontophoresis can also be beneficial in this setting. In addition, a rehabilitation program which emphasizes scapular muscle strengthening, postural correction and rotator cuff strengthening is critical. With biceps tendonosis, non-operative treatment focused on increasing circulation and promoting healing is focused. This includes, heat, soft tissue mobilization, piezo wave therapy, laser, eccentric exercise, and a scapular & rotator cuff strengthening program while avoiding NSAIDs and ice to create a healing environment.
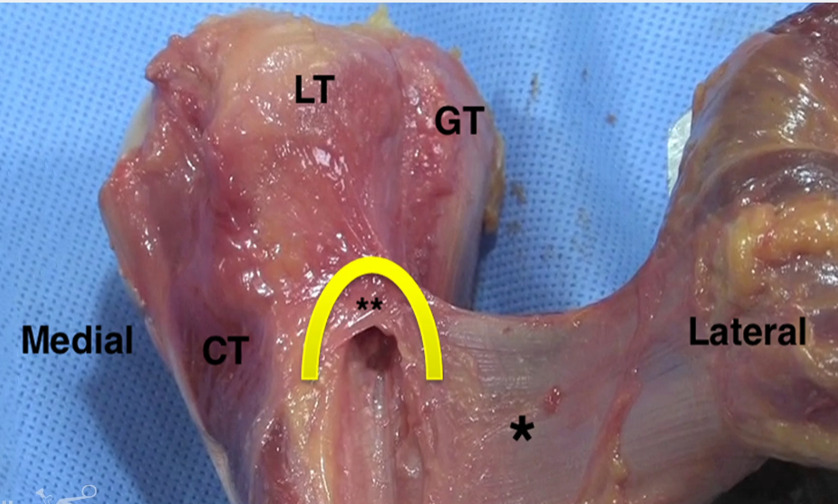
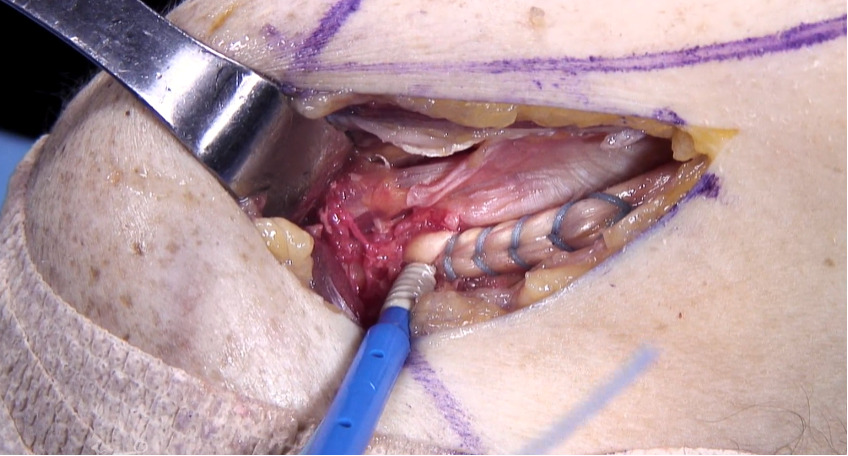
When non operative treatments have failed to give the patient adequate relief and function, surgical intervention can be considered. If surgery is elected, the surgeon may perform a tenotomy, or a biceps tenodesis (either supra-pectoralis or sub pectoralis location). At our institution, we perform all sub-pectoralis biceps tenodesis. We believe this gives the advantage restoring proper tendon tension and length and avoidance of the “Popeye” deformity that is seen with a tenotomy alone.5 Tenotomy can lead to painful muscle spasms as it retracts into the arm. The location of the tenodesis is at the level of the pallium pectoralis. This is a consistent fascial sleeve that extends from the superior boarder of the pectoralis major tendon to the humerus which lies in the metaphyseal-diaphyseal junction of the humerus. This location is ideal since it avoids the risk of fracture when placed in the diaphysis and is also inferior enough to avoid insertion into the humeral head. After cutting the biceps tendon intraarticularly in the joint just above its labral attachment, a longitudinal 3 cm incision is made just inferior to the palpable boarder of the pectoralis major tendon. We use the Birmingham Biceps Technique that uses a 5.5 SwiveLock PEEK screw (Arthrex) to secure the tendon using a Fiberloop suture. Of note, at our institution we do use smaller anchors in high level throwing athletes to avoid the risk of humerus fracture while throwing. A measuring device is used to ensure that the most proximal extent of the tendon that is whipstitched is 4 cm from the musculotendinous junction of the LHB. The screw is inserted into the bicipital groove at the level of the pallium pectoralis which ensures adequate tension. This avoids a “Popeye deformity” as well as retains anatomic muscle/tendon length with the correct anatomic force vector on the tendon. We believe that this technique removes the biceps tendon from the bicipital groove which is a common source of pain. This location places the anchor out of the diaphyseal portion of the bone to reduce post operative fracture risk.
Clinical photographs detailing the subpectoralis LHB tenodesis is shown in Figures 1-5.6
The post operative rehabilitation includes that the patient is instructed not to lift any heavy objects overhead and avoid activation of the biceps in the immediate post operative period. No isolated biceps strengthening exercises for 6-8 weeks post operatively. The rehabilitation can be broken down into 3 phases. Phase 1, is the immediate motion phase weeks 0-2 which our goal is to re-establish non-painful range of motion, retard muscular atrophy, re-establish dynamic stabilization, and decrease pain and inflammation. During phase 1 the patients begin with pendulums and rope and pulley. They will progress to full elevation range of motion and initiate external and internal tubing at 30 degrees of abduction in the scapular plane by the end of phase 1. Exercises focused on rotator cuff and scapula posture are emphasized.
Phase 2 is completed from weeks 2 through 6. The goals of this phase are to regain and improve muscular strength, normalize arthrokinematics, improve neuromuscular control of the shoulder complex, and continuing to diminish pain. Before beginning phase 2 The patients must have full range of motion, minimal pain, and have progressed well with internal/external rotation at 0 degrees of abduction. The goal by the end of phase 2 is the have the patient normalize their arthrokinematics with the use of L-bar range of motion and be able to achieve normal internal and external rotation at 90 degrees of abduction. During this phase, scapular strengthening exercises, postural correction drills and a shoulder strengthening program is utilized. Strengthening exercises focus on dynamic stabilization, and scapular synchronization with active movements.
Phase 3 is the dynamic strengthening phase and consists of weeks 6-12. The goals of this phase are to improve strength, improve neuromuscular control, and prepare patients to return to sport if applicable. To enter phase 3 of rehabilitation patients must have full non-painful range of motion, no pain, and strength at 70% of contralateral extremity. During this phase all exercises are progressed, biceps strengthening is initiated, but more functional exercises are utilized during this phase.
Phase 4 consists of more maintenance and the progression of strength and range of motion. The patient is instructed to continue their ROM exercises and any capsular stretches as needed to avoid any post operative capsular tightness. For athletes, plyometrics can be initiated beginning with 2 handed and progressing to 1 handed plyometrics. We will initiate a gradual return to sport at approximately 12 weeks. Rehabilitation concludes with gradual return to all unrestricted functional activities.4
The outcomes of LHB tenodesis are favorable across all age groups and activity levels. A study currently in review from American Sports Medicine Institute examined 76 softball players and compared results of SLAP repair versus biceps tenodesis. This study revealed no statistical difference between these groups in return to play rates as well as pain and function. This data would suggest a biceps tenodesis is a reasonable option with similar results and shorter follow up time than SLAP repairs for collegiate level throwing athletes.7 An additional study by Griffin et al., demonstrated a satisfaction rate of 40% for SLAP repairs versus 93% for biceps tenodesis in patients under 25 years of age with SLAP tears.8 In Ek et al., they showed favorable results in patients older then 35 undergoing biceps tenodesis.9 LHB tenodesis has reliable results across age groups and activity levels.
LHB tenodesis by the technique listed above has given us a safe and reliable way to treat patients who have failed non-operative management. Our technique has given us excellent results in patients of all ages including younger overhead athletes. This technique also avoids the problem of cosmetic deformity as well as muscle spasm and pain that some patients experience with a tenotomy alone as discussed in Hsu et al. Tenodesis also has the added benefit of increased flexion and supination strength compared with tenotomy alone.5 Our use of anatomic landmarks and placement of the anchor ensures that we have reduced risk of fracture with adequate tension maintained in the musculotendinous unit. Placing the anchor in the anatomic location of the more distal portion of the tendons normal position also maintains proper tendon vector that is consistent with native anatomy.