INTRODUCTION
Shoulder range of motion deficits often arise from various shoulder pathologies and occur in multiple planes.1–5 Patients with signs consistent with general shoulder pain, including internal impingement6,7 or superior labral pathology2 commonly have associated loss of both internal rotation and horizontal adduction.2,6 This common physical limitation in patients with shoulder pain necessitates that interventions are utilized to effectively improve shoulder range of motion, pain, and function.
Assessment and treatment of shoulder mobility is critical to improved patient outcomes as many diagnoses have identified shoulder mobility deficits as a common impairment. Two recent clinical reasoning algorithms for managing patients with shoulder pain recommend that shoulder soft-tissue limitations be assessed and treated to effectively manage these patients.8,9 Morrison recommends treating mobility deficits prior to strength deficits in patients with rotator cuff impingement.3 Several interventions, such as the sleeper stretch, the cross-body stretch, and joint mobilization have demonstrated increased shoulder mobility in individuals with posterior shoulder tightness.10–14 Recently, Salamh et al.12 investigated the immediate effects of scapula stabilized vs. non-stabilized stretching in volleyball players with tight posterior shoulder tissues and found that scapular-stabilized stretching was most effective. A common limitation of these studies is that they were conducted on healthy individuals with posterior shoulder tightness, creating a paucity in the literature to support the use of these stretching interventions in patients with shoulder pain.
Stretching interventions combined with other interventions have been successful improving mobility,6,13–15 function,6,13–15 and pain13,14 in patients presenting with symptoms of internal impingement and mobility deficits. Multi-modal interventions of stabilized scapula stretching, joint mobilization, and scapular strengthening have demonstrated improvements in mobility, function and pain reduction over the course of three to seven weeks.6,15 Patients with rotator cuff tendinitis who do not receive therapy for a month have shown no improvement in the same measures, indicating that no treatment does not seem to resolve symptoms.4 Multi-modal interventions are effective yet limit our understanding which intervention affects a particular impairment.
There is limited evidence to demonstrate that patients with a painful shoulder who seek medical care can benefit from an intervention focusing primarily on posterior shoulder stretching alone to positively impact range of motion, pain and function. Limited evidence exists on the effect of stretching with scapula stabilized compared to non-stabilized in a population with shoulder pain. The aim of this study is to determine the effect of stabilized scapular stretching on patients with shoulder pain. Therefore, the primary hypothesis of this study is that stabilized scapular stretching will improve glenohumeral motion and pain compared to non-stabilized stretch program. A secondary hypothesis of this study is that stabilized scapular stretching will produce greater improvement in function compared to the non-stabilized stretching program.
Methods
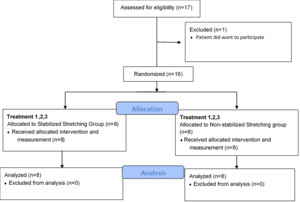
A single-blinded randomized clinical trial was used to compare two shoulder stretching techniques performed over the course of three treatment sessions in patients with shoulder pain (Figure 1).
Subjects
Potential participants were recruited between June 2015 and July 2017. A total of 16 patients with shoulder pain were enrolled in this study that were seeking treatment at the Howell Rehab Centers outpatient physical therapy clinic for shoulder pain. Informed consent was obtained for all participants in accordance with the procedures approved by the University of Kentucky Institutional Review Board prior to participation in the study. All of the participants were screened by a licensed physical therapist and excluded from participating if reporting pain originating from peripheral neurological disorder (such as cervical radiculopathy or thoracic outlet syndrome), determined to have adhesive capsulitis defined as range of motion limitation in external rotation or elevation of 50% or more compared to the uninvolved side, pain greater than or equal to 8/10. Patients with a history of shoulder surgery in the last three months were excluded. Patients were included in the study if shoulder pain was provoked with active, passive or resistive testing of shoulder elevation, external rotation or internal rotation regardless of pain duration or source of pain. Patient’s referring physicians were primary care and sports orthopedic surgeons and the patients had the following referring diagnoses: rotator cuff tendinopathy (n=10), non-specific shoulder pain (n=4), superior labral pathology (n=1), and acromioclavicular joint sprain (n=1).
Patients were randomly assigned to one of two stretching groups: stabilized scapular stretching (n=8) or non-stabilized scapular stretching (n=8), using a block randomization process. The physical therapist was blinded until all initial assessments and measurements were completed. An opaque envelope was opened to indicate treatment assignment. The patient was blind to group membership as all patients were given a stretching intervention. No differences in baseline measures as determined by independent T-test and Chi-square analysis except for horizontal adduction (Table 1).
A priori power analysis was performed using Nquery Advisor 7.0 (Statistical Solutions, Ltd, Boston, MA) using previous data of stabilized vs non-stabilized horizontal adduction range of motion.12 A sample size of 12 in each group would have 80% power to detect a mean difference of 18° assuming a common standard deviation of 15° using a two sided independent t-test with a p = 0.050. These differences were calculated to have an effect size of 1.2.
Measurement Procedures
During the initial visit, measurements were taken bilaterally; subsequent assessments were only taken on the symptomatic side. The physical therapist was blinded to the results using a two-person assessment to minimize bias. A digital inclinometer (Baseline Digital Inclinometer, White Plains, NY) was used to measure all motions described below. The physical therapist and assistant performing all measurements’ reliability was evaluated and found to be excellent. ICC’s ranged from 0.87 to 0.99 with minimal detectable changes with 90% confidence interval ranging from 2° - 4° for all measurement which is consistent with previous research.16,17
Non-stabilized passive flexion was measured with the patient lying supine, and their arm passively elevated in the sagittal plane to the point of pain or resistance, whichever came first. The angle between the arm relative to the horizontal surface of the plinth was recorded. The patient was not allowed to arch their back ensuring that their trunk was in line with the table.
Stabilized supine passive flexion was measured in the same manner except that the physical therapist stabilized the lateral border of the scapula with the heel of their hand before passively elevating the patient’s arm into flexion.
Stabilized supine horizontal adduction was measured with the patient lying supine.17,18 Their arm was abducted to 90° and elbow flexed to 90°. The physical therapist blocked the lateral border of the scapula with the heel of their hand before passively elevating the patient’s arm transversely across their chest into adduction to the point of pain or resistance, whichever came first. The inclinometer was zero referenced perpendicular to the plinth such that if the humerus was pointing directly toward the ceiling that would be zero degrees. Measures less than vertical were recorded in negative degrees and measurement angles greater than zero degrees were recorded as positive values (Figure 2).7,18,19
Stabilized supine internal rotation was measured with the patient lying supine. The patient’s arm was abducted to 90° and elbow flexed to 90°. The physical therapist blocked the scapula anteriorly over the coracoid process and clavicle to prevent scapular substitution. The patient’s forearm was passively rotated forward toward the table in the sagittal plane to the point of pain or resistance with the scapular stabilized by the physical therapist. The inclinometer was zero referenced as described previously. The angle between the forearm relative to the horizontal surface of the plinth was recorded using a digital inclinometer (Figure 3).
All measurements were taken in the same manner before and after each treatment intervention for the three sessions of treatment, as was reported level of pain, using a numeric pain rating scale from 0= no pain to 10= worst possible pain. Single measurements were recorded as all data were collected in an outpatient clinic by the therapist during the standard course of patient care. It was not feasible or consistent with the standard of care to take multiple measurements. The physical therapist had 30 plus years of experience and excellent reliability outcomes supports this measurement approach. It was not feasible to blind the treating physical therapist from group membership as this was a single physical therapist practice. The physical therapist was blinded to measurement values by performing the passive movements while an assistant would zero and align the inclinometer to the humerus, to minimize evaluator bias. Data were recorded by the assistant on the data collection form and recorded in the chart. Measurements were not seen by the physical therapist until the patient had left to attempt to minimize bias.
Prior to the initial evaluation and following the final treatment visit, patients were asked to complete the Penn Shoulder Score, a self-reported measure of shoulder function, pain, and satisfaction.20 The Penn Shoulder Score total score ranges from 0-100 with 100 indicating no pain, full satisfaction and normal function. The retest reliability of this self-reported functional outcome tool has been found to have an ICC with 95% confidence interval of (.89-.97) with a minimal clinically important difference at a 90% confidence interval of 12.1 points.20
Stretching Intervention
All patients regardless of group, received high voltage pulsed (galvanic) electrical stimulation prior to stretching. The bipolar electrodes were placed on the anterior and posterior aspect of the shoulder with a dispersive pad placed over the lumbar spine with the parameters set at 80 pulses per second for 20 minutes. The intensity was set to the point of a strong sensation but no muscle contraction in order to facilitate the gate control theory of pain management.21 After all patients completed the electrical stimulation treatment, they were split into their designated groups: stabilized or non-stabilized scapular stretching intervention.
Stabilized Scapular Shoulder Stretching
The patient was lying supine for all stretches. The treating physical therapist had the patient perform 10 repetitions of passive shoulder flexion in the supine position with the scapula manually stabilized on the lateral portion to restrict scapular motion to focus stretch on scapulohumeral tissues. The patient performed a self-stretching technique by slowly lifting arm overhead into shoulder flexion to the point of tightness but with no pain using their opposite arm or stick to perform the passive motion. The therapist reminded the patient to stop stretching shoulder into flexion right before the point of pain. The patients held this position for five seconds and then relieved the tension by lowering the arm back to neutral. The treating physical therapist re-applied manual stabilization to the scapula, as needed, during the 10 repetitions to minimize scapular motion. This procedure of stabilized scapular self-stretching was repeated in the transverse plane for horizontal adduction. The patient was instructed to slowly pull their humerus across their body with their elbow flexed to the point of tightness but again not to induce any shoulder pain while the physical therapist applied resistance to the lateral scapular border to minimize scapular motion. Passive shoulder internal rotation at 90° of abduction was performed with use of a stick while the physical therapist stabilized the scapula anteriorly over the acromion and coracoid to prevent anterior tilting. The stretching parameters for duration and frequency were the same for all of 10 repetitions with five second holds below the pain threshold.
Non-Stabilized Shoulder Stretching
The patient was lying supine for all stretches with direct supervision of the treating physical therapist. All stretching parameters were exactly the same as described above without the scapula being blocked. The patient was still instructed to perform self- stretching exercises and stop prior to inducing pain while holding for five seconds.
Post-intervention measurements occurred immediately after stretching routine was completed and followed the same procedures as described previously. After, all patients received 15 minutes of cryotherapy using a commercial cold pack with toweling placed between the skin and cold pack with a wrap securing the position. The participants returned for two more sessions based on the participant’s schedule and treating physical therapist’s schedule. Patients are typically seen two-times per week. The average duration was 9 days (range 5-17 days) to complete the study.
Home Exercise Program
Patients were instructed in-home exercises of shoulder flexion and internal rotation three times per day for 10 repetitions with a three-second hold for each stretch. Both groups were given the same home program. Shoulder flexion was performed with the assistance of the opposite arm or with a stick. Shoulder internal rotation was performed with the assistance of a towel either pulling across their back or up their back to induce a non-painful stretch. Each participant was given a home exercise log to monitor adherence to program and asked to return at the end of the study. Self-reported compliance was 85% in the stabilized group and 92% in the non-stabilized group resulting in no difference between the groups (p=0.58).
Statistical Analysis
The data was examined for normality using a Shapiro-Wilks test and found to be normally distributed. A fixed two factor linear mixed model analysis was performed with significance set at (p<0.05). The fixed factors were group (stabilized group and non-stabilized stretching groups) and time (pre and post measurements for the three visits). The dependent measures were the four range of motion measures and current level of pain. The same mixed model analysis for the Penn Shoulder Scores was carried out but with only two time points pre-intervention on Day 1 and post-intervention on Day 3. If a significant interaction between group and time were observed Bonferroni post-hoc analysis was carried out with significance set at (p<0.05). IBM SPSS Statistics for Windows (Version 23.0; Armonk, NY; IBM Corp.) was used to analyze the data.
Results
Significant interactions between group and time were found for three of the four range of motion measurements indicating that the stabilized group improved more: stabilized flexion (Figure 4, p<0.001), stabilized horizontal adduction (Figure 5, p<0.001) and stabilized internal rotation (Figure 6, p < 0.001). Bonferroni post-hoc analyses correcting for multiple comparison reduced the critical value (p ≤0.008). For both stabilized flexion and stabilized horizontal adduction, measures at post-treatment visit 1 through post-treatment visit 3 were found to be both significantly greater and beyond measurement error in the stabilized group compared to the non-stabilized group (Figures 4 and 5). Stabilized internal rotation measures at post-treatment visit 1 through pre-treatment visit 3 were found to be significantly greater and beyond measurement error in the stabilized group compared to the non-stabilized group (p<0.008, Figure 6).
Only non-stabilized flexion did not have a significant interaction (p = 0.38) but demonstrated a significant main effect of greater motion in the stabilized stretching group (164° CI95 157°,171°) compared to the non-stabilized stretching group (150° CI95 142°,158°) (P= 0.033). There was a main effect for time, indicating that regardless of group membership non-stabilized shoulder flexion increased over time. A Bonferroni post-hoc analysis for multiple pairwise comparisons with an adjusted critical value of (p ≤0.003) for time revealed that at final post-treatment visit 3 measure of non-stabilized flexion (164° CI95 157°, 171°) was found to be greater than the first three measurements (Table 2).
Current pain level analysis revealed a significant interaction between group and time (p =0.026) (Figure 7). Post-hoc analysis was performed with pairwise comparisons using a Bonferroni correction for multiple comparisons adjusting the critical value to (p ≤0.008). Pairwise comparisons between groups did not reach this level of significance at any time point.
The linear mixed model ANOVA for the Penn Shoulder Score total score did not reveal a significant interaction between group and time (p =0.64). However, there was a main effect for time, indicating that both stretching groups significantly improved the Penn Shoulder Score total score. The baseline Penn Shoulder Score was 56.3 (CI95 47.3, 65.4) and progressed to 73.0 (CI95 64.5, 81.5) at the end of treatment. (p <0.001), surpassing the minimally clinically important difference.
Discussion
Stabilization of the scapula during stretching improved mobility in patients with shoulder pain in three of the four directions evaluated compared to patients without scapular stabilization. This supports the primary hypothesis that stabilized scapular stretching is more effective than non-stabilized scapular stretching in restoring passive shoulder mobility. However, the hypothesis that stabilized scapular stretching would reduce pain more than non-stabilized stretching was not supported. Based on previous literature, an improvement of 9 degrees in shoulder ROM is determined to be clinically significant.16 Significant and clinically meaningful changes in passive shoulder mobility and function, following pain-free stabilized scapular stretching and simple home program, were achieved in 5-17 days. These results support the concept of re-establishing normal shoulder mobility initially in the rehabilitation process.3,9
Interventions to improve Posterior Shoulder Mobility
Posterior shoulder stretching to improve mobility is well-established.6,10–12,14,15,22–24 However, most research has focused on stretching subjects that had restricted shoulder mobility without shoulder pain. Three previous studies have examined the stretching effect on posterior shoulder tightness (PST) in symptomatic patients.6,14,15 Posterior shoulder mobility improved over the course of multiple visits across three to seven weeks using a multi-modal approach of stretching, strengthening and educational techniques.6,15 The current study focused on only stretching interventions to improve mobility, pain, and function in three visits across nine days on average.
A multimodal approach to treating (PST) in patients with shoulder pain improves mobility and function,6,14,15 however, determining which intervention caused what effect can be difficult to ascertain. Tyler et al.,6 enrolled 22 patients with posterior impingement into an prospective cohort study of physical therapy three times per week, including daily home exercises that included stabilized scapular stretching, joint mobilizations, self-stretching, and shoulder strengthening. The interventions demonstrated significantly increased horizontal adduction by 28 ± 22° and internal rotation by 26 ± 20°.6 These improvements are comparable to the current study which was achieved in three treatments. Cools et al.,15 undertook a similar study enrolling thirty competitive overhead athletes with impingement signs and posterior shoulder tightness. Patients were randomized into either glenohumeral joint mobilization or scapula stabilized stretching. Each group underwent 30-minute treatments, three times per week for three weeks. Half of each treatment focused on scapular stabilized cross body stretching and half on sleeper stretch while the joint mobilization group spent half of their time on posterior and inferior mobilization interventions.15 No differences were seen between groups, but both groups saw improvement of passive internal rotation (12 ± 10°).15 Tahran et al.,14 explored the difference between modified cross-body stretching and modified sleeper stretching in combination with therapeutic exercise on subjects with impingement signs and GIRD, compared to a control group only receiving the therapeutic exercise over 20 treatment sessions. No significant difference was found between stretching groups, improving internal rotation by 22 ± 9°.14 Unfortunately, weekly measurements were not captured in these studies so it is unclear when these changes occurred. It is possible that changes occurred early as seen in the current study but were just not recorded.
The effectiveness of scapular stabilization versus no scapular stabilization during stretching was observed after a single treatment intervention and progressed over the three visits spanning a mean of nine (range 5-17) days. These changes occurred earlier than in previous reports.6,14,15 Potential explanation for the large and early increase in mobility may be due to the stabilized stretching in three differing planes of motion. The therapists in comparable studies stabilized cross-body adduction in similar manners,6,14,15 internal rotation using the plinth6,14 or therapist hand15 but neither intervention incorporated scapular stabilized flexion stretching, which may target different portions of the posterior soft tissue that were restricting motion accounting for the dramatic improvement. The large change in range of motion may be due to the current subjects having a larger mean deficit in internal rotation at baseline, measuring 10° less than Tyler et al.6 and 30° less than Cools et al.15 and Tahran et al.,14 allowing for greater change in motion to occur.
Three of the four motions were positively affected by stabilized scapular stretching with the exception in the non-stabilized flexion, which improved in both groups. Stabilized scapular stretching during flexion targets scapulohumeral tissues while non-stabilized flexion allows the scapula to move therefore stretching multiple tissues in the shoulder region. Both groups performed non-stabilized flexion at home at a similar adherence rate which may account for lack of differences observed in this measurement.
Dosing Parameters and Mechanism
Dosing parameters and effectiveness is varied in previous research. The current study used a dosing parameter of ten stretches, holding for five seconds, in three planes of motion for a total stretching time of 150 seconds. A systematic review of the effectiveness of stretching on PST demonstrated that interventions for PST have stretching parameters that range from ninety seconds to fifteen minutes in healthy populations with posterior shoulder tightness.25 Previous research focusing on duration parameters in hamstring muscles identified thirty seconds as an optimal stretch duration.26 However, applying a passive stretch of fifteen seconds or for two minutes did not demonstrate significant improvements in hip abduction range of motion.27 Stretch duration research has predominantly been studied in patients without pain. In this study’s results suggest short duration holds repeated 10 times in multiple planes were effective to improve motion in a painful population. Connective tissue restrictions of both musculotendinous and capsular structures in the shoulder have been implicated as a mechanism causing shoulder pathologies and altering shoulder joint arthrokinematics.28–30 As this was a clinical study, the authors were unable to discern if the adaptations were muscular or capsular but likely muscular due to early changes. Stretching and soft-tissue mobilization have demonstrated reduced muscular stiffness31 but the viscoelastic changes are temporary and baseline measures return within an hour.32 In the current study changes occurred during treatment and were maintained between treatments beyond the reported viscoelastic affects. Neurophysiologic changes may attribute to range of motion gains as static stretching has been shown to minimally decrease the time required for an H-reflex through diminished motor neuron pool excitability promoting increases in muscle extensibility.33 However, these results were determined from single stretching sessions and current research utilizing long-term protocols have determined no significant neurological adaptations to repeated stretching.34 Therefore, another explanation for these results is due to increased tolerance to stretching.32,34–36 Perhaps through the short yet repetitive stretching performed, tolerances improved in this study, accounting for the improved measures. Proposed mechanisms of increased range of motion following stretching include increases in elasticity of connective tissue and myofibrils, neurophysiological effects, and increased tolerance to stretching.31,32,34,35
Function and Pain improvements not due to stabilized scapular stretching
Patient reported outcomes are critical measures of patient improvement as they evaluate patient’s perception of function and pain. Direct comparisons between studies was not feasible due to frequency of measurement and tools used. To compare the current results to others the percent improvement in the functional score per visit was calculated. The current study had a 12%/visit improvement in function over three visits, as measured by the Penn Shoulder Score, and was most similar to Tyler’s results, a 6%/visit improvement in function over 21 visits.6 It is likely that other studies have similar or perhaps greater improvement but were not measured as frequently.6,14,15,37 Early changes in perceived function have been seen in previous research and is a strong indicator of successful intervention.37,38 In the current study both stretching groups improved with most of the change occurring in the function component of the Penn score. The increased mobility may have allowed patients to perform functional tasks easier accounting for the perceived improvement.
Prior to and following each treatment day pain was measured with a numeric pain rating scale. Previous research has found that two points represents a clinically meaningful change in pain.39 Pain demonstrated a significant interaction but the clinical meaningfulness of a one point change should be questioned (Figure 7). The study duration was short and focused on mobility potentially explaining these findings. The relatively low self-report of current pain level and low number of subjects may also account for the lack of difference. It is also reasonable to interpret this finding that stretching alone does not reduce shoulder pain. Multimodal interventions have shown 30% reductions in pain.6 However, any study without a control group, cannot rule out that pain reduction did not occur naturally over time.
Limitations
An obvious limitation of this study is the small sample size. The a priori power analysis estimated that 12 subjects in each group would be needed to achieve at least 80% power. However, the authors were only able to recruit a total of 16 subjects (8 in each group) over a two-year recruitment process. The estimated effect size used in the original power analysis was 1.2 based on an 18° difference comparing stabilized and non-stabilized stretching interventions to gain horizontal adduction.12 Effect size was calculated after visit 1 (time point 2) and after visit 3 (time point 6) to compare observed versus estimated effect sizes (Table 3). The average effect size was 2.6 which is twice as much change as would have been expected with a fully powered study. A post-hoc power analysis using this new effect size of 2.6 resulted in an achieved power of 99%. Based on the time spent recruiting, and that stabilized scapular stretching was the standard clinical procedures in the clinic where the study took place, the study was discontinued even though it was underpowered. The statistical analysis supported this decision as greater changes were observed in motion using the stabilized stretching intervention for three directions measured.
Another limitation is that this study was performed in a single privately owned physical therapy clinic which reduces the external validity as other clinicians may not have the same technique. The clinician has over 30 years of experience and has used this technique in multiple patients with a positive response. This potentially biases the study as the clinician was interested in the effectiveness of this approach. However, the clinician was willing to expose his patients to another treatment approach of non-stabilized stretching during the course of his typical clinical practice. The implication of this treatment intervention is that it was applied to patients seeking physical therapy for shoulder pain in a clinical environment which enhances its external validity to patients seeking medical care. The therapist was not completely blinded from the data as he documented patient records after care was provided. The inclinometer was recorded by an assistant to minimize bias, but it is possible that the same force applied was not consistent between groups as the therapist was aware of group membership. No long-term follow up to measure motion following the intervention was carried out. Cools et. al.15 demonstrated that range of motion gains were maintained at three weeks following a multimodal intervention approach. The current study was only carried out for three treatments to evaluate immediate effects of a specific stretching intervention on mobility, pain, and function. Follow up assessment was not feasible as other treatment interventions were applied to all patients as determined appropriate by the therapist following the third visit.
Conclusion
Re-establishing normal pain free mobility is a common goal in shoulder rehabilitation and typically precedes re-establishment of strength and function. The results of this study indicate that patients in with shoulder pain that have range of motion deficits benefit the most from stabilized scapular stretching addressing internal rotation, horizontal adduction, and flexion. The results of the current study further indicate that improvements can be observed after a single treatment and can be maintained between visits with a home stretching program. Function was improved with both approaches. Pain improved in the stabilized scapular stretching group but did not reach clinical significance in this short duration intervention.
Statement of IRB Approval
This study was approved by the University of Kentucky Institutional Review Board: 15-0223-P1H
Financial Disclosure
The authors affirm that they have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript, except as disclosed in an attachment and cited in the manuscript. Any other conflict of interest (ie, personal associations or involvement as a director, officer, or expert witness) is also disclosed in an attachment.